Chromoblastomycosis
Patricia Chang1, Elba Arana2, Roberto Arenas3
1Department of Dermatology, Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala, 2Elective student, Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala, 3Mycology section, “Dr. Manuel Gea González” Hospital, Mexico City, Mexico
ABSTRACT
Chromoblastomycosis is a subcutaneous, chronic, granulomatous mycosis that occurs more frequently in tropical and subtropical countries. We report a case of chromoblastomycosis of the earlobe due to Fonsecaea sp in a male patient of 34 years old, due to its uncommon localization.
Key words: Chromoblastomycosis; Fonsecaea pedrosoi; Fonsecaea compacta; Cladosporium carrionii; Fumagoid cells
INTRODUCTION
The chromoblastomycosis is a sub cutaneous mycosis in tropical and subtropical areas considered as an American disease, the main agents are Fonsecaea pedrosoi, in endemic areas of tropical and subtropical environments; Fonsecaea compacta, Cladosporium carrionii. The diagnosis of the disease is through the presence of fumagoids cells.
In our environment, chromoblastomycosis is the third most common subcutaneous mycosis. It predominates in the lower limbs in warty form and F pedrosoi is the most frequent etiological agent.
CASE REPORT
Male patient, 34 years, who consulted a private doctor because of a dermatological condition in his right ear. A biopsy was performed and the report indicated a squamous cell carcinoma. The patient was sent to the oncology outpatient clinic for treatment, but as there was doubt about the histological diagnosis and the clinical picture, a second biopsy was performed that reported a granulomatous-type lesion. An inter-consultation was held at the Dermatology Service for reevaluation. Upon examination, a dermatosis was found in the ear and right facial region, made up of an atrophic squamous plate, hematic crusts and one retroauricular nodule with slightly warty appearance (Figs. 1 and 2). The rest of the physical exam was within normal limits.
The patient says that his disease started 3 years ago with a small asymptomatic “pimple” in his right ear that slowly increased its size until he decided to consult. In the last 6 months he had an occasional itch and was prescribed different antibiotics and non-specific creams. He does not remember bruising the area.
Three clinical diagnosis were made based on the clinical data: chromoblastomycosis; leishmaniasis; and sporotrichosis fixed plaque. A new skin biopsy was performed, along with a direct exam and a culture for fungus and PCR for leishmania.
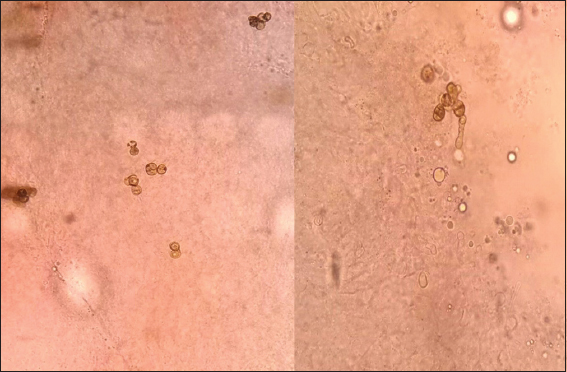
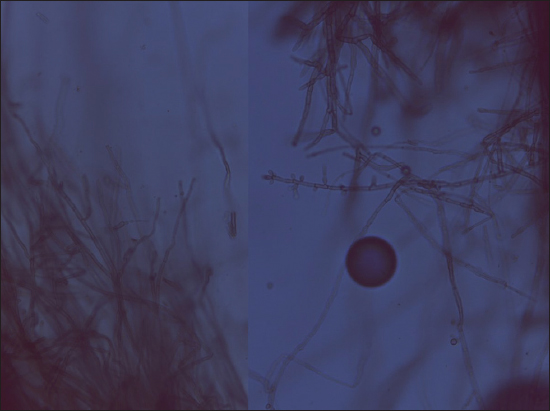
The PCR for leishmania was negative; the direct exam of the biopsy showed presence of fumagoid cells (Fig. 3), and the biopsy showed a granulomatous infiltrate with giant cells and fumagoid cells (Figs. 4 and 5). Fonsecae sp was isolated from the fungus culture (Figs. 6 and 7).

DISCUSSION
Chromoblastomycosis is a disabling granulomatous dermatomycosis of chronic evolution that affects the skin and subcutaneous tissue and localizes in the inferior limbs after a trauma, with formation of nodules and warty plates that can become ulcerated and give place to tumor masses, caused by a variety of black or dematiaceous fungus. It is observed in people who work barefoot [1,2]. It predominates in tropical and subtropical regions particularly in Latin America, although there have been cases in the five continents and therefore is considered of cosmopolite character. It has been called chromomycosis, Fonseca disease, Pedroso and Lane disease [2].
The main agents are Fonsecaea pedrosoi, in endemic areas of tropical and subtropical environments; Fonsecaea compacta, Cladosporium carrionii, in dry climates, in a lesser proportion Phialophora verrucosa, Rhinocladiella aquaspersa, Fonsecaea monophora, Fonsecaea nubica, Exophiala dermatitidis, Exophiala spinifera, Rhinocladiella richardsiae, Cladophialophora yegresii [3,4].
The term chromoblastomycosis was first used by Terra in 1922 to designate a deep subcutaneous mycosis in the lower limbs, especially feet [5]. The first case was described in 1911 by Pedroso y Sao Paulo, Brazil; in 1935, Morales publishes the first chromoblastomycosis case in Guatemala, and successively, multiple chromoblastomycosis cases have been reported in the world [2].
It is a mycosis in tropical and subtropical areas considered as an American disease. However, because of the many cases published in the world, is considered cosmopolite with predominance in the American continent. The country with the highest number of reported cases is Brazil, although the country with the highest per capita proportion is Costa Rica, which has one case per 24,000 habitants. Dominican Republic, Cuba and Puerto Rico follow by frequency order. Other countries are: México, Guatemala, Honduras, Venezuela, Colombia, Madagascar, Australia, Congo and the south of China [2,5].
In Dominican Republic more than 500 cases have been reported and all the clinical forms reported in the literature have been studied, as well as other clinical varieties [1].
The fungus live in the soil and in vegetables, in humid and hot climates with a temperature range between 25°C and 30°C [2].
It is frequent in farmers and lumberjacks. There is a traumatic inoculation of the etiological agent. It is located in the limbs -95%-, and the lower limbs -75%-, with clear predominance in the dorsal part of the foot. The remainder cases appear in the trunk, and rarely in the face or other regions of the body [3].
These fungus are dimorphic and in its parasitic phase manifest as fumagoid cells called muriform cells or sclerotic bodies; these in turn are called Medlar sclerotia.
Clinically the disease can manifest in a warty or vegetative form, as nodules, tumors, in superficial plate or as psoriasis, scars, tumors and elephantiasis. The warty form is the most frequent -53% [1,2].
The initial lesion can appear as a papule that extends in the surface and forms well-limited erythematous-scaly plates, asymmetric and unilateral. They grow slowly in the term of months; generate erythematous nodules that get covered in scales. Approximately one year after appear as extended warty or vegetative plates covered abundantly in scales, ulcers, bloody scars [6]. The size varies from one millimeter up to big plates of several centimeters. Symptomatology of the disease is variable. As the disease advances, it becomes chronic and leaves scars. Most of the patients consult one to five years after the onset of the disease, and there have been cases with 40 years of evolution [1,4].
Among the differential diagnosis are leishmaniasis, cutaneous tuberculosis, psoriasis, sporotrichosis, coccidioidomycosis, blastomycosis, squamous cell carcinoma.
Complications of the disease are added bacterial infection. In very chronic cases, warty lymphostasis and degeneration to squamous cell carcinoma and melanoma, due to the chronic swelling and fibrosis [6].
The easiest way to diagnose is direct examination. The parasite elements must be sought in fragments of the tissue and most of all in scales presenting “black dots.” Potassium hydroxide is used 10-40% in places where the fumagoid cells are in groups of two or more. These are spherical or ovoid, measure 4 to 8 microns in diameter, are yellowish/brownish in color, have a thick membrane, and on occasions have divisions or filaments. Can be compared to coffee grains. Their culture allow confirmation of the causing agent [1,2].
Histopathology is very useful in diagnosis. Sometimes it can show a suppurating granuloma that sometimes is tuberculous. At skin level there is hyperkeratosis with parakeratosis, marked irregular acanthosis that sometimes form a pseudoepitheliomatous hyperplasia. In the superficial and medium skin a granulomatous reaction with lymphocytes, plasma cells, leukocytes, giant epithelioid cells of Langhans type, and the presence brown fumagoid cells [1,2].
Treatment has been a clinical challenge in spite of modern systemic antifungals. In small lesions with little evolution, cryosurgery is recommended as long as they are not located in bending sites, as well as surgery. Some authors recommend itraconazole alone in combined with 5-fluorocistine [7].
When lesions are extended or spread 5-fluorocistine, amphotericin B itraconazole, fluconazole or terbinafine can be used, the last 3 for 6 to 12 months.
Electrodessication, radiotherapy, local heat and vitamin D are other modes of treatment.
In lesions small and of short evolution medical surgical treatment is recommended such as: itraconazole, fluconazole or terbinafine for 3 months, with cryosurgery.
Therapeutic success can be related to the etiological agent (C. carrionii is more sensitive than F. pedrosoi), with the severity of the illness (edema and skin fibrosis can reduce the reach of antifungals to the skins), and with the election of the antifungal drug. So far, there is no consensus nor standardization to establish healing criteria for this mycosis [8,9]. Head and neck lesions do not respond with the same efficacy as other regions at distal level [1].
The preventive measure, aside of avoiding traumatic inoculation of fungi is the use of closed shoes.
Prognosis will depend on the stage of the lesions and their evolution.
In our environment, chromoblastomycosis is the third most common subcutaneous mycosis. It predominates in the lower limbs in warty form and F. pedrosoi is the most frequent etiological agent.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Isa Isa R, Arenas R, Micosis Superficiales, subcutaneas y Pseudomicosis en República Dominicana 2009; Mexico: Graphimedic; 74-80.
2. Bonifaz A, Saul A, Paredes-Solis V, Araiza J, Fierro-Arias J, Treatment of chromo-blastomycosis with terbinafine: experience with four casesJ Dermatol Treat 2005; 16: 47-51.
3. Queiroz-Telles F, Esterre P, Pérez-Blanco M, Vitale RG, Vitale RG, Salgado CG, Bonifaz A, Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatmentMed Mycol 2009; 4: 1-13.
4. Spiker A, Ferringer T, ChromoblastomycosisCutis 2015; 96: 224-267; 268
5. Arenas R, Micología Médica Ilustrada 2008; 3ª edición. Mexico: McGraw-Hill; 161-73.
6. Chaabane H, Mseddi M, Charfi S, Chaari I, Boudawara T, Turki H, Chromoblastomycosis: breast solitary lesionPresse Med 2015; 44: 842-3.
7. Queiroz-Telles F, Nucci M, Colombo AL, Tobón A, Restrepo A, Mycoses of implantation in Latin America: an overview of epidemiology, clinical manifestations, diagnosis and treatmentMed Mycol 2011; 49: 225-36.
8. Kullavanijaya E, Rojanavanich V, Successfull treatment of chromoblastomycosis due to Fonsecaea pedrosoii by itroconazole and cryotherapyInt J Dermatol 1995; 34: 804-07.
9. Bonifaz A, Vázquez-González D, Saúl A, Fierro-Arias L, Ponce-Olivera MR, Refractory onychomycosis due to Trichophyton rubrum: combination therapy with itraconazole and terbinafineN Dermatol Online 2011; 2: 108-12.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.




Comments are closed.