Data analysis of 287 patients present with erythema nodosum: A closer look at associations
Oktem Ayse, Incel Uysal Pinar, Sahin Buket, Yalcin Basak
1Department of Dermatology, Ankara Numune Training and Research Hospital, Ankara, Turkey
Corresponding author: Dr. Oktem Ayse, E-mail: ayseoktem@yahoo.com
Submission: 19.07.2017; Acceptance: 08.09.2017
DOI: 10.7241/ourd.20181.1
ABSTRACT
Background: Erythema nodosum (EN) is the most common clinical variant of panniculitis. It may occur in association with a wide variety of causative stimuli. The aim of our study is to describe the possible etiologic factors associated with EN and compare them with the series previously reported in the literature.
Materials and Method: This is a retrospective chart review of 287 patients who have presented to our clinic with tender erythematous nodular lesions and finally diagnosed as eythema nodosum between January 2010 and December 2015.
Results: Our retrospective study included 239 females and 48 males (sex ratio, 5:1). Of the 287 EN patients, etiologic factor has been determined in 123 (42.85%) of the participants and this group was categorized as secondary EN. In secondary EN group the leading etiologic factor was infections (n=68, 23.69%). Other etiologic factors were Behcet’s Disease (n=18, 6.27%), connective tissue disease (n=8, 2.78%), tuberculosis (n=6, 2.09%) sarcoidosis (n= 5, %1.74), drugs (n=6, 2.09%), granulomatous mastitis (n=2, 0.69%), IBD (n=2,0.69%), malignancy (n=1, 0.34%) and food supplement (n=1, 0.34%).
Conclusion: Our data confirm that viral and bacterial infections are the leading causative factors of EN, followed by Behcet’s Disease, pregnancy and connective tissue disease (CTD). These conditions should be investigated as part of systemic search.
Key words: Behcet’s Disease; Erythema Nodosum; Erythematous Nodule
INTRODUCTION
Erythema nodosum (EN) is the most common clinical variant of panniculitis which is characterized with symmetric, warm, non-ulcerating, non-scarring, tender, red nodosities. The condition frequently occurs on the lower extremities especially on pretibial regions. Most cases appear between the second and fourth decades and the condition affects females more frequently [1–3].
The lesions generally tend to regress within three or four weeks spontaneously. New crops of lesions may continue to appear up to 6 weeks. Even though the diagnosis is based on mainly typical clinical characteristics, deep incisional biopsy may be beneficial for atypical cases. Histopathological examination reveals hypodermal septal inflammation without sign of vasculitis. The exact pathogenesis remains unclear even though it is considered to be a hypersensitivity reaction against various antigenic stimuli. It may occur in association with a wide variety of causative stimuli including infection diseases, drugs, inflammatory bowel disease (IBH), sarcoidosis, tuberculosis, Behcet’s disease (BD) and malignancy. Despite most cases have no clearly identified causative factor, it may be a cutaneous sign of systemic serious comorbidity [1,3,4].
The aim of our study is to describe the possible etiologic factors associated with EN, to examine the characteristics of the primary and secondary forms of the disease and to compare them with the series previously reported in the literature. For this purpose we have collected data of the patients with the diagnosis of EN who have been diagnosed and treated in our department during the period of 2010-2015.
MATERIALS AND METHODS
This is a retrospective chart review of 287 patients who have presented to our outpatient clinic with tender erythematous nodular lesions between January 2010 and December 2015. They were finally diagnosed EN by characteristic clinical findings with or without histological confirmation. Skin biopsies have been carried out in the patients (n= 62) who had not been diagnosed with existing clinical features and had atypical clinical presentation.
Patients were included on the basis of recorded data on the software of hospital information system, Fonet. Medical charts of patients with the ICD code of erythema nodosum for past medical history, infectious symptoms and drug use in preceding weeks. The demographic features (age and sex); clinical features, laboratory tests including complete blood count, erythrocyte sedimentation rate, C-reactive protein, liver function tests, rheumatoid factor, angiotensin converting enzyme, hepatitis B and C serology, anti-streptolysin O (ASO) titer in two consecutive evaluation at 2-4 weeks intervals, anti-nuclear antibody (ANA), urine test; tuberculin skin test; radiological studies including chest x-ray and thorax computed tomography results were evaluated. Patients who had incompatible histological characteristics and whose data were lacking were excluded from the study.
We diagnosed group A beta-hemolytic streptococcal infections with positive throat culture with/or two high consecutive ASO titers with 2-4 weeks interval. We considered patients as viral upper respiratory tract infection when there are clinical findings without bacteriologic evidence of streptococcal or any other bacteriologic infection. Diagnosis of tuberculosis and sarcoidosis were biopsy proven. Patients were questioned and evaluated for the signs and symptoms of BD according to the recently described diagnostic criteria of Behcet’s Syndrome International Study Group Criteria [5] and these patients were newly diagnosed with BD after the clinical presentation of EN lesions. Given the aim of this study is examining patients present with erythema nodosum we excluded the data of BD patients who had been following-up in our Behcet disease outpatient clinic. 58% of whom had EN/EN like lesions during follow-up period.
Patients with EN who were previously diagnosed of BD and in our clinic. Continuous data were reported as the mean SD and categorical variables were reported as percentages.
Ethics Statement
The methods were in accordance with ethical principles of Declaration of Helsinki and the approval letter of ethics committee was obtained.
RESULTS
Patients in our retrospective study included 239 females and 48 males (sex ratio, 5:1). Patient’s ages ranged between of 8-88 years (mean age of 39.2). Thirty eight percent (n=38) of the patients were required inpatient management. Mean hospital stay was 16 days for these patients. Many of the outpatient cases (n=169 patients, 58.88%) were sufficiently treated with removing triggering factor, leg elevation, wet dressing (with 0.9% NaCl or eau de goulard for 20 minutes twice in a day) with bed-rest. In 37 patients nonsteroidal anti-inflammatory drugs and potassium iodide treatment (300-500 mg three times daily) were effective. Colchicine or colchicine-corticosteroid combination was used in 27 of inpatients, effectively. Three of patients who have presented with severe clinical symptoms or did not show clinical improvement were treated with colchicine, corticosteroid and azothioprine combination.
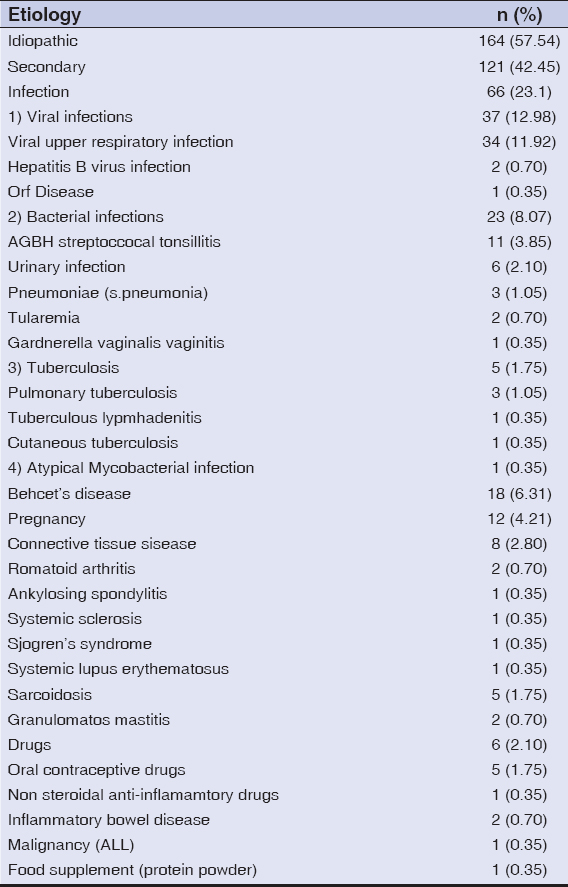
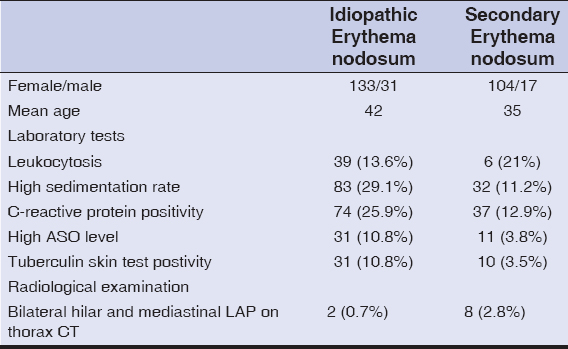
Of the 287 EN patients, we could not identify any causative factor or association in 164 (57.14%) of participants. Possible etiologic factor has been determined in 123(42.85%) of the participants and this group was categorized as secondary EN (Table 1).
Prodromal systemic symptoms were exist in 25% (n=41) of primary and 38% (n=46) of secondary groups. Atypical clinical presentation (n=62) such as unilateral involvement, or atypical localization including upper extremities, gluteus, trunk and thighs were mostly – in 48 patients- observed in secondary EN group. In secondary EN group the leading etiologic factor was infections (n=68, 23.69%). Other etiologic factors were BD (n=18, 6.27%), connective tissue disease (n=8, 2.78%), tuberculosis (n=6, 2.09%) sarcoidosis (n= 5, 1.74%), drugs (n=6, 2.09%), granulomatous mastitis (n=2, 0.69%), IBD (n=2, 0.69 %), malignancy (n=1, 0.34%) and food supplement (n=1, 0.34%). Pregnancy was the precipitating event in twelve (5.02 %) of 239 female patients (Table 1).
Upper respiratory tract infections, common cold and influenza were the most common associated infectious triggers. The diagnosis of acute hepatitis B (HBV) infection was established by characteristic serologic profile in two patients and another one has had the history of chronic inactive hepatitis. In one patient EBV tonsillitis had been proven with acute exudative tonsillitis and EBV IgM positivity. A patient with a purulent-appearing papulonodular lesion on the finger and a history of contact with sheep had the diagnosis of orf disease. Among bacterial infections, group A beta-hemolytic streptococcal infections were discovered in eleven of patients. Six patients that had dysuria symptom and finding of Eschericia coli in urine culture were regarded as urinary tract infection. In three patient that have admitted with fever, cough with which phlegm, chest pain, infiltration in chest X-ray, a diagnosis of streptococcal pneumonia has been done with positive sputum cultures. Two cases that have had the history of living in the epidemic regions were considered the diagnosis of ulceroglandular tularemia. One female patient had a diagnosis of Gardnerella vaginalis associated vaginitis. We established active pulmonary tuberculosis in three, tuberculosis lymphadenitis in one, tuberculous spondylitis in one and cutaneous tuberculosis in one of the cases.
Eighteen (6.27%) of cases were diagnosed with BD. Five patients who have presented with typical Löfgren’s syndrome findings such as EN, bilateral hilar adenopathy were diagnosed with sarcoidosis. Granulomatous mastitis has been established in two females. The other potential etiologies and laboratory findings are summarized in Tables 1 and 2.
Regarding the patients with preceding viral upper respiratory tract infections and tonsillitis approximately 3 weeks of time interval was observed between the infection and onset of lesions. Exact time period could not be identified for other potential associations. There was not any detectable difference in primary or secondary EN groups according the lesion number. Highest number of EN lesions (nine nodules) was observed in a patient with the diagnosis of inflammatory bowel disease. During the 5-year data period recurrence was observed in twelve patients (9 of idiopathic group and 3 of secondary group; one had sarcoidosis, two had Behcet disease).
DISCUSSION
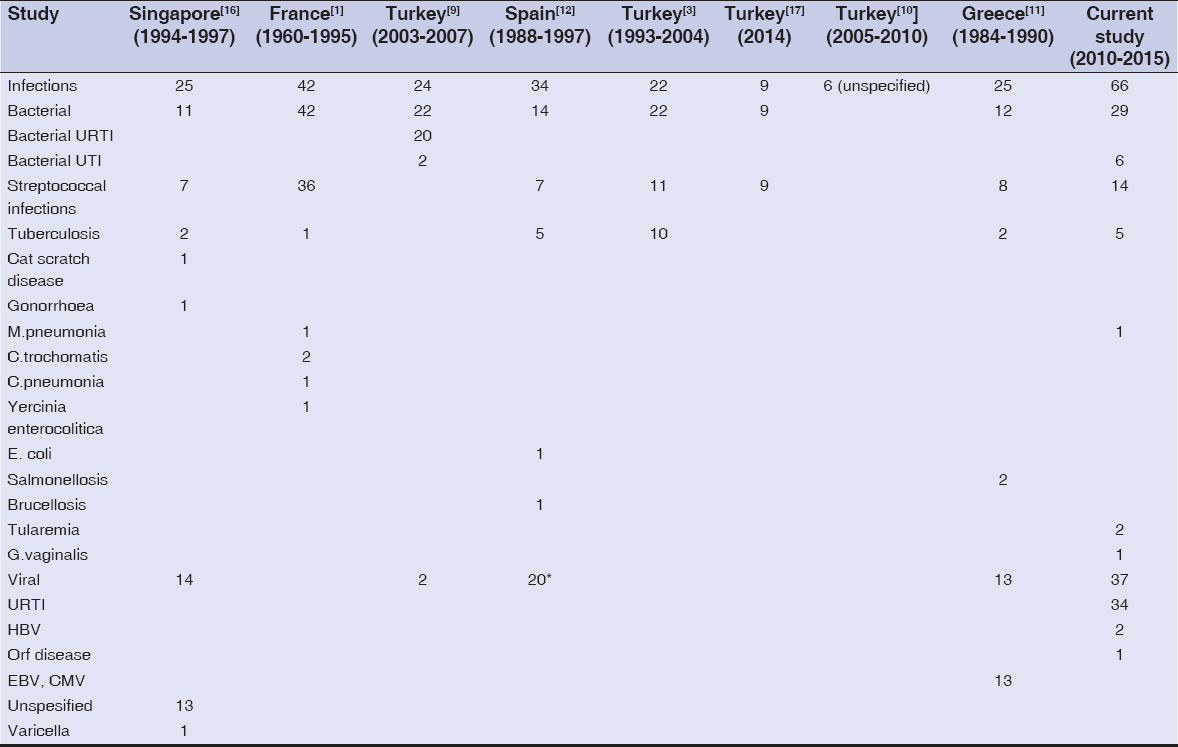
To our knowledge, this is the largest series of patients in the literature. Our study indicates that most common (23.1%) predictive factor of EN is infections and viral infections were the most common form. However demonstrating the causative factors and link between an infectious disease and EN may be extremely difficult because of the clinical or serologic improvement at the time of lesion development. Also, differentiating the preceding subclinical symptoms of erythema nodosum (malaise, arthritis, fever etc) from the prodromal period of an infectious etiology is a potential pitfall. On the other hand, drugs frequently implicated factors in etiology of EN, nevertheless we could assessed medication in 2% of participants. The incidence of drug use in the etiology of EN was much lower than we expected regarding the lack of data regarding medical history and unconsciously medication use attitudes of our society. For these reasons, we believe that infectious and medical triggers may be overlooked and these patients were classified as ‘idiopathic’ or primary EN.
There are variable results about the frequency of tuberculosis in the etiology of EN in Turkey. Mert et al. were reported higher frequencies of primary tuberculosis [3,6]. On the other hand none of the patients were diagnosed with primary tuberculosis in the series of Kisacik et al [7]. Our study revealed that tuberculine skin test (TST) was reactive in 41(14%) of all cases whereas mycobacterium tuberculosis infection could be identified as a predictive factor in 6 (2%) of the cases. Given the fact that EN is a reactive process of immuncompetent individuals, strong positive response to TST is not surprising especially in Turkey, high incidence setting for tuberculosis. Therefore, according to our experience, erythema nodosum may occur in patients with highly positive tuberculine skin test but without focus of infection.
In our series other uncommon infectious triggers were also identified; hepatitis B virus, parapoxviurs (orf disease), Francisella Tularensis (tularemia), Gardnerella Vaginalis, atypical mycobacterial infection. In literature numerous factors other than infections and drugs have been known to cause to EN; malignant disease, pregnancy, sarcoidosis and romatologic disease. Needless to say, the proportion of secondary factors and overall incidence of EN differs from between distinct geographic regions (Tables 3 and 4).
In contrary to some reports, we detected BD as a second common trigger in 6.3% of patients presenting with erythema nodosum [8]. Similar to other reports from our country, by taking into account data of BD patients who had develop EN lesions in the follow-up period, association of BD and EN was detected in 29,7% of our patients [9,10] (Table 3).
Sarcoidosis is one of the most common etiologic factors in Europe [11,12]. However, we detected sarcoidosis with the ratio of 1%. Pregnancy, hormone therapy and oral contraceptive pills are other well known triggering factors of EN [1,13]. In a young male patient we could associate EN with usage of protein powder supplement with the purpose of gaining muscle for a few weeks. We considered that the protein products might induced the occurrence of EN although there is not report in the literature. Idiopathic granulomatous mastitis (IGM) represents a rare association of EN [14]. Notably our two patients with idiopathic granulomatous mastitis were required systemic steroid and colchicine treatment for EN.
In fact, it may be extremely difficult to prove the true predictive factor in some instances. The strength of our study is in its high numbers for the condition. On the other hand, potential pitfall of this study is retrospective study design, lack of control group. Among the extensive etiologic factor list, new onset of EN after receiving vaccination is not common, but in the literature there are reported cases following vaccination for tetanus, diphtheria, and acellular pertussis (Tdap), hepatitis B, tuberculosis, cholera, typhoid, human papillomavirus, malaria, small pox and rabies [15]. In our series of 287 patients we did not detect any case that triggered with vaccination.
CONCLUSION
In our series we could not find any precipitating factors in 57.5 % of the patients. Our data confirm that viral and bacterial infections are the leading causative factors of EN, followed by BD, pregnancy and connective tissue disease (CTD). These conditions should be investigated as part of systemic search at initial presentation. Nevertheless clinicians should be aware of uncommon precipitating conditions such as rare microbial agents, idiopathic granulomatous mastitis or food supplement. Large prospective studies are still needed for reliable results providing interactions with EN and its associations.
REFERENCES
1. Cribier B, Caille A, Heid E, Grosshans E. Erythema nodosum and associated diseases. A study of 129 cases. Int J Dermatol. 1998;37:667-72.
2. Bohn S, Buchner S, Itin P. [Erythema nodosum:112 cases. Epidemiology, clinical aspects and histopathology]. Schweiz Med Wochenschr. 1997;127:1168-76.
3. Mert A, Kumbasar H, Ozaras R, Erten S, Tasli L, Tabak F, et al. Erythema nodosum:an evaluation of 100 cases. Clin Exp Rheumatol. 2007;25:563-70.
4. Schwartz RA, Nervi SJ. Erythema nodosum:a sign of systemic disease. Am Fam Physician. 2007;75:695-700.
5. Criteria for diagnosis of Behcet’s disease. International Study Group for Behcet’s Disease. Lancet. 1990;335:1078-80.
6. Mert A, Ozaras R, Tabak F, Pekmezci S, Demirkesen C, Ozturk R. Erythema nodosum:an experience of 10 years. Scand J Infect Dis. 2004;36:424-7.
7. Kisacik B, Onat AM, Pehlivan Y. Multiclinical experiences in erythema nodosum:rheumatology clinics versus dermatology and infection diseases clinics. Rheumatol Int. 2013;33:315-8.
8. Atanes A, Gomez N, Aspe B, de Toro J, Grana J, Sanchez JM, et al. [Erythema nodosum:a study of 160 cases]. Med Clin (Barc). 1991;96:169-72.
9. Oz A, Adim S, Izol B, Saricaoglu H, Baskan E, Tunali S. Erythema nodosum epidemiology:5-years Retrospective Study. Turk J Dermatol. 2012;6:87-90.
10. Ad?şen E, Şeker Ü, Gürer MA. Etiologic Factors In Erythema Nodosum. Turkderm. 2008;42:113-7.
11. Psychos DN, Voulgari PV, Skopouli FN, Drosos AA, Moutsopoulos HM. Erythema nodosum:the underlying conditions. Clin Rheumatol. 2000;19:212-6.
12. Garcia-Porrua C, Gonzalez-Gay MA, Vazquez-Caruncho M, Lopez-Lazaro L, Lueiro M, Fernandez ML, et al. Erythema nodosum:etiologic and predictive factors in a defined population. Arthritis Rheum. 2000;43:584-92.
13. Yang SG, Han KH, Cho KH, Lee AY. Development of erythema nodosum in the course of oestrogen replacement therapy. The British journal of dermatology. 1997;137:319-20.
14. Fruchter R, Castilla C, Ng E, Pomeranz MK, Femia AN. Erythema nodosum in association with idiopathic granulomatous mastitis:a case series and review of the literature. J Europ Acad Dermatol Venereol. 2017;31:e391-e3.
15. Cohen PR. Combined reduced-antigen content tetanus, diphtheria, and acellular pertussis (tdap) vaccine-related erythema nodosum:case report and review of vaccine-associated erythema nodosum. Dermatol Ther (Heidelb). 2013;3:191-7.
16. Giam YC, Ong BH, Tan T. Erythema nodosum leprosum in Singapore. Ann Acad Med Singapore. 1987;16:658-62.
17. Aydin-Teke T, Tanir G, Bayhan GI, Metin O, Oz N. Erythema nodosum in children:evaluation of 39 patients. Turk J Pediatr. 2014;56:144-9.
Notes
Source of Support: Nil
Conflict of Interest: None declared.

Comments are closed.