Erythema nodosum induced by kerion Celsi in a Tunisian child: A case report
Mariem Mohamed1, Marouene Belkahla1, Faten Hammedi2, Hichem Belhadjali1, Jameleddine Zili1
1Dermatology Department, Fattouma Bourguiba University Hospital, Monastir 5000, Tunisia, 2Pathology Department, Fattouma Bourguiba University Hospital, Monastir 5000, Tunisia
Sir,
Erythema nodosum (EN) is the most frequent form of acute nodular panniculitis [1]. The combination between EN and dermatophytosis of the scalp (kerion Celsi) is infrequently present in the literature [2]. We report another case of EN induced by kerion Celsi in Tunisian child.
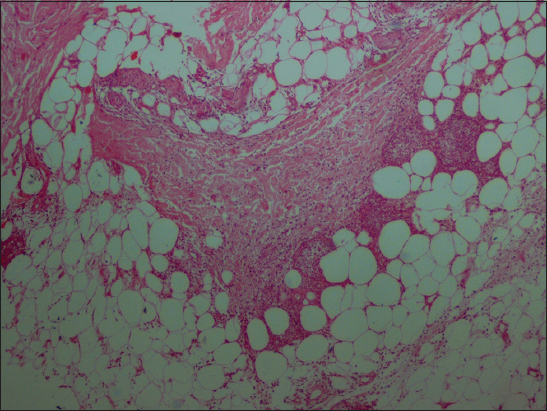
A 7-years-old boy consulted us for a scaled plaque of the scalp starting 2 weeks ago. The child used to play with the rabbits according to the mother. Dermatologic examination showed a 3 × 6 cm suppurative and scaly plaque, spangled with pustules, and located on the temporal area of the scalp (Fig. 1). Over the 2 legs, we found a multiple and painful, erythematous subcutaneous nodules (Fig. 2). Mycologic direct examination of scalp lesion showed large-spore ectoendothrix invasion of the hair fragment and Trichophyton Mentagrophites. Histologic examination of skin biopsy of leg lesion was consistent with diagnosis of EN (Fig. 3). No other causes of EN were founded allowing us to retain the diagnosis of erythema nodosum complicating kerion celsi. The child was treated by griseofulvin 20 mg/kg/day associated to econazole nitrate cream for his kerion celsi and by mefenamic acid 500 mg/day for his EN. EN lesions regressed by the 7th day and the kerion lesions resolved without sequelae by the 6th week of antifungal treatment.
Erythema nodosum is the most frequent form of acute panniculitis [1]. It can be associated to a wide variety of processes including dermatophytic infections like kerion Celsi [2]. EN complicating kerion celsi could be assimilated to a dermatophitide also called “id reaction”: a distant cutaneous allergic reaction to a fungal infection. The association between EN and kerion celsi was reported in only 15 cases (14 children and 1 woman) [2,3]. The pathogenic mechanism of this association has not been fully elucidated. Type IV hypersensibility seems to play a major role in this phenomenon. Llorente et al [4] founded increased TH1 cytokine expression in the skin lesions and peripheral blood of most of the patients with erythema nodosum compared to a control group. In the same time, it was been showed that the skin lesions produced by dermatophytic infection of zoophilic agents specifically produced by Trichophyton Mentagrophites are caused by TH1 response involved in the host defense against the dermatophytosis [5]. That could explain the predominance of Trichophyton Mentagrophites in the reported cases of EN associated to kerion Celsi, including our, (13/16 cases). On the other hand, the role of griseofulvin as causal agent of reported cases of EN associated with kerion celsi was discussed. In fact, EN occurred after the use of griseofulvin in 7 of the 15 reported cases. However, In seven other cases, as it is in our case, EN occurred before the use of griseofulvin [2]. Furthemore, improvement of EN is usually obtained using antifungal therapy.
We reported here another case of unusual association between EN and kerion Celsi, of which there are only 16 cases (including ours) in the international literature after the Second World War.
REFERENCES
1. Requena L, Requena C, Erythema nodosumDermatol Online J 2002; 8: 4-
2. Castriota M, Ricci F, Paradisi A, Fossati B, De Simone C, Capizzi R, Erythema nodosum induced by kerion celsi of the scalp in a child: a case report and mini-review of literatureMycoses 2013; 56: 200-3.
3. Zaraa I, Trojjet S, El Guellali N, El Euch D, Chelly I, Mokni M, Childhood erythema nodosum associated with kerion celsi: a case report and review of literaturePediatr Dermatol 2012; 29: 479-82.
4. Llorente L, Richaud-Patin Y, Alvarado C, Reyes E, Alcocer-Varela J, Orozco-Topete R, Elevated Th1 cytokine mRNA in skin biopsies and peripheral circulation in patients with erythema nodosumEur Cytokine Netw 1997; 8: 67-71.
5. Nakamura T, Nishibu A, Yasoshima M, Tanoue C, Yoshida N, Hatta J, Analysis of Trichophyton antigen-induced contact hypersensitivity in mouseJ Dermatol Sci 2012; 66: 144-53.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.


Comments are closed.