The limberg flap reconstruction – the optimal surgery for pilonidal sinus disease
Ramu Shapur Srihari, Appaji Mandya Naveen, Harinatha Sreekar
Department of General Surgery, Consultant, Plastic and Reconstructive Surgery, MVJ Medical College and RH, Hosakote, Bangalore, India
ABSTRACT
Introduction: Pilonidal sinus disease is a common condition usually seen in young adults causing significant morbidity. Many methods have been employed for its management but are also associated with high complications. Our study analyzes the efficiency of rhomboid excision of sinus and its tract, and reconstruction with Limberg flap in the management of pilonidal sinus disease.
Materials and Methods: From July 2013 to May 2015, 46 patients were operated for pilonidal sinus disease by rhomboid excision Limberg flap reconstruction in two surgical units. Duration of operation, postoperative pain, duration of hospitalization and postoperative complications were noted. The follow up was done on an out-patient basis, every month for first three months.
Results: Out of 46 patients, 40 were male (86.9%) and 6 were females (13.04%). The mean age of presentation was 28 years (range 16–50 years). The operative time ranged from 40 to 75 minutes, mean operation time being 50 minutes. Hospitalization ranged from 3-5 days, drains were removed on postop day 2/3. The stitches were removed after 12–14 days. Four patients developed mild infection. One patient developed necrosis at the tip of the flap. One patient developed recurrent lesion after 4 months, which may be due to improper excision of the sinus. The time off-work ranged from 12 to 22 days. The mean follow-up period was 3 months.
Conclusion: Limberg flap is very effective for pilonidal disease with comparatively fewer complication, short hospitalization, lesser rates of reoccurrence, early healing and lesser time off-work. The technique can be mastered easily and provides an effective procedure for primary as well as recurrent disease. The results of this study support the wide excision and Limberg flap rotation as a preferred treatment of the disease.
Key words: Limberg flap; Pilonidal; Surgery
INTRODUCTION
Intergluteal pilonidal disease is a commonly encountered condition in adult primary care, and it causes significant morbidity. The estimated incidence is 26 per 100 000 people affecting men twice as often as women [1,2]. Pilonidal disease generally presents as a cyst, abscess, or one or more sinus tracts with or without discharge in the upper part of the natal cleft [3,4].
Etiology is uncertain but relates to the implantation of loose hair into the depth of natal crease. Other factors associated, are increased sweating with sitting and friction, poor personal hygiene, obesity, local trauma, narrowness of natal cleft [5,6]. Implantation of hair leads to infection and abscess formation later leading to discharging sinus.
The management of pilonidal sinus disease remains controversial, and gold standard treatment modality has yet to be established [7]. There has been a debate regarding the best treatment for pilonidal diseases for many years. The choice of ideal therapy should be guided by several principles – Simple to perform, Limited inpatient stay, Low recurrence rate, Minimal postoperative pain, Limited wound care, Early return to activity, Cost effective, tailored to the patient and the extent of the disease [8].
In 1946, Limberg first described a technique for closing a 60° rhombus-shaped defect with a transposition flap. It meets the entire requirement for being the ideal procedure for sacrococcygeal pilonidal sinus if performed according to appropriate surgical principles [6,9]. The advantage of this reconstruction is that it is very easy to perform and design. It flattens the natal cleft with a wide and well vascularized pedicle that can be sutured without tension. That eventually helps in maintaining local hygiene, avoids hair insertion by reducing the friction between buttocks, reducing humidity, maceration, erosions and scar formation at the natal cleft [9].
Limberg procedure is a safe and reliable technique in the treatment of sacrococcygeal pilonidal sinus disease, with low complication and recurrence rates if performed according to appropriate surgical principles [10]. This study was carried out to evaluate the advantages, results of rhomboid excision and Limberg flap reconstruction in the management of pilonidal sinus disease.
MATERIALS AND METHODS
This prospective study was conducted from July 2013 to May 2015 in two surgical centers. It includes 46 patients who were treated for pilonidal sinus disease by sinus excision and Limberg flap procedure. Incision and drainage was done for Patients who had pilonidal abscess, later underwent definitive surgery. Surgery was performed under general anesthesia or regional anesthesia. After adequate skin preparation, Patients were placed in prone jack-knife position with buttocks strapped with adhesive tapes for wide exposure. The extent of the sinus was assessed by injecting methylene blue into all sinuses to outline its cavity. The rhomboid area to be excised was marked and flap lines were mapped on the skin (Fig. 1).
The rhomboid skin incision (with each side equal in length) was deepened to the pre-sacral fascia centrally and to the gluteal fascia laterally (Fig. 2). Under the guidance of methylene blue, all sinuses were excised en-bloc without incising outpocketings of the sinus cavity.
After excision, the Limberg fasciocutaneous flap was prepared by extending the incision laterally down to the fascia of the gluteus maximus muscle (Fig. 3). The size of the prepared flap was equal to that of the rhomboid area. The fasciocutaneous flap was transposed medially to cover the rhomboid defect created by excision of the sinus without any tension.
Hemostasis was achieved by the use of electrocautery. A single multiple-hole, closed suction drain was inserted underneath the flap. Subcutaneous tissue was approximated with interrupted vicryl 2-0 suture. The skin was closed with interrupted prolene 3-0 suture (Fig. 4). Antibiotics are given for 5 days initially intravenous subsequently oral. Drain was removed after 48–72 hours. Alternate sutures were removed on 10th postoperative day (POD). Rest of the sutures were removed on the 12th POD.
Postoperatively patients’ were advised, to avoid prolonged sitting or exercise for two weeks. Hair removal either by shaving or by hair removal cream was advised for at least 1 month. Patients were followed up in OPD monthly for 6 months.
The duration of operation, postoperative pain, length of hospital stay, duration of incapacity for work, postoperative complications (infection, flap edema, wound dehiscence), and postoperative recurrence were recorded. Duration of operation was defined as the length of time between the first incision and placement of the last suture. Postoperative pain was assessed according to a visual analogue scale (VAS) from 0 (no pain) to 10 (worst pain imaginable) on the first postoperative day. Duration of incapacity for work was defined as Length of hospital stay. Duration of inability to work is defined as the time from the date of surgery to the date on which patient returned to normal activities, including employment and leisure activities.
Ethics
This study was performed on human subjects; thus, all patients were aware of the presence of the study and they were fully informed about the drug and its side-effects.
RESULTS
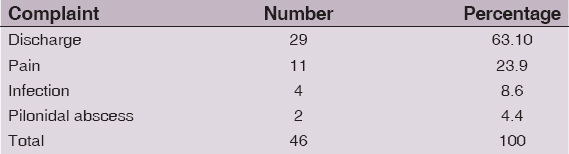
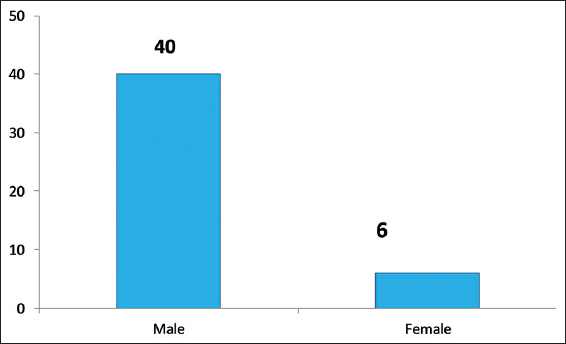
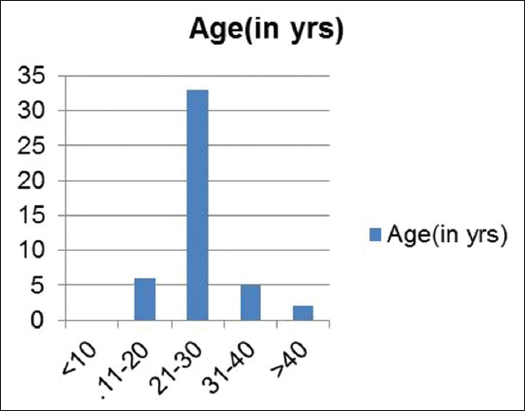
The study consisted of 40 males (86.96%) and 6 females (13.04%), with a mean age of 28 years (range 16–50 years). Mean operative time was about 50 minutes (range 40-50 minutes). The mean age of presentation was 28 years old (range 16–50 years old) Table 2. 29 patients (63.05%) presented with discharge, 11 presented with pain (23.9%), 4 with infection (8.6%) and 2 (4.3%) with pilonidal abscess Pain score, as calculated by VAS, has a mean of 3.65 (range 3-5). The mean length of hospital stay was 3.5 days (range 3 – 4 days) and most patients returned to work within 3 weeks. The distribution of patients according to demographic characteristics, history of the disease, operative time, pain score and duration of hospital stay are given in Table 1 and Figs. 5 and 6.
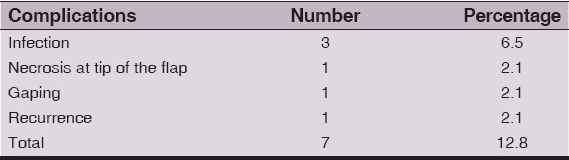
Three patients developed mild infection which was treated with antibiotics. One patient developed necrosis at the tip of the flap. One patient developed recurrent lesion 6 months postoperatively, which may be due to improper excision of the sinus (Table 2).
The stitches were removed after 12–14 days (Table 3). The time off-work ranged from 12 to 22 days. The time to walk without pain ranged from 10 to 16 days. The mean follow-up period was 4 months.
DISCUSSION
Multiple subcutaneous sinuses or abscesses containing hair characterize the disease [11]. Pilonidal sinus disease is an acquired condition affecting young adults. The etiology and pathogenesis of pilonidal sinus is still a matter of debate. Three main factors play a role in embedding of hair: Invaders formed by free hair (H-hair), the force that provides hair embedding the (F-force), and the vulnerability of the skin that lets the embedding of the hair deeper in the gluteal region (V-vulnerability) [12]. Other factors affecting the incidence are increased sweating associated with sitting and buttock friction, poor personal hygiene, obesity, and local trauma, Increase depth, narrowness of the natal cleft and the friction movements of the buttocks paves the way for loose hair to collect and insert in deep cleft [13].
The varied surgical techniques proposed for the treatment of pilonidal sinuses are evidences of the lack of an ideal procedure of management, reflecting the need for a safe and efficient surgical method for the same. The hair is perceived as a foreign body, initiates an inflammatory response and can then lead to a pocket of infection leading to abscess or sinus formation [5].
The surgical treatment should intend towards removing all the sinus tracts as well as the predisposing factors that contribute in the formation of pilonidal sinus [14].
Recurrence is the main problem associated with all surgeries described which ranged from 21.4% to 100% for incision and drainage, 5.5%–33% for excision and open-packing, 8% for marsupialization, 3.3%–11% for Z plasty [14]. The Limberg flap procedure is a safe choice for the surgical treatment of sacrococcygeal recurrent pilonidal sinus disease due to its low complication rate, short length of hospital stay, early return work, low VAS score, high patient satisfaction and shorter complete healing duration [15]. With the Limberg flap technique, internal flap cleft can be flattened and tissue can be approximated without tension.
In this study, 46 patients with sacrococcygeal pilonidal disease were managed with rhomboid excision and Limberg flap reconstruction. Recurrence was noted in one patient (2.1). Akin et al [5]. Operated on 411 patients and reported recurrence rates of 2.91%, so results were comparable to them. Superficial necrosis was seen in one patient (2.1%), which may be due to the design of the long flap or fault technique. El-khadrawy [16] operated on 40 patients and had superficial necrosis at the tip of the flap in four patients (10%). 12-18 days was Time off-work in this study which is comparable to that reported by Karaca AS et al (group II) [17].
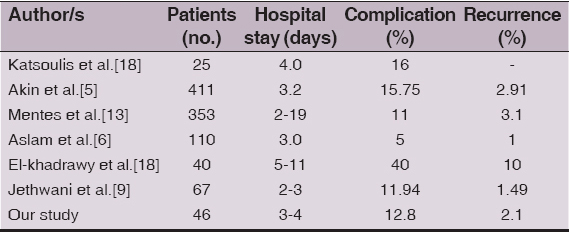
Several studies have been reported till date and results of this study are in accordance with them (Table 4) in terms of hospital stay, complication and recurrence rate.
Exercise or sitting down on the wound to be avoided for two weeks and the patient has to return slowly to normal activities. Hair removal either by shaving the edges of the wound is mandatory [14].
The advantages of Limberg flap reconstruction are:
-
Easy to perform, learn and design
-
Flattens the natal cleft with a large well-vascularised pedicle that can be sutured without tension. Midline dead space and scar is avoided. Useful in complex sinuses with multiple pits where radical excision leaves large defect.
-
Useful in recurrent pilonidal disease.
-
Reduces hospital stay and time to resume normal activities.
CONCLUSION
The study infers that “wide local excision and Limberg flap reconstruction is an effective procedure for primary and recurrent pilonidal sinus disease with low complication rates, short hospitalization, low recurrence rates, earlier healing and shorter time off-work. The surgery can be mastered easily.
The results of this study favor rhomboid excision and Limberg flap reconstruction for pilonidal disease.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. McCallum I, King PM, Bruce J, Healing by primary versus secondary intention after surgical treatment for pilonidal sinusCochrane Database Syst Rev 2007; 4: CD006213-Doi:10.1002/14651858.CDoo6213.pub 2
2. McCallum IJD, King PM, Bruce J, Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysisBMJ 2008; 336: 868-71.
3. Gul VO, Destek S, Ozer S, Etkin E, Ahioglu S, Ince M, Minimally Invasive Surgical Approach to Complicated Recurrent Pilonidal SinusCase Rep Surg 2015; 2015: 759316-
4. Steele SR, Perry WB, Mills S, Buie WD, Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for the management of pilonidal diseaseDis Colon Rectum 2013; 56: 1021-7.
5. Akin M, Gokbayir H, Kilic K, Topgul K, Ozdemir E, Ferahkose Z, Rhomboid excision and Limberg flap for managing pilonidal sinus: long-term results in 411 patientsColorectal Dis 2008; 10: 945-8.
6. Aslam MN, Shoaib S, Choudhry AM, Use of Limberg flap for pilonidal sinus–a viable optionJ Ayub Med Coll Abbottabad 2009; 21: 31-3.
7. El-Khatib HA, Al-Basti HB, A perforator-based bilobed fasciocutaneous flap: an additional tool for primary reconstruction following wide excision of sacrococcygeal pilonidal diseaseJ Plast Reconstr Aesthet Surg 2009; 62: 494-8.
8. Khanna A, Rombeau JL, Pilonidal DiseaseClin Colon Rectal Surg 2011; 24: 46-53.
9. Jethwani U, Singh G, Mohil RS, Kandwal V, Chouhan J, Saroha R, Limberg flap for pilonidal sinus disease: our experienceOA Case Reports 2013; 2: 69-
10. Dass TA, Zaz M, Rather A, Bari S, Elliptical Excision with Midline Primary Closure Versus Rhomboid Excision with Limberg Flap Reconstruction in Sacrococcygeal Pilonidal Disease: A Prospective, Randomized StudyThe Indian Journal of Surgery 2012; 74: 4305-308.doi:10.1007/s12262-011-0400-9
11. Jamal A, Shamim M, Hashmi F, Qureshi MI, Open excision with secondary healing versus rhomboid excision with Limberg transposition flap in the management of sacrococcygeal pilonidal diseaseJ Pak Med Assoc 2009; 59: 157-60.
12. Kanat BH, Sözen S, Disease that should be remembered: Sacrococcygeal pilonidal sinus disease and short historyWorld J Clin Cases 2015; 3: 876-9.
13. Mentes O, Bagci M, Bilgin T, Ozgul O, Ozdemir M, Limberg flap procedure for pilonidal sinus disease: results of 353 patientsLangenbecks Arch Surg 2008; 393: 85-9.
14. Suresh Chandu, Ramya Y, Limberg Flap Reconstruction for Pilonidal Sinus: Our ExperienceJournal of Evolution of Medical and Dental Sciences 2014; September183: 4510986-10991.DOI:10.14260/jemds/2014/3433
15. Bali ?, Aziret M, Sözen S, Emir S, Erdem H, Çetinkünar S, Effectiveness of Limberg and Karydakis flap in recurrent pilonidal sinus diseaseClinics (Sao Paulo) 2015; 70: 350-5.
16. El-khadrawy OH, The rhomboid flap for recurrent pilonidal diseaseTanta Med Sci J 2006; 1: 175-81.
17. Karaca AS, Ali R, Çapar M, Karaca S, Comparison of Limberg flap and excision and primary closure of pilonidal sinus disease, in terms of quality of life and complicationsJ Korean Surg Soc 2013; 85: 236-9.
18. Katsoulis IE, Hibberts F, Carapeti EA, Outcome of treatment of primary and recurrent pilonidal sinuses with the Limberg flapSurgeon 2006; 4: 7-10.62
Notes
Source of Support: Nil,
Conflict of Interest: None declared.











Comments are closed.