|
Get Citation
|
|
|
Chang P, Meaux T. Onychomatrichoma. Our Dermatol Online. 2017;9(1):80-81. |
|
|
Download citation file:
|
Onychomatrichoma
1Department of Dermatology, Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala; 2Resident of LSU Dermatology, Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala
Corresponding author: Dr. Patricia Chang, E-mail: pchang2622@gmail.com
Submission: 10.04.2017; Acceptance: 23.10.2017
DOI: 10.7241/ourd.20181.23
40-year-old female referred by her general practitioner for treatment of a fungus on the nail of the left index finger. The lesion had been present for five years and previously treated with fluconazole for 6 months without improvement.
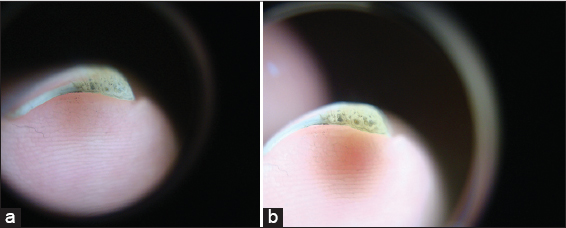
Physical examination revealed an onychopathy localized to the nail of the left index finger, characterized by a yellowish discoloration, thickening, onycholysis, and splinter hemorrhages (Fig. 1), dermoscopic examination showed dimples of distal nail plate (Fig. 2a and b). The remainder of the physical examination was unremarkable.
No significant past medical or family history. dimples of distal nail plate
The lesion had been present for five years, and began with changes in the color of the nail and asymptomatic thickening of its edge. The patient was diagnosed with onychomycosis and treated without observed changes, and therefore he was referred to our department.
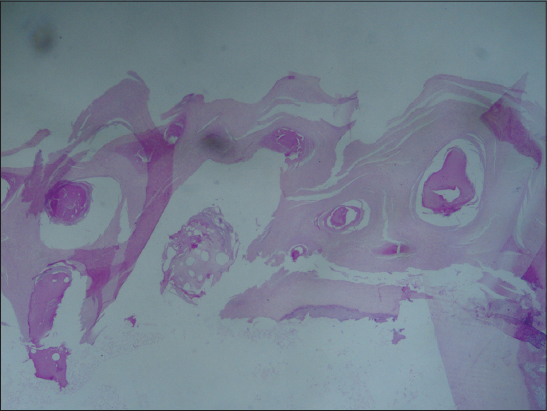
With this clinical data, the diagnosis of onychomatricoma was made (Fig. 1) dermoscopic panoramic view of the distal nail plate with small cavities (Fig. 2a) and dermoscopic close up of the small cavities at the free edge of the nail (Fig. 2b) and biopsy was performed of the free border of the nail plate was performed. Hematoxylin and eosin staining revealed the presence of keratin-filled cavities (Fig. 3).
First described by Baran and Kint in 1992, onychomatricoma is a rare, benign, usually painless tumor of the nail matrix. It characterized by digitiform projections from the matrix that also leads to changes of the nail plate. Women in the 5th decade of life are most commonly affected [1]. Clinically, one or multiple fingernails may contain the tumor simultaneously. Physical exam findings include xanthonychia, ungula hyperkeratosis, splinter hemorrhages and longitudinal transverse over-curvature of the nail plate [1–3]. A frontal view of the nail typically reveals multiple holes in the thickened free margin. Tumors may affect the entire nail matrix and nail plate, with the authors of one article suggesting the name “giant onychomatricomas” for this variant [4]. Potentially misleading clinical findings, such as verrucous surface, total dystrophy of the nail unit, and a pseudofibrokeratoma appearance, have been reported as well. Thus, differential diagnoses may include verruca or Bowen’s disease, squamous cell carcinoma, and fibrokeratoma, respectively [5,6]. Diagnosis is often clinical, however histopathologic examination is required in less obvious cases, such as those mentioned above. Excision is usually curative.
As mentioned previously, onychomatricoma is a benign tumor with a fairly straightforward clinical diagnosis in most cases, if the clinician is aware of its existence. The rarity of this entity and possible confusion due to less than classic clinical presentation may require further workup. Diagnosis may not be obvious until surgery is performed, at which point the typical filiform projections are more visible [4]. Pathologists may be faced with making the diagnosis without the nail plate, as it is often not submitted. In these cases, histologic findings are characterized by a pedunculated fibroepithelial tumor reminiscent of a fibrokeratoma on longitudinal section. Distinguishing features include epithelial-lined invaginations around optical cavities and a stroma organized in 2 layers. A good potential marker of onychomatricoma is antibody AE13, specific to trichocytic keratins Ha 1-4 [7]. Immunohistochemistry can also be helpful. Onychomatricoma typically exhibits positive staining for CD34, epithelial membrane antigen, S-100, actin, and desmin [6]. Keratinization is without a granular layer [3]. Although considered a benign lesion, onychomatricoma may have malignant potential. Complete excision recommended to avoid recurrence [2].
REFERENCES
1. Tavares GT, Chiacchio NG, de Souza MV. Onychomatricoma:a tumor unknown to dermatologists. An Bras Dermatol. 2015;90:265-7.
2. Chang P, Meaux T. Onicomatricoma. Informe de un caso. DCMQ. 2015;13:162-4.
3. Tosti A, Piraccini BM. Nail Disorders In:Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. 3rd ed. Philadelphia, PA:Elsevier Saunders;2012:chap 71:1145.
4. Estrada-Chavez G, Vega-Memije ME, Toussaint-Caire S, Rangel L, Dominguez-Cherit J. Giant onychomatricoma:report of two cases with rare clinical presentation. Int J Dermatol. 2007;46:634-6.
5. Perrin C, Baran R, Balaguer T, Chignon-Sicard B, Cannata GE, Petrella T, MichielsJF. Onychomatricoma:new clinical and histological features. A review of 19 tumors. Am J Dermatopathol. 2010;32:1-8.
6. Fraga GR, Patterson JW, McHargue CA. Onychomatricoma:report of a case and its comparison with fibrokeratoma of the nailbed. J Dermatopathol. 2001;23:36-40.
7. Perrin C, Baran R, Pisani A, Ortonne JP, Michiels JF. The onychomatricoma:additional histologic criteria and immunohistochemical study. Am J Dermatopathol. 2002;24:199-203.
Notes
Source of Support: Nil
Conflict of Interest: None declared.

Comments are closed.