Circumscribed palmar hypokeratosis: Report of 2 new Ecuadorian cases, dermatoscopic description and brief literature review
Enrique Uraga1,2, Annette Morán1, Juan Carlos Garcés2
1Private Skin Center, Dr. Enrique Uraga Peña, Guayaquil, Ecuador, 2Department of Dermatology, Vernaza Luis Hospital, Guayaquil, Ecuador
ABSTRACT
The circumscribed palmoplantar hypokeratosis (CPH) is a dermatosis that is unfrequently reported around the world. It predominantly affects middle to advanced aged women, involving acral skin, asymptomatic lesions, and of unknown cause. However, its´ clinical, histopathologic and dermoscopic characteristics are distinctive. We report two cases of female patients, who come for a medical consultation presenting a long-term lesion of several years, located on the palm, asymptomatic and with no apparent cause.
Key words: Circumscribed hypokeratosis; Dermatoscopy; Cases report
INTRODUCTION
Circumscribed palmar or plantar Hypokeratosis was first described by Perez et al., in June of the 2002 [1], it refers to a rare dermatosis, characterized by an erythematous lesion, which is depressed, usually solitary, of a long-term history, asymptomatic, involving the hypothenar or thenar area of the palm and rarely, the sole [2,3] or dorsal area of the hand [4]. It mostly affects middle or advanced aged women, and its pathogenesis is not clear. Its´ histopathological characteristics consist of a well-defined depression of the epidermis. The epidermis that covers the depression shows a markedly thin stratum corneum and a thin granular layer [5], although thicker than the latter. More than 60 cases from Germany, Spain, Austria, Chile [1], Peru [5], United States, France [3], Italy, Korea, Japan, Malta, New Zeland [6] and Ecuador [7] have been reported so far.
CASE REPORT
Case 1
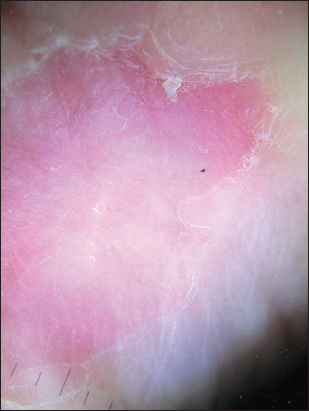
A 79-year old female, with no significant medical personal history, came for a dermatologist consultation, presenting an erythematous plaque, with superficial desquamation compatible with Actinic Keratosis localized on her right temporal region. Although on her physical examination, an oval lesion was noted, with erythematous base, loss of epidermis and sharp-cut borders, with a 2cm-diameter approximately, located on the external and palmar region of her left thumb. After inquiring the patient about this lesion, she referred a 10-year history, asymptomatic, with no previous trauma that she could recall of (Fig. 1).
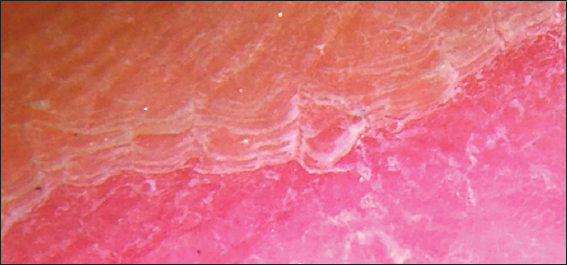
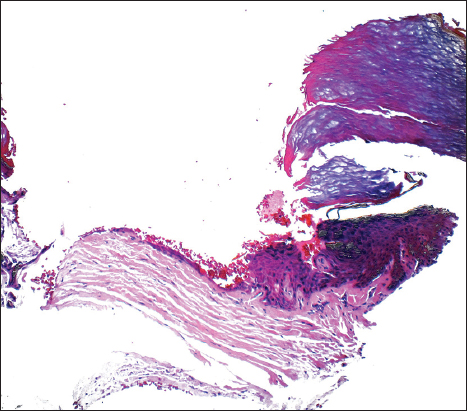
A dermatoscopy study of the lesion was realized, noticing an erythematous base with irregular borders (Fig. 2). Amplifying the dermoscopic image, showed a stair-like edge and erythematous center, speckled with white macules and red dots (Fig. 3). A histopathological study was requested due to clinical suspicion of circumscribed palmar hypokeratosis. It reported acral skin with thick corneal layer which is characteristic of the anatomical area, presence of an area with abrupt well-defined loss of the corneal layer and the underlying dermis with slight superficial perivascular infiltrate, compatible with the diagnosis of circumscribed palmar hypokeratosis (Fig. 4).
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
Case 2
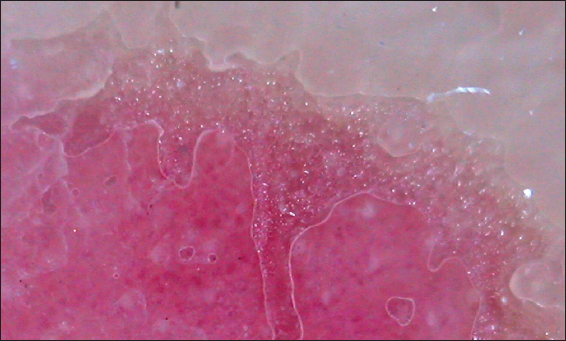
A 53-year old female, without any relevant medical history, came for a dermatologist consultation for presenting a depressed lesion, with a slightly erythematous base, irregular well-defined border, of 1 cm diameter approximately, localized on left palm, asymptomatic, with a four year history. It had not presented any particular physical change during this time and the patient does not recall any local trauma (Fig. 4). The dermatoscopy image of the lesion, showed a depressed lesion with erythematous base and keratotic borders (Figs. 5–7). There was a clinical suspicion of circumscribed palmar hypokeratosis, therefore, the histopathology was required; which confirmed the diagnosis.
DISCUSSION
Circumscribed palmoplantar hypokeratosis (CPH) was first described on 2002 by Perez et al., as an epidermic genetic disorder involving the acral regions, reporting a series of 10 patients who presented lesions with distinctive clinical and histopathological characteristics; 9 of them on the palm and 1 on the sole. Of these patients with palmar affectation, 6 of them had the lesion located on the thenar eminence, 2 of them on the hypothenar eminence and 1 of them on the palmar area of the left thumb [5]. It constitutes an independent well-characterized disorder, involving most frequently adult women, with a woman to man ratio of 4:1 [8], age may vary between 35 to 84 years old, with an average of 64.6 years old [9], and the lesions can last from 2 to 30 years [10], with an average of 12.8 years [9]. For this reason it has been categorized as an acquired disorder; although one congenital case on the United States was reported affecting an afroamerican 10-year old patient, who presented it since birth [11].
The pathophysiologic mechanism that develops CPH is not clear, Perez et al. proposed that it constitutes an epidermal benign clonal malformation, although, the late onset of the disease and the tendency to progression, suggest a proliferative dynamic disorder, without propensity to an oncogenic transformation [12]. CPH usually affects the dominant hand, which points towards a ¨forme fruste¨ of epidermolysis bullosa, with secondary lesions resulting from repetitive local trauma [13], however, just a small number of patients refer local trauma history or previous burns on the affected area [14–16].
On the other hand, Böer et al., mentioned the finding of human papilloma virus (HPV) type 4 in 2 reported cases, to which a polymerase chain reaction (PCR) was realized that suggest that CPH could be a rare morphological manifestation of common warts. Berk reported the presence of HPV type 6 in 1 of his 3 reported cases [17]. Nevertheless, the study for this virus has been done on other reported cases and the results has come up negative [10,16]. On 2007 Ishiko et al. realized immunohistochemical studies to the skin sample, from which it was found an overexpression of AE1/AE3 and diminished K9 and K2e. The expression of K16 and ki 67 did not show distinctive difference from normal nor perilesional skin, which suggests it could be associated with a keratinization disorder [10,12,18]. On 2009, Tanioka et al. proposed the existence of two subtypes of the disease. The most common one characterized by the erythematous palmar lesion, associated with diminished K6 and K16 and normal K9 immunohistochemically reported. The other subtype usually affecting the plantar region, without or hardly any erythema, associated with diminished k26 and connexin 9 expression [2]. Yamamoto et al. on 2011 advocated that it is a cell fragility disorder, due to a precipitated decomposition of desmosomes on the superior granular layer and of corneodesmosomes on the lowest corneal layer, which could be consequence of a high proteolytic activity associated with abundant Odland bodies present on this disease. These findings suggest the existence of two different pathogenic subtypes of CPH, the first one induced by an elevated corneocyte fragility and the second one caused by an abnormality on adhesion structures [14,19]. For Urbina and col., it is about a keratinization disorder expressed morphologically on the granular and corneal layers only. It consists on a reduction of keratin filaments and keratohyaline granules combined with an increased number of lipids on the corneal layer [20]. The transmission electron microscopy (TEM) does not identify abnormal mitosis or atypical cells, which supports the theory that subclinical local trauma could generate a defect during the development of the keratin [21].
Other authors noted that the hypokeratotic epidermis found on CPH could be consequence of a clonal expansion of the keratinocytes which lose the ability to differentiate towards hyperkeratotic palmoplantar keratinocytes. The exact mechanism of this referred abnormal differentiation is unknown, even so, the existence of patients suffering of multiple CPH lesions suggest some genetic predisposition to this defect [21].
CPH is also known as circumscribed acral hypokeratosis [22] and it is a chronic dermatosis, of benign progression, characterized by a lesion that shows a slow evolution or it could even remain stable throughout many years. Only 1 case of a malignant transformation of these lesions has been reported, so still a close clinical follow up is recommended [21].
Clinically, CPH typically presents a solitary skin lesion, circular, erythematous, depressed, well-defined, of 1-4cm of diameter, asymptomatic, localized on the thenar or hypothenar eminence of the hand or in the center of the sole [22,23], nonetheless a few reports exist of patients presenting multiple lesions [24], or lesions localized on the dorsal region of the fingers of the hands [4,22] or in a no acral area, such as the case of a 63 year old male presenting a lesion on his anterior thorax [7].
The diagnosis of CPH is based on the clinical features, the anatomical location, and the histopathologic characteristics of the lesion [7]. The dermatoscopy currently depicts distinctive findings. The histology describes a depression of the epidermis with a stair-like border between affected and normal skin. The epidermis that covers the depressed area, shows a thinner granular and corneal layer, if compared to perilesional skin.
The corneal layer that covers the depression is ortokeratotic with a basket basophilic pattern [1], while the adjacent area to the hypokeratosis shows a frayed pattern [12].
Exists a morphologic change of the corneocytes on the edge of the hypokeratotic area. Specifically, the superficial corneocytes show a vacuolar appearance and are basophilic; on the other hand the deeper corneocytes appear hypereosinophilia. A slight lymphocytic infiltrate surrounding the capillaries on the superficial dermis was present [12]. Groysman et al reported la existence of granular parakeratosis, local subepidermal fibin deposition and ulcers which can be related with a post traumatic skin lesion [7].
The differential diagnosis most commonly considered are Bowen´s disease and Porokeratosis of Mibelli, however the absence of atopy and cornoid lamillation void these diagnosis [24].
On dermatoscopy and microscopy with oil immersion, Nishimura et al. described the presence of ¨stair-like¨ desquamation on the borders of the lesion and well-defined erythema with scattered white macules and small red dots. The findings on the edge of the lesion correspond histologically to the thinning of the corneal layer, the erythema and red dots are consequence of the dilated capillaries on the papillary and reticular layers of the dermis, and the white macules could represent the sweat gland ducts which become accentuated because of the thinner corneal layer [25–27].
Currently there is no established treatment for this condition. Many local topical therapies have been tested; neither single nor combined therapies have been successful, getting no improvement or only partial remission. The use of corticosteroids, hydrocolloids or topical retinoid appears ineffective [26]. Urbina et al. reported healing almost completely a lesion using calcipotriol, after a 4-5 year continued treatment [20]. Dynamic Phototherapy resulted on a partial improvement after two cicles of treatment [28]. The superficial excision of the lesion is rarely done, but offers a complete cure after a 6-month follow up. Exists one reported case of a lesion being cured with the use of cryotherapy [26]. Wilk et al. informed a partial improvement on a patient being treated with topical 5-fluoruoracil for 18 months, but, the lesion reappears 3 months after discontinuing the treatment. Finally, a case of a patient with bilateral lesions was spontaneously healed [29]. On our two cases reported, we initiated treatment with topical calcipotriol, getting no improvement for three months, so both patients decided to discontinue the treatment.
CONCLUSION
To conclude, we agree with all the other authors with the fact that it is an under-diagnosed dermatosis [30]. Due to the fact that the lesion is asymptomatic, it is usually a random finding during a physical medical examination, so it is required to be attentive during the examinations as more and more cases are being reported. The distinctive dermatoscopy referred, such as the erythematous base, ¨stair-like¨ edge, white macules and red dots, become strong decisive findings for the diagnosis of this disorder. On our country, Ecuador, our cases combined with Pinos et al [7]. add up to 5 cases reported of this unusual disease.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Pérez A, Rutten A, Gold R, Urbina F, Misad C, Izquierdo MJ, Circumscribed palmar or plantar hypokeratosis: A distinctive epidermal malformation of the palms or solesJ Am Acad Dermatol 2012; 47: 1-
2. Rocha L, Menta M, Circumscribed palmoplantar hypokeratosis: report of two Brazilian casesAn Bras Dermatol 2013; 88: 623-6.
3. Baccard M, Morel P, Lésion plantaire circonscriteAnn Dermatol Venereol 2007; 134: 875-6.
4. Amakata M, Teraki Y, Case of circumscribed hypokeratosis on the dorsum of the index fingerJ Dermatol 2015; 42: 754-6.
5. García J, Catacora J, Montesinos P, Hipoqueratosis palmar circunscrita: reporte de un primer casoFolia Dermatol Peru 2005; 16: 137-9.
6. Jarrett P, Sutton T, Circumscribed palmar hypokeratosisAustral J Dermatol 2007; 48: 57-9.
7. Pinos V, Garzón E, Montegegro M, Alvarado A, Núñez M, Hipoqueratosis acral circunscritaPiel (Barc) 2014; 29: 276-9.
8. Tosi D, Sala F, Crosti C, Circumscribed palmar or plantar hypokeratosisInd J Dermatol 2011; 56: 211-3.
9. Urbina F, Pérez A, Requena L, Rutten A, Circumscribed palmar or plantar hypokeratosis 10 years after the first description: what is known and the issues under discussionActas Dermosifiliogr 2014; 105: 574-82.
10. Barry K, Glusac EJ, Kashgarian M, Gwin K, McNiff JM, Circumscribed palmar hypokeratosis: two cases and a review of the literatureJ Cutan Pathol 2008; 35: 484-7.
11. Arbesman J, Loss LC, Helm KL, Rothman I, A Congenital Case of Circumscribed Acral HypokeratosisPediatr Dermatol 2012; 29: 485-7.
12. Ishiko A, Dekio I, Fujimoto A, Kameyama K, Sakamoto M, Benno Y, Abnormal keratin expression in circumscribed palmar hypokeratosisJ Am Acad Dermatol 2007; 57: 285-91.
13. Kanitakis J, Lora V, Chouvet B, Zambruno G, Haftek M, Faure M, Circumscribed palmoplantar hypokeratosisJEADV 2011; 25: 296-301.
14. DeBloom JR, Ting W, Stone MS, Aepey CJ, Circumscribed palmar hypokeratosisJ Am Acad Dermatol 2004; 51: 319-21.
15. Riveiro-Falkenbach E, Rodríguez-Peralto JL, Circumscribed palmar hypokeratosis associated to a burn scarAm J Dermatopathol 2013; 35: 246-7.
16. Boër A, Falk TM, Circumscribed palmar hypokeratosis induced by papilloma virus type 4J Am Acad Dermatol 2006; 54: 9089-
17. Berk DR, Boer A, Bauschard FD, Hurt MA, Santa-Cruz DJ, Eisen AZ, Circumscribed acral hypokeratosisJ Am Acad Dermatol 2007; 57: 292-6.
18. Akasaka K, Maesawa C, Takahashi K, Masuda T, Akasawa T, Circumscribed palmar or plantar hypokeratosis: Two cases and a review of published workJ Dermatol 2012; 39: 314-5.
19. Yamamoto O, Yoshida Y, Adachi K, Yamada N, Abnormal cell attachment in circumscribed palmar hypokeratosis: ultrastructural observationsBr J Dermatol 2011; 164: 1395-6.
20. Urbina F, Misad C, González S, Circumscribed palmar hypokeratosis: clinical evolution and ultrastructural study after prolonged treatment with topical calcipotriolJEADV 2005; 19: 491-4.
21. Lekić B, Jankovic B, Nicolic M, Circumscribed Palmar Hypokeratosis: The first case from South-East EuropeActa Dermatovenerol Croat 2013; 21: 39-42.
22. Cribier B, Fabre F, Merlio C, Antoni N, Hypokératose acrale circonscrite: forme plantaire et forme du dos du doigt (deux cas)Ann Dermatol Venereol 2009; 136: 32-6.
23. Vives R, Valcayo AM, Hernández R, Larrinaga B, Hipoqueratosis palmar circunscritaActas Dermosifiliogr 2003; 94: 491-2.
24. Obermoser G, Zelger B, “Multifocal” circumscribed palmar hypokeratosis: Malformation or not?J Am Acad Dermatol 2003; 49: 1197-8.
25. Nishimura M, Nishie W, Nakazato S, Nemoto-Hasebe I, Fujita Y, Shimizu H, Circumscribed palmar hypokeratosis: correlation between histopathological patterns and dermoscopic findingsBr J Dermatol 2012; 167: 221-2.
26. DeBoyes T, Sherrod Q, El-Masry M, Williams EA, Chiu MW, Circumscribed palmar hypokeratosisInt J Dermatol 2012; 51: 486-7.
27. Benoit S, Seitz CS, Hamm H, Vetter-Kauczok CS, Bröcker EB, Circumscribed palmar hypokeratosis: partial remission by photodynamic therapyBr J Dermatol 2007; 157: 804-5.
28. Fueyo–Casado A, Mallo-García S, Martínez-González C, Santos-Juanes J, Circumscribed palmar hypokeratosisJ Am Acad Dermatol 2009; 61: 1090-1.
29. Wilk M, Zelger BG, Zelger B, Circumscribed Palmar Successful treatment with fluorouracil creamDermatol Ther 2011; 1: 11-4.
30. Ruíz-Villaverde R, Extremera F, Mata P, Ramírez C, Hipoqueratosis palmar circunscritaPiel 2006; 21: 413-4.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.