Dermoscopic patterns in confluent and reticulated papillomatosis: a case report
Balachandra S. Ankad, Vijay Dombale, Lakkireddy Sujana
Department of Dermatology, S N Medical College, Bagalkot, Karnataka, India
ABSTRACT
Confluent and reticulated papillomatosis (CRP) is an uncommon, progressive, distinctive dermatosis. It is characterized by persistent brown, scaly macules, papules, patches and plaques. It appears as tinea versicolor or acanthosis nigricans resulting in delay in the diagnosis. Hence a diagnostic tool which could help to diagnose this condition is dermoscopy. We reported a 24 year old male with skin lesions on upper back, neck and shoulders. Dermoscopic examination demonstrated fissures and ridges. Whitish structures were present on the ridges which are surrounded by grayish globules. These globules were lined by brown lines at the periphery. Fissures were brown in color. Global appearance was ‘crocodile skin-like’ pattern. Ridges and furrows in dermoscopy of CRP correspond to rete ridges in the histology. Whitish structures were there around follicular ostia which represent hyperkeratosis and acanthosis of follicular epidermis. Authors also observed sparse hairs in the involved area and V-sign under dermoscopy. Hence, pathogenesis of CRP probably revolves around hair follicles. CRP demonstrates specific dermoscopic patterns which correlate well with histopathologic changes. Therefore, authors propose that these patterns would aide in the diagnosis of CRP.
Key words: Acanthosis; Confluent reticulated papillomatosis; Dermoscopy; hyperkeratosis; Pathogenesis; Pattern; Whitish structures
INTRODUCTION
Confluent and reticulated papillomatosis (CRP) is an uncommon, progressive, distinctive dermatosis characterized by persistent brown, scaly macules, papules, patches and plaques [1].
CRP was first described in 1927 by Gougerot and Carteaud and it occurs predominantly in young adults and teenagers, affecting the neck, upper trunk and axillae with cosmetically displeasing appearance. Recognition of CRP is usually difficult by clinicians, including dermatologist as it frequently appears as pityriasis versicolor or acanthosis nigricans resulting in delay in the diagnosis [2]. Hence a diagnostic tool which could help to diagnose this condition is required to overcome this hurdle.
Dermoscopy is a noninvasive and quick auxiliary method that allows visualization of details of skin lesion which are subtle on examination by unaided eyes. And patterns are correlated with histopathological examination of the lesions. Thus, it is being employed commonly in clinical practice [3,4]. Therefore; dermoscopy can be utilized in the diagnosis of CRP. An attempt was made to evaluate the dermoscopic patterns in CRP. Authors believe that patterns are specific to CRP and they correlate to histopathological changes.
CASE REPORT
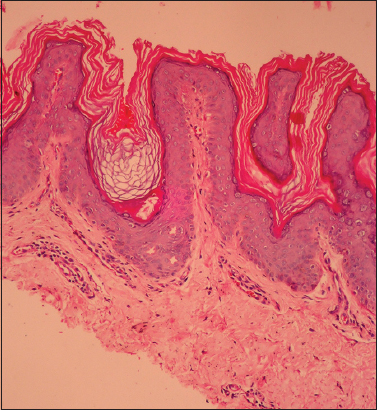
A 24 year old male presented with skin lesions on upper back, neck and shoulders since 10 months. Cutaneous examination revealed hyperpigmented, hyperkeratotic and scaly papules that coalesced into plaques in a reticulated pattern (Fig. 1). Lesions were asymptomatic. Tinea versicolor was suspected nevertheless potassium hydroxide preparation and culture for fungus was negative. Systemic examination was normal. Biochemical and hematological analyses were unremarkable. Dermoscopic examination was done using polarized dermoscopy. It demonstrated fissures and ridges. Whitish structures were present on the ridges which are surrounded by grayish globules. These globules were lined by brown lines at the periphery. Fissures were brown in color (Fig. 2). Global appearance was ‘crocodile skin-like’ pattern. A 4 mm punch biopsy was done and histopathology showed orthokeratosis, hyperkeratosis, mild acanthosis, follicular plugging and elongation of rete ridges in epidermis. There was inflammatory infiltrate surrounding hair follicle and sebaceous glands (Fig. 3). The patient was given minocycline 100 mg once daily for 8 weeks resulting in complete remission of lesions with hypopigmentation (Fig. 4). There was no relapse even after 15 months of follow up.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
CRP is an uncommon dermatological condition. The etiology is unknown, although an abnormal keratinization has been implicated and sometimes has been associated with Malassezia species. It has a chronic course with remissions and exacerbations [5]. Accepted theories suggest that this condition might be the result of an exaggerated response to fungi [6].
Differential diagnosis of CRP include benign acanthosis nigricans, pseudoacanthosis nigricans, tinea versicolor, amyloidosis and importantly all these conditions present clinically as hyperpigmented patches and plaques that spread to become confluent and reticulated [7].
Dermoscopy is a new and valuable tool providing surface and subsurface microscopic views of skin and hair. This method fills the lacunae encountered in clinical diagnosis thus increasing accuracy of diagnosis [8].
Recently, dermoscopy is gaining importance in clinical practice as it is being used widely in the field of dermatology. Inflammatory conditions such as psoriasis, lichen planus, lichen sclerosis et atrophicus demonstrate specific patterns under dermoscopy [9].
Dermoscopy of CRP is very rare in the literature. In one report, authors observed sulci and gyri under dermoscopy in one patient with CRP [4]. However; patterns were not correlated with histological changes. In this study, dermoscopy of CRP demonstrated ridges and furrows which were arranged in ‘crocodile skin-like’ pattern in global view. Ridges and furrows were due to the confluent and reticulated nature of plaques and papules. Furrows were brown in color and were not well defined at few places. They were arranged in rhomboid pattern which correspond to rete ridges in the histology. Ridges and furrows are observed in seborrheic keratosis and they are in ‘fat fingers or cerebriform’ pattern [10,11].
Whitish structures were observed in the ridges and were centered on follicular ostia. These represent hyperkeratosis and acanthosis of follicular epidermis. Whitish structures are demonstrated in hypertrophic lichen planus and correspond to compact orthokeratosis, hyperkeratosis and acanthosis [12]. In lichen sclerosus, they appear as white chrysalis strands representing homogenization of collagen in the dermis, not the hyperkeratosis and acanthosis of epidermis [9]. In pyogenic granuloma, whitish structures are in ‘white rail line’ fashion revealing fibrous septa [13]. Therefore, whitish structures under dermoscopy indicate possible pathology in integument. Furthermore, these patterns should be considered in accordance with clinical features due to their varied pathological representation as mentioned above.
Brownish lines correspond to increased melanin in the epidermis and their pattern is different in each condition [10]. In solar lentigo, they are in ‘uniform reticular’ pattern and in acral nevus; they take ‘parallel’ pattern [11]. Here in CRP, brownish lines were at the periphery of grayish globules giving a wavy or curvilinear appearance. Thus pattern of pigmentary lines in dermoscopy gives clue to the diagnosis.
Authors observed interesting hair changes in CRP. Hairs were sparse in the involved area. Two hairs were emerging out of single follicular ostium at few points which is referred to as V-sign or V-hair. This trichoscopic finding is characteristic of trichotillomania and indicates trauma and damage of hair shafts [14]. The yeast, Malassezia furfur, which is sebaceo-folliculotrophic in nature, is implicated as etiologic organism in most of the cases of CRP [5, 6]. Furthermore, there is evidence of follicular plugging in histology which clearly states that follicles are involved in the pathogenesis [1]. Based on these observations along with hair changes and whitish structures around follicular ostia observed under dermoscopy in CRP, authors are of opinion that pathogenesis of CRP probably cornered around hair follicles. Nevertheless, this is a primitive observation, further evaluation is warranted.
Histopathology of CRP shows hyperkeratosis, acanthosis, elongation of rete ridges and undulated epidermis and follicular plugging with inflammatory infiltrate in the dermis [15]. In this study, hyperkeratosis, follicular plugging, mild acanthosis, elongation of rete ridges, papillomatosis and inflammatory infiltrate were noted in histopathology. However, authors could not observe the yeast.
CONCLUSION
Dermoscopy is gradually acquiring its importance as a diagnostic aide in clinical diagnosis in recent past. CRP demonstrates specific dermoscopic patterns which correlate well with histopathologic changes. Hence, authors propose that these patterns would aide in the diagnosis of CRP and recommend usage of dermoscopy in every day practice. Since, these observation were based on single case report, further studies of CRP involving large sample size are suggested.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Rao TN, Guruprasad P, Sowjanya CL, Nagasridevi I, Confluent and reticulated papillomatosis: Successful treatment with minocyclineIndian J Dermatol Venereol Leprol 2010; 76: 725-
2. Davis MD, Weenig RH, Camilleri MJ, Confluent and reticulate papillomatosis (Gougerot-Carteaud syndrome): a minocycline-responsive dermatosis without evidence for yeast in pathogenesis. A study of 39 patients and a proposal of diagnostic criteriaBr J Dermatol 2006; 154: 287-93.
3. Micali G, Micali G, Lacarrubba F, IntroductionDermatoscopy in clinical practice-Beyond pigmented lesions 2010; 1st edn. London: Informa healthcare; 1-2.
4. Bernardes Filho F, Quaresma MV, Rezende FC, Kac BK, Nery JAC, Azulay-Abulafia L, Confluent and reticulate papillomatosis of Gougerot-Carteaud and obesity: dermoscopic findingsAn Bras Dermatol 2014; 89: 507-9.
5. Rodríguez-Carreón AA, Arenas-Guzmán R, Fonte-Avalos V, Gutiérrez-Mendoza D, Vega-Memije ME, Domínguez-Cherit J, Confluent and reticulated Gougerot-Carteaud papillomatosis: a case report of an excellent response to minocyclineGac Med Mex 2008; 144: 67-70.
6. Lee SH, Choi EH, Lee WS, Kang WH, Bang DS, Confluent and reticulated papillomatosis: a clinical, histopathological, and electron microscopic studyJ Dermatol 1991; 18: 725-30.
7. Baalbaki SA, Malak JA, al-Khars MA, Confluent and reticulated papillomatosis. Treatment with etretinateArch Dermatol 1993; 129: 961-3.
8. Tosti A, Ross EK, Tosti A, Patterns of scalp and hair disease revealed by videodermoscopyDermoscopy of hair and scalp disorders 2007; 1st edn. London: Informa healthcare; 1-14.
9. Shim WH, Jwa SW, Song M, Kim HS, Ko HC, Kim MB, Diagnostic usefulness of dermatoscopy in differentiating lichen sclerosus et atrophicus from morpheaJ Am Acad Dermatol 2012; 66: 690-1.
10. Bowling J, Bowling J, Non-melanocytic lesionsDiagnostic dermoscopy- The illustrated guide 2012; 1st edn. West Sussex: Wiley-Blackwell; 59-91.
11. Johr RH, Stolz W, Johr RH, Stolz W, Dermoscopy from A to ZDermoscopy – An illustrated self-assessment guide 2010; New York: McGraw Hill; 1-26.
12. Ankad BS, Beergouder SL, Sujana L, Dermoscopy of Hypertrophic Lichen PlanusAustin J Dermatol 2014; 1: 2-
13. Zaballos P, Carulla M, Ozdemir F, Zalaudek I, Bañuls J, Llambrich A, Dermoscopy of pyogenic granuloma: a morphological studyBr J Dermatol 2010; 163: 1229-37.
14. Rakowska A, Slowinska M, Olszewsk M, New trichoscopy findings in trichotillomania: flame hairs, v-sign, hook hairs, hair powder, tulip hairActa Derm Venereol 2014; 94: 303-6.
15. Tamraz H, Raffoul M, Kurban M, Kibbi AG, Abbas O, Confluent and reticulated papillomatosis: clinical and histopathological study of 10 cases from LebanonJ Eur Acad Dermatol Venereol 2013; 27: 119-23.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.