|
Get Citation
|
|
|
Aqil N, Nassiri A, Baybay H, Douhi Z, Elloudi S, Mernissi FZ. Erythroderma: A clinical and etiological study of 92 patients. Our Dermatol Online. 2019;10(1):1-6. |
|
|
Download citation file:
|
Erythroderma: A clinical and etiological study of 92 patients
Niema Aqil, Aicha Nassiri, Hanane Baybay, Zakia Douhi, Sara Elloudi, Fatima Zahra Mernissi
Department of Dermatology, Hassan II University Hospital Center, Fes, Morocco
Corresponding author: Dr. Niema Aqil, E-mail: niemaaqil90@gmail.com
Submission: 24.06.2018; Acceptance: 05.08.2018
DOI:10.7241/ourd.20191.1
ABSTRACT
Background: Ery throderma is a rare and severe dermatological manifestation of a variety of diseases. It is usually difficult to find the underlying cause. This is a dermatological emergency that can be life-threatening.
Objective: study aimed to examine the causes, as well as the clinical and laboratory profiles of patients with erythroderma in our department.
Methods: This retrospective study was carried out in the Department of Dermatology of CHU Hassan II of Fez. Between January 2013 and May 2017. We included all patients hospitalized for acute or chronic erythroderma
Results: During the study period, 1700 patients were hospitalized in the Department of Dermatology. Erythroderma was diagnosed in 92 patients (5.41%), corresponding to an incidence of 20 cases/year. The average age was 49.6 years with a male to female ratio of 0.70. The average duration of evolution was 259 days. Erythroderma was dry in 82.6% of cases. Inflammatory anemia was found in 10.9% of patients. Eosinophilia in 44.6% of patients. Hepatic cytolysis and hyponatremia in 12.9%. Kidney failure in 18.3%. The most common cause of erythroderma was exacerbation of pre-existing dermatoses (43.5%), including psoriasis (27.2%), eczema (7.6%), pemphigus foliaceous (6.5%) and pityriasis rubra pilaris (2.2%). Followed by drug reactions (38%) dominated by the drug reaction with eosinophilia and systemic symptoms syndrome (30.4%). Cutaneous T-cell lymphomas constituted 15.2% of the causes of erythroderma. The evolution was good in 87% of the patients, whose methods of management were based on symptomatic measures in association with the etiological treatment.
Conclusion: Erythroderma is a severe dermatological syndrome of various etiologies. Drug inducederythroderma is a very important entity to know. Indeed, its early diagnosis allows a fast and adequate care thus improving the prognosis of this entity.
Key words: Erythroderma, Etiologies, Department of dermatology
INTRODUCTION
Erythroderma or exfoliative dermatitis is a rare skin disorder that may be the result of many different causes. It represents an extreme state of skin irritation involving the whole or most of the skin surface. Because most patients are elderly and skin involvement is widespread, the disease implies an important risk to the life of the patient. The causative factors can be grouped as previous dermatoses, drug reactions, malignancies systemic diseases, infections and idiopathic disorders The four more common causes of idiopathic protracted erythroderma are probably atopic dermatitis of the elderly, intake of drugs overlooked by the patient, pre lymphomatous eruptions and occult malignancies [1,2]. Histopathology can help identify the cause of erythroderma in up to 50% of cases, particularly by multiple skin biopsies [3]. Many chronic dermatoses may be histologically indistinguishable in erythrodermic patients [4].
To date there are no published studies on the frequency of underlying causes of erythroderma from our country. In order to delineate the salient features of erythroderma in our region, we have reviewed the cases of erythroderma examined and treated in our department between 2013 and 2017 (four-and-a-half-year period). Our study aimed to examine the causes, as well as the clinical and laboratory profiles of patients with erythroderma in our department. Finally, our data are discussed and compared with previously published series.
MATERIALS AND METHODS
We conducted a retrospective analysis of the clinical and laboratory profile of all patients with erythroderma admitted to the Dermatology and Venereology Department of Hassan II University Hospital Center of Fez Morocco, between January 2013 and May 2017. Our department is one of the largest dermatology teaching units in Morocco, integrated in a tertiary referral hospital in the central region of the country. All the patients diagnosed with erythroderma had developed erythema involving more than 90% of the body surface area. Due to the risks that erythroderma implies for the patient’s life and to study the cause in each case, they are always treated as inpatients. The records of these patients were carefully reviewed and the data recorded was personal data, past medical history (including history of skin diseases), drug consumption history, previous episodes of erythroderma onset and clinical data during the episode (pruritus, cutaneous signs, nail involvement, temperature, presence of edema, lymphadenopathy and visceral enlargement). Laboratory investigations including complete hematological parameters, serum electrolytes, liver and kidney function tests. electrocardiography, and chest radiography were performed for all the patients as a routine in the dermatology ward of our hospital. Whenever indicated, further investigations such as skin biopsies, lymph node biopsies, bone marrow investigation, flow-cytometry, immunophenotyping, patch tests and CT-scans were performed. We also examined follow-up data concerning the management, outcome and relapses when such information was available. For statistical analysis, data was compiled electronically into Excel programme and analysed using SPSS® (Statistical Package for the Social Sciences, v. 20). Clinical and laboratory data were analysed by chi-square (v2) and Fischer tests looking for a possible relationship between clinical data, laboratory tests, and corresponding etiologies. Statistical significance wa defined as P<0.05.
Ethics Statement
Patientshave given their informed consent and thatthe study protocol has been approved by the institute’s committee onhuman research.
RESULTS
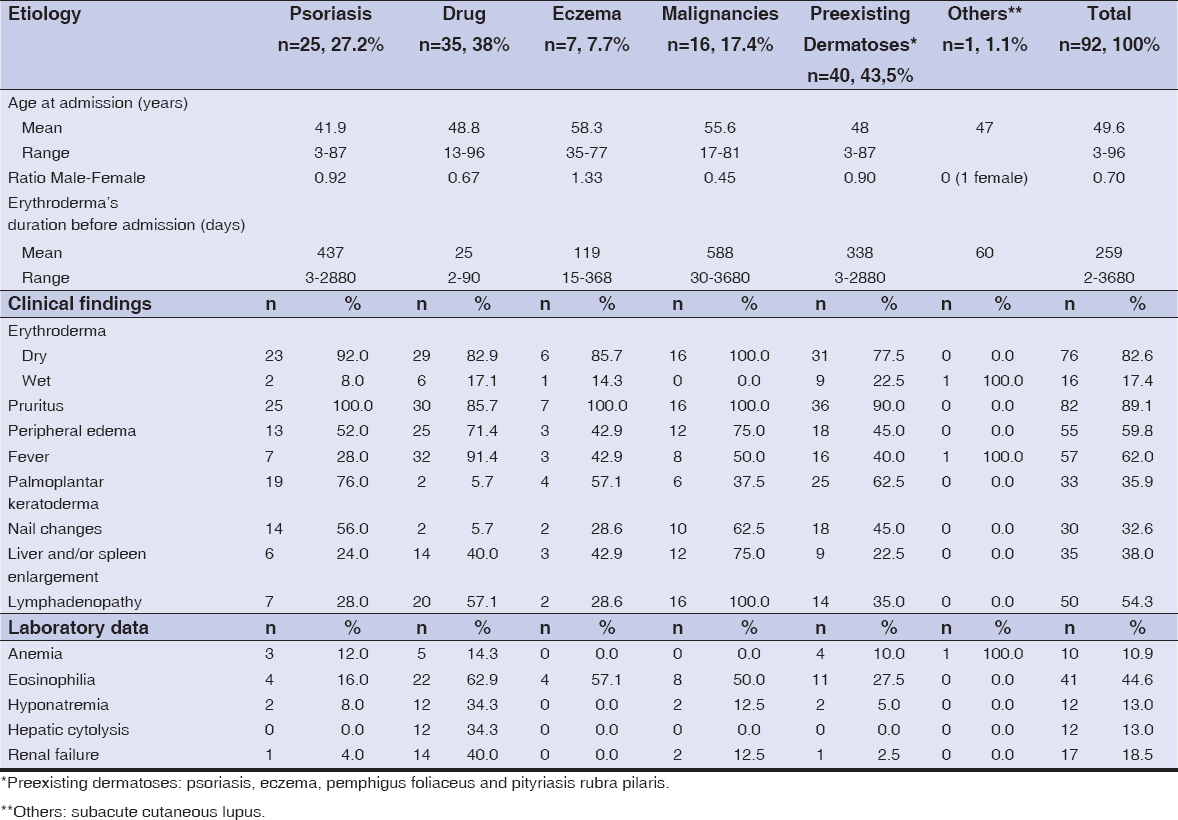
During the study period, 1700 patients were hospitalized in the Department of Dermatology. Erythroderma was diagnosed in 92 patients (5.41%), corresponding to an incidence of 20 cases/year. The average age was 49.6 years (range 3–96) with a male to female ratio of 0.70. Patients were seen in our department at a median of 259 days (range 2 to 3680 days) after the onset of erythroderma. A shorter duration was observed in patients with drug-induced erythroderma and a longer one with erythroderma caused by malignacies. In 48 (52.2%) of the 92 patients, erythroderma began acutely. As shown in table 1, erythroderma was dry in 82.6% of cases, pruritus was the most common complaint, was recorded in 82 (89.1%) patients; 57 of the 92 patients (62%) had a fever during the episode, 55 patients (59.8%) had pitting edema, palmoplantar keratoderma were found in 33 patients (35.9%) mostly in the group of psoriasis patients. Nail changes (including Beau’s lines, onychodystrophy, pits, discoloration, subungual hyperkeratosis, onycholysis and paronychia) were observed in 30 (32.6%) patients. Nail changes were mostly found in malignancies and psoriasis patients. Other main symptoms included liver and/or spleen enlargement in 35 (38%) patients and lymph node enlargement in 50 (54.3%) patients.
Eosinophilia in 44.6% of patients. Kidney failure in 18.3%. Hepatic cytolysis and hyponatremia in 12.9%. Inflammatory anemia was found in 10.9% of patients.
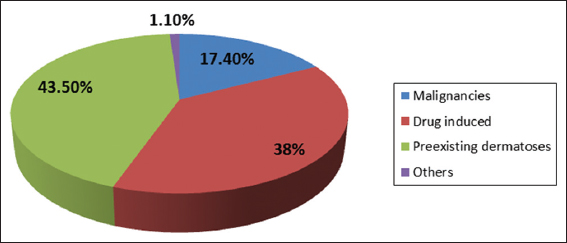
Laboratory abnormalities are also summarized in table 1, including inflammatory anemia, eosinophilia, hyponatremia, hepatic cytolysis and renal failure. Cutaneous biopsy was performed in 55 (59.78%) patients. A skin biopsy was not performed in the rest of the patients because the cause of erythroderma was clear from the start as previous dermatosis. The biopsy was usually performed during the first three days after the patient was admitted to the hospital. The most common cause of erythroderma was exacerbation of pre-existing dermatoses (43.5%), including psoriasis (27.2%), eczema (7.6%), pemphigus foliaceous (6.5%) and pityriasis rubra pilaris (2.2%). Followed by drug reactions (38%) dominated by the DRESS syndrome (30.4%). Cutaneous T-cell lymphomas constituted 15.2% of the causes of erythroderma.
Etiologically, the 92 patients were categorized into four groups (Fig. 1): (1) Pre-existing dermatoses (49 patients, 43.5%): psoriasis 25 (27.2%), eczema 7 (7.7%), pemphigus foliaceus 6 (6.5%), pityriasis rubra pilaris 2 (2,2%). (2) Drug reactions (35 patients, 38%). (3) Malignancies (16 patients, 17.4%): mycosis fungoides and sezarysyndrom (14), lung cancer (1), cavum cancer (1). (4) Others (1 patient, 1.1% subacute cutaneous lupus).
Some etiologies were significantly associated with certain clinical signs and biological tests:
- Acute onset and drug-induced erythroderma (p = 0.000).
- Chronic onset and pre-existing dermatoses and malignancies (p=0.000).
- Dry erythroderma and malignancies (p=0.031).
- Fever and drug-induced erythroderma (p = 0.000).
- Peripheral edema and drug-induced erythroderma and malignancies (p=0.035).
- Palmoplantar keratoderma and pre-existing dermatoses (Psoriasis and Pityriasis rubra pilaris) (p = 0.000).
- Nail changes and psoriasis and mycosis fungoïde (p=0.000).
- Lymphadenopathy as well as liver/spleen enlargement were clinical features significantly associated with malignancy- related erythroderma cases (p=0.000 and p=0.003, respectively).
- Lymphadenopathy and drug-induced erythroderma (p = 0.000).
- Hypereosinophilia with drug-induced erythroderma (p = 0.015).
- Hepatic cytolysis was more frequently objectified in the drug reactions (p = 0.004).
No other cause of erythroderma was significantly associated with any of the remaining laboratory abnormalities analyzed (including anemia, hyponatremia or renal failure).
The evolution was good in 87% of the patients, whose methods of management were based on symptomatic measures in association with the etiological treatment. 10 patients died after transfer to an intensive care unit, either because of the etiology of erythroderma, the decompensation of an underlying pathology, or of infectious shock.
DISCUSSION
We collected 92 cases of erythroderma in an four-and-a-half-year period, corresponding to an incidence of 20 cases/year. A survey of erythroderma cases conducted in the Portugal identified an annual incidence of 9.4 cases/year [1], and another Tunisian series reported a hospital incidence of 6.3 cases/year [5], an increased incidence as we found, has never been noted in the literature, this could be explained by the delay of the consultation of patients. Erythroderma usually occurs in the fifth decade with a male predominance in the majority of reported studies [6–14]. Our series is in accordance with the literature, concerning the age of patients, but with a female predominance. Typically, the onset of erythroderma is gradual and insidious [5,9–11], except in the drug-induced cases, where it tends to be sudden [5,12] In our series we identified similar results, given that drug-induced cases were associated with a shorter duration of erythroderma before admission. The approach of patients with erythroderma depends on their previous dermatological background. Patients with a history of dermatological disorder may develop erythroderma during a flareup. In such cases, the aetiological diagnosis is easy to reach. Otherwise, erythroderma remains a diagnostic challenge. In one series reported by Eugster et al., five patients among seven with malignancy-related erythroderma had a history of preexisting psoriasis.[12] Furthermore, drugs can also precipitate erythroderma in a well known psoriatic patient. So, it is important to consider other possible aetiologies even in patients who may have a clear history of pre-existing dermatosis [15,16].
The final diagnosis is a result of the evaluation of the clinical, biochemical, histological findings and the evolution of the erythroderma in each individual patient. Like many other series [4, 8–14], the majority of clinical features were non-specific. As in other studies [11,12,14], pruritus was the most common complaint of our patients and could not be traced to any specific cause of erythroderma. In this respect, only one retrospective study on the subject has found a significant association between pruritus and psoriasis [8]. As was the case of our series, other reports have found that palmoplantar keratoderma [8,9] as well as nail changes [8,9,12] are predictive clinical signs of psoriasis. Thus, in the absence of history of psoriasis, these cutaneous modifications may direct clinicians to psoriasis.
Edema was reported to be to drug reactions [17,18]. In our study, half of patients presented edema as it was seen in the Portugal survey [1]. We also found a significant relation between edema, drug consumption and malignancies. More than half of our patients had fever, comparable to the incidence reported in other studies [8,11–14]. We also noted that fever was more frequently associated with drug reactions, an association previously identified in three other recent series [1,8,9]. We found a higher percentage of lymphadenopathy and hepatic/splenic enlargement in comparison with previous series [8–14].
In previous publications, lymphadenopathy has been associated with cutaneous T-cell lymphomas, drug reactions and psoriasis [10] Hepatic or splenic enlargement have been reported in association with erythroderma caused by drug consumption [2]. In our study however, we only found significant associations between both lymphadenopathy and hepatic/splenic enlargement, and the group of patients with cutaneous T-cell lymphomas. Also between lymphadenopathy and drug consumption. In our series, drug-induced erythroderma was significantly associated with hypereosinophilia. The latter is, however, not a specific finding limited to drug reactions, as it has been previously reported in other studies to be also significantly associated with psoriasis, eczema and cutaneous T-cell lymphoma [1,5,8,9].
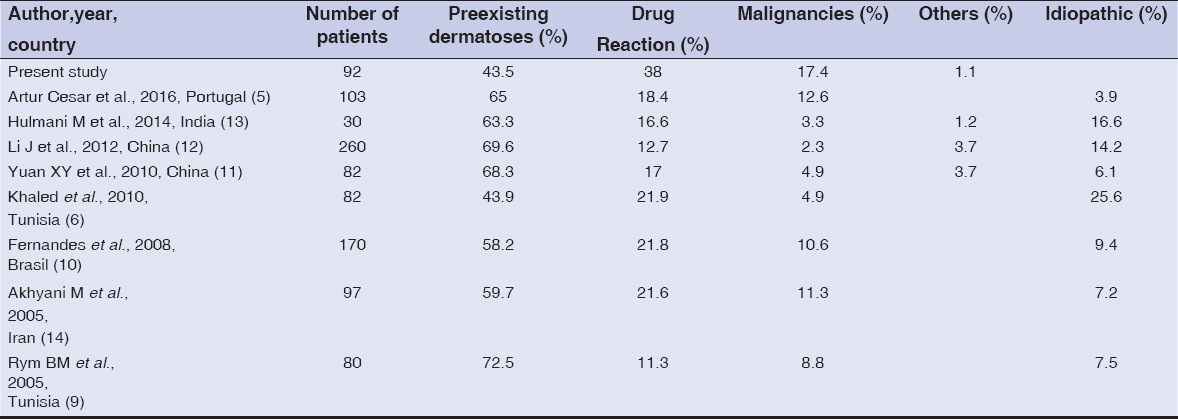
Comparison of the etiological groups among recent series of erythroderma and our own is given in Table 2. This table reveals a variation of the relative incidence of the different etiological groups of erythroderma. This may be partly related to genetic, geographical and social disparities. Our findings support the perception that non-malignant erythroderma, despite often bringing distress to patients, most often does not pose a significant risk to the patient’s life [19]. Despite its limitations as a retrospective design, this study provides us with interesting information related to clinical features of erythroderma. However, long-term prognostic assessment, close follow-up and better study design are needed in future studies.
CONCLUSION
Erythroderma is a dermatological clinical syndrome of generalized erythema and scaling, due to various etiologies. Although the causes may be diverse, most cases of erythroderma have a preexisting skin disease. Patients with previously normal skin often have drug-induced erythroderma or malignancy. Indeed, its early diagnosis allows a fast and adequate care thus improving the prognosis of these entities. In the uncommon cases were no underlying cause is found, close follow-up is recommended. Early diagnosis for skin diseases in our country avoids consultation at advanced stages as erythroderma, and decrease the frequency of erythroderma and its complications in our context.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Artur Cesar, Maria Cruz, Alberto Mota, Filomena Azevedo. Erythroderma. A clinical and etiological study of 103 patients. J Dermatol Case Rep. 2016;10:1–9.
2. Ndiaye M, Ly F, DiousséP, Diallo M, Diop A, Diatta BA, et al. [The characteristics of severe forms of psoriasis on pigmented skins:A retrospective study of 102 cases in Dakar, Senagal]. Our Dermatol Online. 2017;8:138-42.
3. Caroline Ram-Wolff, Nadine Martin-Garcia,Armand Bensussan, Martine Bagotand Nicolas Ortonne. Histopathologic diagnosis of lymphomatous versus inflammatory erythroderma:a morphologic and phenotypic study on 47 skin biopsies. Am J Dermatopathol. 2010;32:755–63.
4. Nupur P, Singh R. Erythroderma:a clinico –etiological study in a tertiary hospital. Int J Scien Res. 2018;7:8179.
5. Khaled A, Sellami A, Fazaa B, Kharfi M, Zeglaoui F, Kamoun MR. Acquired erythroderma in adults:a clinical and prognostic study. J Eur Acad Dermatol Venereol. 2010;24:781-8.
6. Diallo M, Diadie S, Diatta BA, Diop A, Ndiaye MT, Ndiaye M, et al. Acquired erythroderma in adults in senegal:epidemiological and etiological aspects. Dermatol Case Rep. 2017;2:128.
7. Tan GFL, Kong YL, Tan ASL,Tey HL. Causes and Features of Erythroderma. Ann Acad Med Singapore. 2014;43:391-4.
8. Sehgal VN, Srivastava G, Sardana K, MNAMS. Erythroderma ⁄exfoliative dermatitis:a synopsis. Int JDermatol. 2004;43:39–47.
9. Rym BM, Mourad M, Bechir Z, Dalenda E, Faika C, Iadh AM, et al. Erythroderma in adults:a report of 80 cases. Int J Dermatol. 2005;44:731-5.
10. Fernandes NC, Pereira FSM, Maceira JP, Cuzzi T, Dresch TFLR, Araújo PP. Eritrodermia:estudoclínico-laboratorial e histopatológico de 170 casos. An Bras Dermatol. 2008;83:532-36.
11. Yuan XY, Guo JY, Dang YP, Qiao L, Liu W. Erythroderma:A clinical-etiological study of 82 cases. Eur J Dermatol. 2010;20:373-7.
12. Li J, Zheng HY. Erythroderma:a clinical and prognostic study. Dermatology. 2012;225:154-62.
13. Hulmani M, Nandakishore B, Bhat MR, Sukumar D, Martis J, Kamath G, et al. Clinico-etiological study of 30 erythroderma cases from tertiary center in South India. Indian Dermatol Online J. 2014;5:25-9.
14. Akhyani M, Ghodsi ZS, Toosi S, Dabbaghian H. Erythroderma:a clinical study of 97 cases. BMC Dermatol. 2005;5:5.
15. Rothe MJ, Bernstein ML, Grant-Kels JM Life-threatening erythroderma:diagnosing and treating the “red man“. Clin Dermatol. 2005;23:206-17.
16. Eugster R, Kisling S, Brand CU. Clinical aspects and aetiology of erythroderma:an analysis of 64 cases. ScweizRundscMed Prax. 2001;90:1449–54.
17. Mistry N, Gupta A, Alavi A, Sibbald RG. A review of the diagnosis nd management of erythroderma (generalized red skin). Adv Skin Wound Care. 2015;28:228-36;quiz 237-8.
18. Maldonado-García CA, Orozco-Anahuatib AP. Abordajediagnóstico de la eritrodermia en el adulto. Rev Med Inst Mex Seguro Soc. 2017;55:353-60.
19. Shirazi N, Jindal R, Jain A, Yadav K, Ahmad S. Erythroderma:A clinico-etiological study of 58 cases in a tertiary hospital of North India. Asian J Med Scien. 2015;6:20-4.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Comments are closed.