Lupus and pulmonary nodules consistent with bronchiolitis obliterans organizing pneumonia induced by carbamazepine in a man
Awatef Kelati, Salim Gallouj, Mariame Meziane, Fatima Zahra Mernissi
Department of Dermatology of the Hospital Hassan II, Faculty of Medicine, Fez, Morocco
ABSTRACT
Several drugs have been implicated in the induction of systemic lupus erythematosus (SLE), but there are only some observations of carbamazepine induced SLE since the first case described in 1966, this drug has also been implicated in the induction of other disorders and rarely pulmonary toxicity; but the occurrence of two rare side effects of this drug: the induced SLE and pulmonary nodules consistent with the bronchiolitis obliterans organizing pneumonia in same patient is really unusual and -to our knowledge- the second observation reported in the literature.
Key words: Carbamazepine; Lupus; Bronchiolitis obliterans organizing pneumonia
INTRODUCTION
Several drugs have been implicated in the induction of systemic lupus erythematosus (SLE), but there are only some observations of carbamazepine induced SLE since the first case described in 1966 [1], this Carbamazepine (CBZ) has been used as an anticonvulsant since 1962 and is a drug of choice for treatment of simple or complex partial seizures and generalized secondary seizures in both children and adults [2,3] and which could be responsible for many side effects including sleep disorders, anorexia, nausea, vomiting, irritability, ataxia and diplopia, yet, CBZ pulmonary toxicity is rare, because only few case reports of interstitial pneumonitis, bronchospasm, pulmonary edema, pulmonary nodules and bronchiolitis obliterans organizing pneumonia (BOOP) have been reported [4–6].
Our case demonstrates two rare side effects of this drug: the induced SLE and pulmonary nodules consistent with the BOOP which is really unusual and -to our knowledge- the second observation [7] reported in the literature.
CASE REPORT
A 59 -years- old man followed since the age of 12 years for epilepsy and was under treatment by CBZ since one year.
He presented after 2 months of the use of CBZ, erythematous plaques like the butterfly wings on the face according to the patient tell and erythema on the back, the hands and feet with photosensitivity, inflammatory arthralgias and intermittent dry cough.
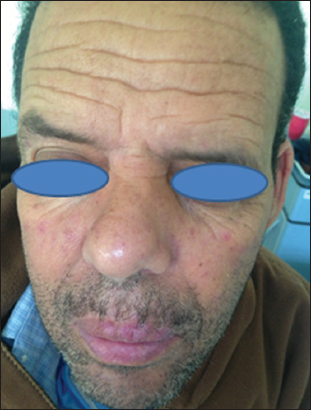
Clinical examination found bilateral malar erythematous plaques (Fig. 1) and erythematous plaques of the neckline, the back and the dorsal surface of the hands and purpuric plaques at the palmar surfaces of the hands and soles of the feet (Figs. 2 and 3) with a nibbled appearance on pulps of the fingers and erythematous alopecia patches of the scalp.
Initial Blood investigations revealed anemia (haemoglobin of 10.5 g/dl), thrombocytopenia (platelet count of 100 000/mm3), leukopenia (white cell count of 1900/mm3) and especially lymphopenia (lymphocytes count of 1000/mm3) with a positive rate of antinuclear antibodies in a titer of l/160, anti-dsDNA: 100 u/ml and positive rate of anti-histones without complement deficiency. The erythrocyte sedimentation rate and the levels of C-reactive protein were slightly increased (35 mg/L and 50 mm/h).
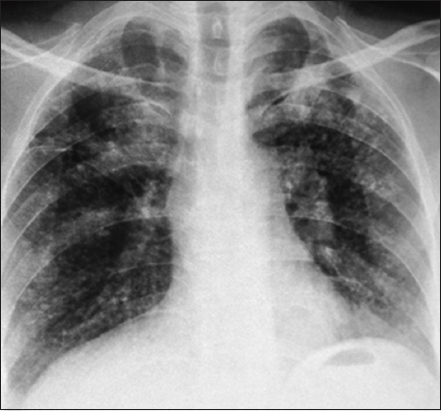
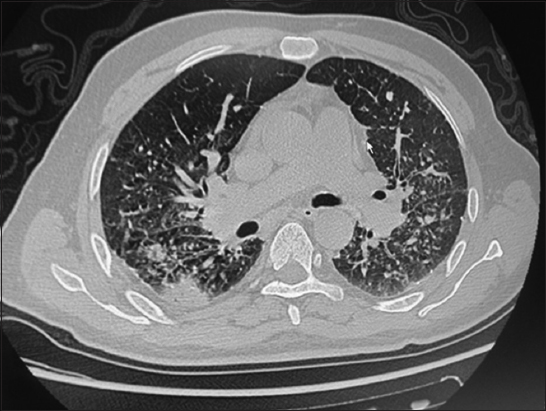
The skin biopsy confirmed the diagnosis of lupus. The chest radiography demonstrated bilateral interstitial infiltrates with multiple lung nodules (Fig. 4) more visible in the chest tomographic scan (Fig. 5), so a pulmonologist advice was asked and an infectious or occupational (silicone) origin were eliminated. The histological examination of this pulmonary infiltrate was not performed.
Ultimately, the diagnosis of CBZ induced lupus was retained based on clinical, biological and histological criteria and after the pharmacovigilance advice. In addition, the lung lesions were diagnosed as BOOP also induced by the CBZ.
Based on these facts, the CBZ was stopped and we prescribed a low dose of corticosteroids to our patient (0.5 mg/kg/j) and Hydroxychloroquine with a good evolution.
DISCUSSION
The drug induced lupus has been known since more than 50 years. In 1945, this diagnosis was suggested by Hoffman [8] and has been described in 1952 with Hydralazine, since then, hundreds of publications have been devoted to this subject [9–11], including some cases of CBZ induced SLE since Simpson described the first case in 1966 [8,12–14].
On the other hand, BOOP is a nonspecific scarring process that occurs in response to injury of the bronchioles, it is characterized histologically by the presence of inflammatory fibrinous plugs obstructing the terminal and respiratory bronchioles (bronchiolitis obliterans) and extending into the alveolar ducts and adjacent alveoli (organizing pneumonia) [15]. It was first described in 1985 as an idiopathic entity and rarely a secondary process in several clinical settings, such as wegener granulomatosis, lymphoma or other neoplasms, bronchiectasis, acute respiratory infections, radiation treatment, or appear idiopathically [6]. BOOP has been also described in association with the use of some drugs like the acebutolol, amiodarone, cephalosporin, bleomycin, tryptophan, gold salts, barbiturates, sulfasalazine, o-penicillamine, [7] and in one case, it was described as a side effect of CBZ in a lupus patient, as the case of our patient which is the second observation reported.
Generally, both the induced lupus and the BOOP have usually a good outcome after the cessation of the drug [6], and corticosteroids improves the visceral involvement in the systemic lupus, which was the case of our patient.
CONCLUSION
The originality of our case is the rare induction of SLE and BOOP by Carbamazepine in a man, which represent another real warning regarding this drug use.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Simpson JR, “Collagen disease” due to carbamazepine (Tegretol)BMJ 1966; 2: 1434-
2. Goncalves D, Moura R, Ferraz C, Vitor AB, Vaz L, Carbamazepine-induced interstitial pneumonitis associated with pan-hypogammaglobulinemiaRespir Med Case Rep 2012; 5: 6-8.
3. Loiseau P, Carbamazepine: clinical efficacy and use in epilepsyAntiepileptic drugs 2002; 5th ed. Philadelphia: Lippincott Williams & Wilkins; 262-72.
4. Archibald N, Yates B, Murphy D, Black F, Lordan J, Dark J, Corris PA, Carbamazepine-induced interstitial pneumonitis in a lung transplant patientRespir Med 2006; 100: 1660-2.
5. Banka R, Ward MJ, Bronchiolitis obliterans and organising pneumonia caused by carbamazepine and mimicking community acquired pneumoniaPostgrad Med J 2002; 78: 621-2.
6. Tamada T, Nara M, Tomaki M, Ashino Y, Hattori T, Secondary bronchiolitis obliterans organising pneumonia in a patient with carbamazepine-induced hypogammaglobulinemiaThorax 2007; 62: 100-
7. Milesi-Lecat AM, Schmidt J, Aumaitre O, Kemeny JL, Moinard J, Piette JC, Lupus and pulmonary nodules consistent with bronchiolitis obliterans organizing pneumonia induced by carbamazepineMayo Clin Proc 1997; 72: 1145-7.
8. Hoffman BJ, Sensitivity of sulfadiazine resembling acute disseminated lupus erythematosusArch Dermatol Syph 1945; 51: 130-2.
9. Morrow JD, Schroeder HA, Perry HM, Studies on the control of hypertension by hyphex. II. Toxic reactions and side effectsCirculation 1953; 8: 829-39.
10. Le Goff P, Saraux A, Les lupus induitsRev Rhum [Ed Fr] 1999; 66: 43-8.
11. Masson C, Couchouron T, Audran M, Lupus induitsRev Rhumat 2005; 72: 168-75.
12. Molina-Ruiz AM, Lasanta B, Barcia A, Pérez-Vega E, Requena L, Drug-induced systemic lupus erythematosus in a child after 3 years of treatment with carbamazepineAustralas J Dermatol 2015; Sep30
13. Harnett DT, Chandra-Sekhar HB, Hamilton SF, Drug-induced lupus erythematosus presenting with cardiac tamponade: a case report and literature reviewCan J Cardiol 2014; 30: 247-e11-2
14. Pelizza L, De luca P, La Pesa M, Minervino A, Drug-induced systemic lupus erythematosus after 7 years of treatment with carbamazepineActa Biomed 2006; 77: 17-9.
15. Gray R.E, Bronchiolitis Obliterans Organizing PneumoniaArch Intern Med 2001; 161: 158-64.
Notes
Source of Support: Nil
Conflict of Interest: None declared.


Comments are closed.