Prevalence and determinants of eczema among females aged 21 to 32 years in Jeddah city – Saudi Arabia
Sultana T. Binyamin1, Fathi Algamal1, Amani N. Yamani1, Mai S. Labani1, Fatenah H. Alaqbi1, Anhar A. Baeshen1, Abdulelah T. Binyamin1, Mohammed T. Al-Nazzawi2, Shahad M. Alamoudi1, Mohammed A. Aljunaid3, Lamis F. Basaeed4, Ahmed H. Alhasan3, Alanoud M. Al-Marzoug5
1Faculty of Medicine, Ibn Sina National College, Jeddah, Saudi Arabia; 2Faculty of Medicine, Batterjee Medical College, Jeddah, Saudi Arabia; 3Faculty of Medicine, University of Jeddah, Jeddah, Saudi Arabia; 4Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia; 5Faculty of Medicine, King Saud bin Abdul-Aziz University for Health Sciences, Riyadh, Saudi Arabia
Corresponding author: Dr. Sultana T.Binyamin, E-mail: sultanaalnahdi@hotmail.com
Submission: 25.05.2016l; Aceptance: 15.07.2016
DOI: 10.7241/ourd.20171.05
ABSTRACT
Introduction: Atopic dermatitis (AD) is a common, chronic an inflammatory skin disease with early onset and with a lifetime prevalence of approximately 20%. Although the pathogenesis of the disorder is not completely understood, it appears to result from the complex interplay between defects in skin barrier function, environmental and infectious agents, and immune abnormalities.
Aim: To investigate the prevalence and determinants of Eczema among Saudi female aged 21 to 32 years old in Jeddah city.
Methods: A cross sectional study involved 190 female students from IbnSina National College for Allied Health Sciences in Jeddah city were chosen by convenient sampling. Data were collected by Interview questionnaire (ISAAC: Core Questionnaire for Asthma, Rhinitis and Eczema) after getting their consent. SPSS used for data entry and analysis.
Results: Prevalence of eczema among medical college females was 16.6%, Eczema was similar in Saudi and Non-Saudi females (13.97% and 12.66% respectively, P = 0.545). Eczema was associated with eye allergy (34.2%) with statistical significance P = 0.003. Eczema was associated family members history with statistical significance P = 0.012. There was not statistical significant relationship between eczema and education level, parental jobs, drugs chest and nose allergy.
Conclusion: Prevalence of eczema among female medical students was 16.6%. Eczema was significantly associated with eye allergy and Family history of skin allergy was risk factor of eczema.
Key words: Prevalence; Determinants; Eczema; Females; Saudi Arabia
INTRODUCTION
Eczema or Atopic Dermatitis is a chronic pruritic inflammatory skin disease that occurs most frequently in children, but also affects adults. Eczema is often associated with elevated serum level of immunoglobulin E and a personal or family history of atopy, which describes a group of disorders that includes eczema, asthma, and allergic rhinitis [1,2]. Although sensitization to environmental or food allergens is clearly associated with the Eczema phenotype, it does not seem to be a causative factor but may be a contributory factor in a subgroup of patients with severe disease [3].
Epidemiology
Eczema affects approximately 5 to 20 percent of children worldwide [4]; in the United States, it is approximately 11 percent [5]. Data on prevalence of Eczema in adults are limited and in most cases based upon self-administered questionnaire information. In a Danish population-based study including approximately 16,500 adults aged 30 to 89 years, the 1-year prevalence of atopic eczema was 14 percent [6]. In a in West Sweden study of approximately 30,000 individuals aged 16 to 75 years, the current eczema prevalence was 11 percent [7]. In a Danish cohort study including approximately 1300 individuals aged 28 to 30 years who had been followed-up for 15 years, 10 percent reported atopic dermatitis, but 6 percent were found to have atopic dermatitis at clinical examination [8]. The incidence of Eczema appears to be increasing. It may occur in any race or geographic location, although there appears to be a higher incidence in urban areas and developed countries, especially Western societies. A systematic review of epidemiologic studies performed between 1990 and 2010 found an increasing trend in incidence and prevalence of atopic eczema in Africa, eastern Asia, western Europe, and parts of northern Europe [9]. In the vast majority of cases, Eczema has an onset before age five years, and prevalence data in children show a slight female to male preponderance (1.3 to 1) [10].
Risk Factors
A family history of atopy (eczema, asthma, or allergic rhinitis) and the loss-of-function mutations in the filaggrin (FLG) gene, involved in the skin barrier function, are major risk factors for Eczema [11]. Approximately 70 percent of patients have a positive family history of atopic diseases. Children with one atopic parent have a two- to threefold increased risk of developing Eczema, and the risk increases to three- to fivefold if both parents are atopic [2]. Although 30 to 80 percent of patients with Eczema are sensitized to certain foods, the timing of solid food introduction or food avoidance strategies in pregnant or nursing women does not appear to influence the risk of Eczema [12].
Although 30 to 80 percent of patients with atopic dermatitis are sensitized to certain foods, the timing of solid food introduction or food avoidance strategies in pregnant or nursing women does not appear to influence the risk of atopic dermatitis [13].
There is evidence from a 2011 systematic review to support an inverse relationship between atopic dermatitis and exposure to endotoxin, early day care, farm animal, and dog pets in early life (the “hygiene hypothesis”) [14].
A multiplicity of factors, including skin barrier abnormalities, defects in innate immunity response, Th2-skewed adaptive immune response, and altered skin resident microbial flora are involved in the pathogenesis of atopic dermatitis [15,16]. Whether skin inflammation is initiated by skin barrier dysfunction (“outside-in” hypothesis) or by immune dysregulation (“inside-out” hypothesis) is still in debate.
The epidermis is the first line of defense between the body and the environment. The skin barrier keeps environmental irritants, allergens, and microbes from entering the body and prevents excessive water loss. The barrier function of the skin is primarily located in the stratum corneum, which consists of vertical stacks of anucleatecorneocytes packed with keratin filaments embedded in a matrix of filaggrin breakdown products [17]. The corneocyte layers are embedded in an extracellular matrix replete with multiple lamellar bilayers enriched in ceramides, cholesterol, and free fatty acids derived from secreted lamellar body precursor lipids [18].
Clinical Manifestations
Dry skin and severe pruritus are the cardinal signs of Eczema. However, the clinical presentation is highly variable, depending upon the patient’s age and disease activity.
Acute eczema is characterized by intensely pruritic erythematous papules and vesicles with exudation and crusting, whereas subacute or chronic lesions present as dry, scaly, or excoriated erythematous papules. Skin thickening from chronic scratching (lichenification) and fissuring may develop over time. In many patients, lesions in different stages may be present at the same time.
Most patients with Eczema have a cutaneous hyperreactivity to various environmental stimuli, including exposure to food and inhalant allergens, irritants, changes in physical environment (including pollution, humidity, etc), microbial infection, and stress [19].
Diagnosis
The diagnosis of Eczema is clinical, based upon history, morphology and distribution of skin lesions, and associated clinical signs [2]. The United Kingdom working group on Eczema published criteria for diagnosing Eczema that include one mandatory and five major criteria [20,21]: Evidence of pruritic skin, including the report by a parent of a child rubbing or scratching. In addition to itchy skin, three or more of the following are needed to make the diagnosis:
- History of skin creases being involved. These include: antecubital fossae, popliteal fossae, neck, areas around eyes, fronts of ankles.
- History of asthma or hay fever (or history of atopic disease in a first-degree relative for children <4 years of age).
- The presence of generally dry skin within the past year.
- Symptoms beginning in a child before the age of two years. This criterion is not used to make the diagnosis in a child who is under four years old.
- Visible dermatitis involving flexural surfaces. For children under four years of age, this criterion is met by dermatitis affecting the cheeks or forehead and outer aspects of the extremities.
Skin biopsy and laboratory testing, including IgE levels, are not used routinely in the evaluation of patients with suspected Eczema and are not recommended. However, in selected patients, histologic examination of a skin biopsy or other laboratory tests (eg., serum immunoglobulin E, potassium hydroxide preparation, patch testing, genetic testing) may be helpful to rule out other skin conditions [2].
Treatment
Patients with Eczema do not usually require emergency therapy, but they may visit the emergency department for treatment of acute flares caused by eczema herpeticum and bacterial infections. Topical steroids are currently the mainstay of treatment. In association with moisturization, responses have been excellent [22].
Aim of the Study
Overall objective
The main objective of the present study was to investigate the prevalence and determinants of Eczema among Saudi female aged 21 to 32 years old in Jeddah city.
Specific objective
- To study the relationship between the family characteristic and the occurrence of Eczema.
- To study the relationship between the home characteristics of the studied females and the occurrence of Eczema.
- To study the relationship between the family history of Eczema and the occurrence of Eczema in the studied females.
- To study the relationship between the personal characteristics of the studied females and the occurrence of Eczema.
- To study the association between Eczema and the occurrence of Eczema and Bronchial Asthma.
MATERIALS AND METHODS
Study Design
A cross sectional study design.
Subjects and Study Setting
Study involved 228 university female students from IbnSina National College for Allied Health Sciences.
Sampling Techniques
A convenient sampling used and the size of the sample was determined according to the following criteria: Alpha=0.05, Beta=0.2 with moderate size effect.
Tools for Data Collection
Personal, social and environmental questionnaire, which provided information about the family characteristics, but the home circumstances and personal details of the studied female. Data were collected using ISAAC: Core Questionnaire for Asthma, Rhinitis and Eczema.
Statistical Analysis
The collected data were coded and typed on a computer file using the SPSS statistical package version 22 IBM for PC. Data was presented as tables and figures. Data was analyzed using statistical test of significance tests: Chi square test, and level of significance for the present study was chosen as 5% (a=.05).
RESULTS
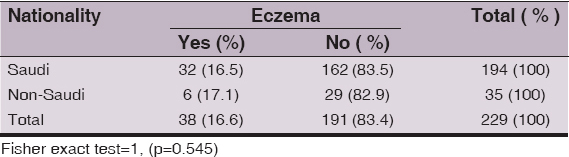
The prevalence of eczema among medical college females was 16.6%, Eczema was similar in Saudi and Non-Saudi females (13.97% and 12.66% respectively). This difference was not statistically significant where Fisher’s exact test was 1, (P = 0.545) (Table 1).
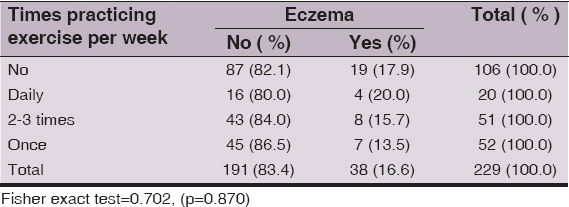
The highest proportion of eczema was among daily times practicing exercise per week (20%). This difference was not statistically significant where Pearson Chi-Square 0.702, P = 0.870 (Table 2).
The highest proportion of eczema among suffer from eye allergy (34.2 %) This difference was statistically significant where Pearson chi- square = 10.216, P = 0.003 (Table 3).
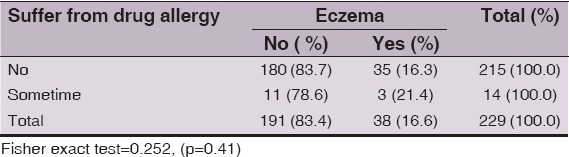
The highest proportion of eczema among suffer from drug allergy (21,4 %) This difference was not statistically significant where Pearson chi- square 0.252, P = 0.419 (Table 4).
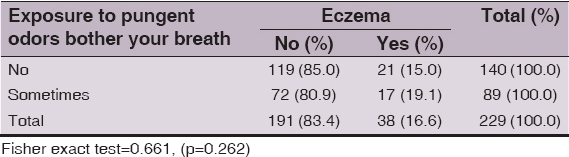
The Eczema was higher in females students who exposure to pungent odors bother her breath (19.1%) and females students who exposure to pungent odors do not bother her breath. This difference was not statistically significant where Fisher’s exact test was 0.661, and P = 0.262 (Table 5).
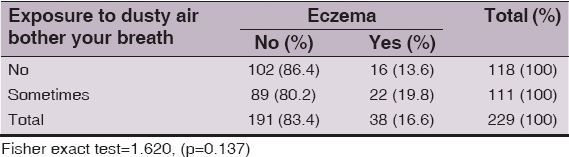
The Eczema was higher in females students who exposure to dusty air bother her breath (19.8%) and females who exposure to dusty air do not bother her breath. This difference was not statistically significant where Fisher’s exact test was 1.620, and P = 0.137 (Table 6).
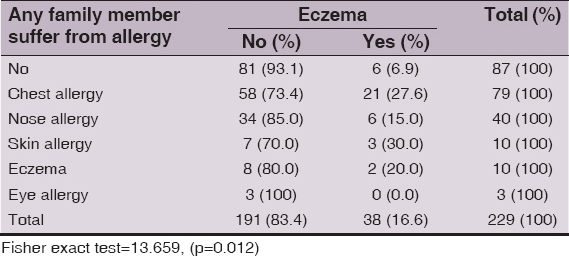
Eczema was higher in females students who their family member suffer from allergy (30.0%) and females students who their family member do not suffer from This difference was statistically significant where Fisher’s exact test was 13.659, and P = 0.012 (Table 7).
Eczema was higher in females students who have been diagnosed before of having chest allergy, nose allergy and eczema (26.3%) and female students who have been not diagnosed having chest allergy, nose allergy and eczema. This difference was not statistically significant where Fisher’s exact test was 5.599, and P = 0.133 (Table 8).
Ethics
This study was performed on human subjects; thus, all patients were aware of the presence of the study and they were fully informed about the drug and its side-effects.
CONCLUSION
Eczema was significantly associated with eye allergy and Family history of skin allergy was risk factor of eczema
Recommendations
Student with eye allergy and family history of skin allergy should be screened for eczema.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Spergel JM, From Eczema to asthma:the atopic marchAnn Allergy Asthma Immunol 2010; 105: 99-
2. Eichenfield LF, Tom WL, Chamlin SL, Krol A, Paller AS, Schwarzenberger K, Guidelines of care for the management of Eczema:section 1. Diagnosis and assessment of EczemaJ Am AcadDermatol 2014; 70: 338-51.
3. Williams H, Flohr C, How epidemiology has challenged 3 prevailing concepts about EczemaJ Allergy ClinImmunol 2006; 118: 209-13.
4. Strachan D, Sibbald B, Weiland S, Aït-Khaled N, Anabwani G, Anderson HR, Worldwide variations in the prevalence of symptoms of atopic eczema in the International Study of Asthma and Allergies in ChildhoodJ Allergy ClinImmunol 1999; 103: 125-
5. Shaw TE, Currie GP, Koudelka CW, Simpson EL, Eczema prevalence in the United States:data from the 2003 National Survey of Children’s HealthJ Invest Dermatol 2011; 131: 67-73.
6. Vinding GR, Zarchi K, Ibler KS, Miller IM, Ellervik C, Jemec GB, Is adult atopic eczema more common than we think?- A population-based study in Danish adultsActa Derm Venereol 2014; 94: 480-
7. Rönmark EP, Ekerljung L, Lötvall J, Wennergren G, Rönmark E, Torén K, Eczema among adults:prevalence, risk factors and relation to airway diseases. Results from a large-scale population survey in SwedenBr J Dermatol 2012; 166: 1301-8.
8. Deckers IA, McLean S, Linssen S, Mommers M, van Schayck CP, Sheikh A, Investigating international time trends in the incidence and prevalence of atopic eczema 1990-2010:a systematic review of epidemiological studiesPLoS One 2012; 7: e39803-
9. Kang K, Polster AM, Nedorost St Eczema, Bolognia JL, Jorizzo JL, Rapini RP, Dermatology 2003; New York: Mosby; 199-
10. Sandström MH, Faergemann J, Prognosis and prognostic factors in adult patients with Eczema:a long-term follow-up questionnaire studyBr J Dermatol 2004; 150: 103-
11. Irvine AD, McLean WH, Leung DY, Filaggrin mutations associated with skin and allergic diseasesN Engl J Med 2011; 365: 1315-27.
12. Kramer MS, Kakuma R, Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the childCochrane Database Syst Rev 2012; 9: CD000133-
13. Flohr C, Yeo L, Eczema and the hygiene hypothesis revisitedCurr Probl Dermatol 2011; 41: 1-34.
14. Kuo IH, Yoshida T, De Benedetto A, Beck LA, The cutaneous innate immune response in patients with EczemaJ Allergy ClinImmunol 2013; 131: 266-78.
15. Boguniewicz M, Leung DY, Eczema:a disease of altered skin barrier and immune dysregulationImmunol Rev 2011; 242: 233-
16. Elias PM, Wakefield JS, Mechanisms of abnormal lamellar body secretion and the dysfunctional skin barrier in patients with EczemaJ Allergy ClinImmunol 2014; 134: 781-
17. Feingold KR, Elias PM, Role of lipids in the formation and maintenance of the cutaneous permeability barrierBiochim Biophys Acta 2014; 1841: 280-94.
18. Leung DY, New insights into Eczema:role of skin barrier and immune dysregulationAllergol Int 2013; 62: 151-
19. Brandner JM, Zorn-Kruppa M, Yoshida T, Moll I, Beck LA, De Benedetto A, Epidermal tight junctions in health and diseaseTissue Barriers 2015; 3: e974451-
20. Seidenari S, Giusti G, Objective assessment of the skin of children affected by Eczema:a study of pH, capacitance and TEWL in eczematous and clinically uninvolved skinActaDermVenereol 1995; 75: 429-33.
21. Kelleher M, Dunn-Galvin A, Hourihane JO, Murray D, Campbell LE, McLean WH, Skin barrier dysfunction measured by transepidermal water loss at 2 days and 2 months predates and predicts Eczema at 1 yearJ Allergy ClinImmunol 2015; 135: 930-5.
22. Flohr C, England K, Radulovic S, McLean WH, Campbel LE, Barker J, Filaggrin loss-of-function mutations are associated with early-onset eczema, eczema severity and transepidermal water loss at 3 months of ageBr J Dermatol 2010; 163: 1333-6.
Notes
Source of Support: Nil
Conflict of Interest: None declared.


Comments are closed.