|
Get Citation
|
|
|
Gupta M. Maduromycosis of foot. Our Dermatol Online. 2017;8(1):92-93. |
|
|
Download citation file:
|
Maduromycosis of foot
Mrinal Gupta
Consultant Dermatologist, Treatwell Skin Centre, Jammu, India
Corresponding author: Dr Mrinal Gupta, E-mail: drmrinalgupta@yahoo.com
Submission: 13.05.2016; Acceptance: 16.08.2016
DOI: 10.7241/ourd.20171.23
Maduromycosis is a progressive granulomatous infection of the skin and subcutaneous tissues which may involve muscle and bone. Mycetoma pedis (mycetoma of the foot), the most common form of mycetoma, is known widely as the Madura foot. The infection is endemic in Africa, India and South Americas and Madurella mycetomatis is the most prevalent cause of mycotic mycetoma worldwide. The characteristic clinical presentation includes a triad of tumor like swelling, draining sinuses, and macroscopic grains [1]. Infection usually follows a traumatic inoculation of the pathogen into subcutaneous tissue via contaminated mechanical vectors. This infection can spread and involve fascia, muscle, bone and regional lymph nodes [2]. Mycetoma requires long-term treatment, consisting of a combination of surgical procedures and prolonged medical therapy. In the absence of a correct diagnosis and appropriate treatment, mycetoma can lead to significant morbidity due to bone destruction and deformities [3].
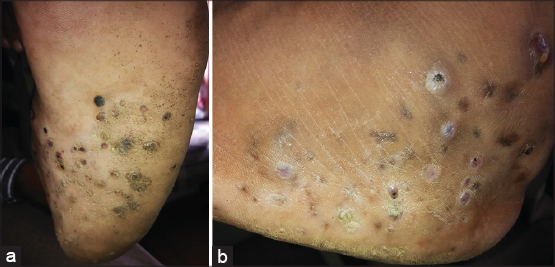
A 45 year old male presented to us with 5 years history of gradually progressive swelling and painful nodular lesions over the plantar and lateral aspect of his right foot. The lesions were a single nodule to begin with, but over the time, they had increased in size and number to their present size, and there was history of intermittent purulent discharge and crusting over these nodules. He did not recall any predisposing injury and did not suffer from systemic symptoms. On physical examination, the patient had a large swelling in the dorsum of his right foot with multiple crusted nodules and sinuses draining purulent fluid (Fig. 1a and b). There was no lymphadenopathy. Other systems were normal.
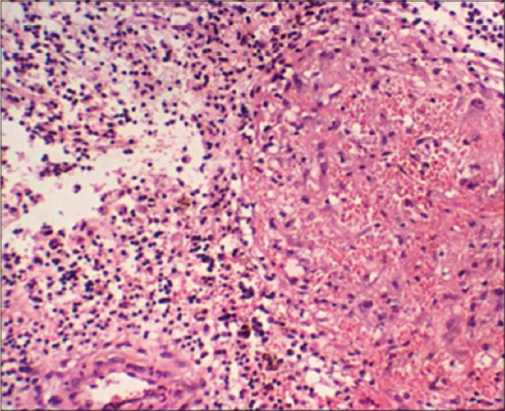
A biopsy of the lesions was done which revealed large amount of black grains, with a reactive inflammatory process surrounding the lesion (Fig. 2), which confirmed the diagnosis of Maduromycosis. The patient was treated with Itraconazole for 6 months which showed mild improvement in symptoms.
REFERENCES
1. Venkatswami S, Sankarasubramanian A, Subramanyam S, The madura foot:looking deepInt J Low Extrem Wounds 2012; 11: 31-42.
2. Ahmed AO, van Leeuwen W, Fahal A, van de Sande W, Verbrugh H, van Belkum A, Mycetoma caused by Madurella mycetomatis:a neglected infectious burdenLancet Infect Dis 2004; 4: 566-74.
3. Abd Bagi ME, Fahal AH, Sheik HE, Abdul Wahab O, Taifoor MK, Osmanr EM, Pathological fractures in mycetomaTrans R Soc Trop Med Hyg 2003; 97: 582-4.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Comments are closed.