Erythema gyratum repense like eruption in bullous pemphigoid: A case report
Hojat Eftekhari1, Abbas Darjani1, Mojgan Nazari2, Sareh Shafaei1, Leila Yousefkhani1, Nahid Nickhah1
1Department of Dermatology, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran, 2Social Determinants of Health Research Center, Faculty of Nurse Midwifery, Guilan University of Medical Sciences, Rasht, Iran
ABSTRACT
Bullous pemphigoid (BP) is an autoimmune disease characterized by presence of bullous eruption on the trunk and extremities especially flexural aspects of the limbs. This disease usually occurs in the elderly. The initial presentation of BP is variable. An urticarial or erythematous rash may precede the appearance of the blister formation and can be associated with itch or pruritus. We presented 87 year old bedridden man diagnosed with BP who initially presented with erythema gyratum repens like eruption before blister formation. This case report discusses the presentation of figurate erythema in non-bullous phase of BP for clinicians.
Key words: Erythema; Pemphigoid; Bullous
INTRODUCTION
Bullous pemphigoid (BP) is an autoimmune bullous disease that is characterized by sub epidermal blisters on trunk and extremities and oral lesion is unusual. This disease may be signaled by urticarial or eczematous rash. Skin biopsy is the most reliable test for diagnosis. A direct immunofluorescence (DIF) shows deposition of Auto Antibodies (IgG) and complement (C3) at the dermo- epidermal junction [1,2].
The goal of this reporting is to explain variable features of non-bullous phase of BP and the association between BP and erythema gyratum repens like eruption in a 87 years old man.
CASE REPORT
A 87 years old bed ridden male admitted to hospital with chief complain of several blisters formation and pruritus. He started to have polycyclic erythema eruption at the back of the trunk since 20 days ago which was configured as Erythema gyratum repens like eruption.
The lesions were troublesome because of pruritus. Five days later, tense blisters were formed at the dorsal aspect of the right hand and were rapidly outspreaded through upper and lower extremities. He gave no history of weight loss or constitutional symptoms. His past medical history revealed cerebrovascular attack (CVA), femur fracture, dementia, BPH and nephrectomy. He was also incontinence since 3 years ago and was relatively bedridden before admission. The only drug he used was Finasteride 5 mg/day. His personal history was remarkable for cigarette smoking 60P/Y. He had no family history of cancer and skin disease.
Detailed cutaneous and mucosal examination showed erythematous plaques at the forehead and excoriated crusts on face and neck. Erythema gyratum repens like eruption was seen at the back of the trunk with typically “wood grain” appearance (Fig. 1). At the front aspect of the trunk there were multiple annular erythematous formations with crust. Multiple tense blisters and vesicles were detected all over the arms and legs (Figs. 2 and 3).
The blisters were filled with clear fluid which aroused from erythematous skin. Nikolsky sign was negative and the rest of the examination of oral cavity and genitalia did not show abnormality. In general examination lymphadenopathy was not detected. Two plus edema of right foot was seen. He had wheeze all over the lung. His left hand was spastic and in an internal rotation position due to the past history of CVA.
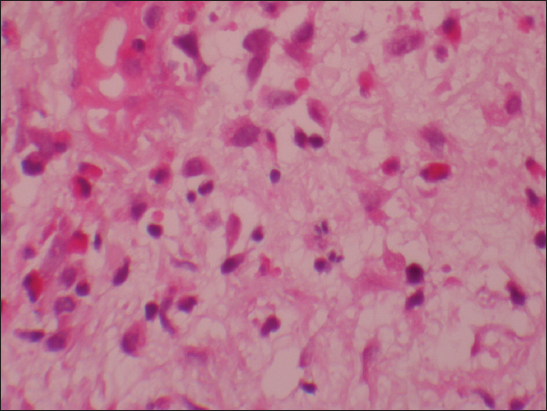
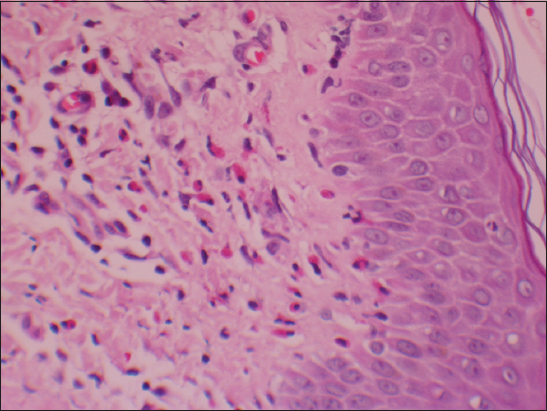
Two biopsies were taken from the bullae formation of the hand and the figurated erythema at the back.
The biopsy of the hand showed subepidermal blister containing some eosinophils (Figs. 4 and 5) with linear deposition of IgG and C3 along dermoepidermal junction and the biopsy from back lesion showed spongiotic dermatitis with eosinophils suggestive for early lesion of BP.
At the lab data he had white blood cell, 18700 cell/m3 with marked eosinophilia (23%), hemoglobin 12.4 g/dl, MCV104 fl and albumin 3 g/dl with total protein 5.6 g/dl. Other lab tests showed CRP 1+ and ESR 20. CXR was normal.
The patient was started on 30 mg Prednisolone and Clobetasol ointment for topical use. The erythema gyratum repens like eruption disappeared with the start of treatment in a few days and new blisters did not appear.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
Bullous Pemphigoid is the most common autoimmune subepidermal blister disease that typically present in elderly. Before blister formation cutaneous manifestation of BP can be extremely polymorphic and nonspecific, from mild to severe pruritus alone to eczematous, papular or urticarial lesion. This signs and symptoms can be persistent for several weeks or months alone, and may remain as the only signs of BP.
The BP has association with some situation such as internal malignancy (GI, urinary bladder, lung), lymphoprolifrative disorder, autoimmune disease (such as IBD, SLE, and Dermatomyositis), trauma and neurologic disorders (such as MS, Stroke, dementia, and psychiatric disease). Patients with Erythema gyratum repens should be considered as having malignancy and should be mandatorily evaluated.
Several studies showed the association between figurate erythema and BP. In this case erythema gyratum repens like eruption was occurred before blister formation and there were no signs and symptoms of malignancy during six month follow-up.
Gilmour et al, reported a patient with urticarial arcuate lesion in a BP patient. Further assessment showed an underlying colon cancer [3]. In contrast Reynoso et al reported a patient with BP and figurate erythema without underlying malignancy [1].
Hadi et al studied 9 case of BP with figurate erythema that three of them had underlying malignancy (bronchogenic carcinoma and colon cancer) [4].
Urano-Saehisa et al, reported a patient with BP, bizarre figurate erythematous eruption and generalized pigmentation with underlying adenocarcinoma of stomach [5].
Geraham et al, report a case with figurate erythema resembling erythema gyratum repens in a patient with BP that have bronchial carcinoma [6]. Clinical Importance: Erythema gyratum repens can be a feature of bullous pemphigoid even absence of malignancy.
ACKNOWLEDGMENT
The authors thank the staff of Razi Hospital and the patient. There is no financial support as well as no conflict of interest in this study.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Reynoso-von Drateln C, Balderrama-Vargas C, Martínez-Baumbach EB, Tinoco-Ventura E, Rodríguez-Mora E, Bullous pemphigoid with figurate erythema, a case reportRev Med InstMexSeguro Soc 2008; 46: 427-30.
2. Balakirski G, Merk HF, Mergahed M, Bullous Pemphigoid: a new look at a well-known diseaseHautarzt 2014; 65: 1013-6.
3. Gilmour E, Bhushan M, Griffiths CE, Figurate erythema with bullous pemphigoid: a true paraneoplastic phenomenonClin Exp Dermatol 1999; 24: 446-8.
4. Hadi SM, Barnetson RC, Gawkrodger DJ, Sexana U, Bird P, Merretta TG, Clinical, histologocal and immunological studies in 50 patients with Bullous pemphigoidDermatologica 1988; 176: 6-17.
5. Urano-Suehisa S, Tagami H, Yamada M, Hishiki S, Tokura Y, Bullous pemphigoid, figurate erythema and generalized pigmentation with skin thickening in a patient with adenocarcinoma of the stomachDermatologica 1985; 171: 117-21.
6. Graham-Brown RA, Bullous pemphigoid with figurate erythema associated with carcinoma of the bronchusBr J Dermatol 1987; 117: 385-8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.