|
Get Citation
|
|
|
Brzezinski P, Sousak M, Bimbi C. Erythema annulare centrifugum preceding carcinoma larynx. Our Dermatol Online. 2018;9(4):443-446. |
|
|
Download citation file:
|
Erythema annulare centrifugum preceding carcinoma larynx
Piotr Brzezinski1,2, Masaoud Sousak3, Cesar Bimbi4
1Institute of Biology and Environmental Protection, Pomeranian Academy, ul. Arciszewskiego 22A, 76-200 Slupsk, Poland, 2Department of Dermatology, Provincial Specialist Hospital in Slupsk, ul. Mickiewicza 12, 76-270 Ustka, Poland, 3General Surgery Department, Paluckie Health Center, Znin, Poland, 4Institute of Dermatology Centro Historico, Dermatology, Porto Alegre, Brazil
Corresponding author: Dr. Piotr Brzezinski, E-mail: brzezoo77@yahoo.com
Submission: 12.03.2018; Acceptance: 01.09.2018
DOI: 10.7241/ourd.20184.23
ABSTRACT
Erythema annulare centrifugum (EAC) is characterized by annular, erythematous plaques with trailing scale. The skin lesions may be indurated or soft and may be static or spread centrifugally. It is considered to be a reactive condition with a wide variety of inciting causes but unclear pathophysiology. We describe a 62-year-old man with EAC. Since no association of EAC with concomitant bacterial or viral infections, we started diagnostics in the direction of systemic disease or cancer. Investigations confirmed carcinoma of larynx. We want to emphasize that EAC can appear many years before the onset of carcinoma. This is the first description of the ECM and carcinoma of the larynx with a long list of co-existing cancers.
Key words: Erythema annulare centrifugum; Erythema; Erythematous plaques; Carcinoma larynx; Carcinoma planoepitheliale
INTRODUCTION
Erythema annulare centrifugum (EAC) initially described in 1881. The term erythema annulare centrifugum first was used 1916 (Darier/Darier-Lipschütz). It includes erythema perstans, erythema gyratum perstans, erythema marginatum perstans, erythema exudativum perstans, erythema microgyratum perstans, erythema figuratum perstans, and erythema simplex gyratum. EAC is characterized by annular, erythematous plaques with trailing scale. The skin lesions may be indurated or soft and may be static or spread centrifugally [1].
It is considered to be a reactive condition with a wide variety of inciting causes but unclear pathophysiology [2].
Although its etiology is not known for certain, it is assumed to be hypersensitivity reaction to malignancies, infections, and drugs. Inciting factors may include viral (Epstein-Barr virus), bacterial (Streptococcal infections, E. coli), or fungal infections (dermatophytes), parasites, arthropod assault, medications (spironolactone, amitryptiline, ampicillin, cimetidine, hydrochlorothiazide, salicylates), malignant conditions or other systemic diseases, and foods. The eruption clears with cessation of the drug or treatment of the associated disease. However, in the majority of cases no underlying cause is identified [3–5].
The prognosis for EAC is excellent, except when associated with an underlying malignancy and other systemic disease. A diagnosis of EAC should be followed by diagnostic workup because it may result in discovery of an underlying disease.
The coexistence of EAC and cancer is used determine: Paraneoplasticerythema Annulare centrifugum eruption (PEACE) [6]. PEACE is speculated to be a result of a cytokine or other tumor-associated factors.
We describe a 62-year-old man affected by EAC who upon further examination was diagnosed carcinoma larynx.
CASE REPORT
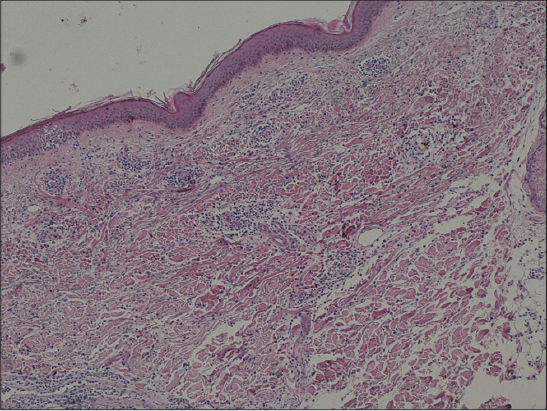
A 62-year-old male patient was admitted to our clinic with erythematous, annular, polycyclic plaques with indurated borders, without desquamation and rarely itching, on the limbs (Fig. 1).
Skin lesions was for more than 2 years. Clinical lesions was suggested EAC.
Skin punch biopsy revealed focal epidermal spongiosis and focal parakeratosis with eosinophils (Fig. 2).
The patient was diagnosed as EAC based on histopathologic and clinical findings.
The patient was excluded fungal infections (PAS stains for exclusion of fungi and wet mount microscopy for mycosis – negative); parasites; medications and started diagnostics in the direction of systemic disease or cancer.
Routine laboratory findings were within the normal ranges, Borrelia serology were negative.
The patient was referred to a specialist in internal medicine.
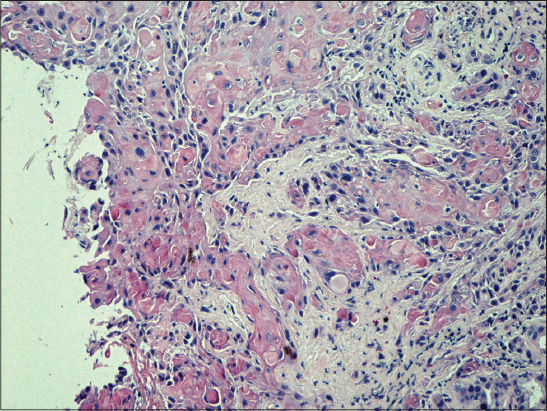
The patient came to the dermatology clinic only for six months (it was during radiotherapy due to carcinoma larynx). Histopathological diagnosis carcinoma of larynx was a carcinoma planoepitheliale (G2) (Fig. 3).
On the interview with the patient, otolaryngological and videolaryngostroboscopic examinations we diagnosed hypertrophic changes in the whole length of the right vocal fold with the fold mobility preserved.
The skin lesions decreased skin and reduce (but not resolved completely).
Currently you are finished radiotherapy. Skin lesions not occurs (three-month observation).
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
There are two types of EAC (by Ackerman): a deep type with indurated borders, without desquamation and rarely itching. A superficial type with desquamation following the advancing border and itching is more frequent. It is not clear whether these represent two separate diseases or a continuous range [4].
A review of medical literature reveals that malignancies related to EAC are acute myelocytic leukemia, Hodgkin’s lymphoma, chronic lymphocytic leukemia, multiple myeloma, malignant histiocytosis [5] and internal organs cancers: nasopharyngeal carcinoma, peritoneal carcinomatosis, primary bronchial carcinoid, prostate carcinoma, mucinous ovarian carcinoma, breast cancer, metastatic gastric carcinoma [1,2].
One study of 66 cases identified cutaneous fungal infection as the most important etiologic factor (72%), while other causes included benign internal neoplasm (13%), skin diseases (18%) and internal diseases (21%) [6]. A study involving 73 EAC patients revealed neoplasia in 7% of deep type EAC cases [7].
Laryngeal cancer may also be called cancer of the larynx or laryngeal carcinoma.
Incidence is five in 100,000 (12,500 new cases per year) in the USA. The American Cancer Society estimated that 9,510 men and women (7,700 men and 1,810 women) would be diagnosed with and 3,740 men and women would die of laryngeal cancer in 2006.
Each year, about 2,200 people in the U.K. are diagnosed with laryngeal cancer [8].
Most laryngeal cancers are squamous cell carcinomas, reflecting their origin from the squamous cells which form the majority of the laryngeal epithelium. Cancer can develop in any part of the larynx, but the cure rate is affected by the location of the tumour.
Smoking is the most important risk factor for laryngeal cancer. Heavy chronic consumption of alcohol, particularly alcoholic spirits, is also significant. Some other quoted risk factors are low socioeconomic status, male sex, and age greater than 55 years.
Our patient was a hoarseness and persistent cough (he smoked cigarettes).
Ayca Alan Atalay at al described 52-year-old man affected by EAC, who upon further examination was diagnosed with squamous cell carcinoma of the lung (SCCL) [9]. The plaques had been present for more than 3 months.
Authors from Bulgaria describe recurrence of breast cancer after 10 years in a 73-year-old Caucasian female patient presented for three annular erythematous lesions on the left leg and buttock, persisting for two months [10].
CONCLUSION
Long-term, recurrent, non-specific cutaneous lesions are the most frequent cutaneous manifestation in patients with cancer. Our patient was a smoker, had a hoarseness and persistent cough and so EAC.
Although the EAC recurred since two years, carcinoma of the larynx was diagnosed in a “good” period (non-metastatic).
We want to emphasize that EAC can appear many years before the onset of carcinoma.
This is the first description of the ECM and carcinoma of the larynx with a long list of co-existing cancers.
ACKNOWLEDGEMENTS
Ass. Prof. Viktoryia Kazlouskaya (Ackerman Academy of Dermatopathology, NY USA.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Lee HJ, Chang SE, Lee MW, Choi JH, Moon KC, Koh JK. Metastatic gastric carcinoma presenting as an erythema annulare centrifugum-like lesion. Br J Dermatol. 2007;157:1044-5.
2. Panasiti V, Devirgiliis V, Curzio M, Rossi M, Roberti V, Bottoni U, et al. Erythema annulare centrifugum as the presenting sign of breast carcinoma. J Dermatol. 2008;35:186-7.
3. Abreu Velez AM, Avila IC, Howard MS. Immune response in a cutaneous allergic drug reaction secondary to imidapril, benazapril and metformin. Our Dermatol Online. 2013;4:192-5.
4. Chodkiewicz HM, Cohen PR. Paraneoplastic erythema annulare centrifugum eruption: PEACE. Am J Clin Dermatol. 2012;13:239-46.
5. Narváez D, Di Martino Ortiz B, Rodríguez Masi M. Annular skin lesions in childhood: Review of the main differential diagnoses. Our Dermatol Online. 2017;8:75-80.
6. Kim KJ, Chang SE, Choi JH. Clinicopathologic analysis of 66 cases of erythema annulare centrifugum. J Dermatol. 2002;29:61-7.
7. Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol. 2003;25:451-62.
8. Toraub K, Jeewon R. Sociodemographic factors and their association to prevalence of skin diseases among adolescents. Our Dermatol Online. 2013;4:281-6.
9. Atalay AA, Abuaf OK, Dogan B. Squamous cell lung carcinoma presenting with erythema annulare centrifugum. Acta Dermatovenerol Croat. 2013;21:56-8.
10. Dourmishev LA, Gergovska MJ, Nikolova K, Balabanova MB. Erythema annulare centrifugum in a patient operated on for breast carcinoma. Acta Dermatovenerol Croat. 2010;18:264-6.
Notes
Source of Support: Nil
Conflict of Interest: None declared.

Comments are closed.