Dermatologic challenges of health care for displaced people. lessons from a German emergency refugee camp
Uwe Wollina, Beatrix Gaber, Rahaf Mansour, Dana Langner, Gesina Hansel, André Koch
Department of Dermatology and Allergology, Academic Teaching Hospital Dresden-Friedrichstadt, Dresden, Germany
ABSTRACT
Background: The World faces the highest waves of displaced people since World War II. There is limited knowledge about need of dermatological care for refugees and asylum seekers.
Methods: We report the experience with a temporary emergency refugee camp in Dresden form the viewpoint of a hospital department. This is a descriptive report covering the period of 10 weeks.
Results: In this refugee camp up to 1 100 people were hosted. The male to female ratio was 5.3. The majority of inhabitants were young males (60%), 20% were children. While 40% of refuges came from Syria, Afghanistan, Iraq and Pakistan were also important countries of origin. Communication war a crucial issue while providing health care. Dermatologic service was granted as consultation, outpatient and inpatient clinic. Most contacts were noted in the outpatient clinic. The majority of patient attended the clinic with communicable diseases such as bacterial or viral infections and infestations. Wounds and chronic inflammatory diseases were rather uncommon. Only 4 patients had to be treated in the hospital (inpatient clinic).
Conclusions: Displaced people (refugees, asylum seekers) come in big waves to Europe. Dermatologic service is an important part of first aid health care in an emergency camp. Language barriers and cultural barriers have to overcome for optimal service. This is the first report from Germany.
Key words:Refugee camp; Dermatology; Leishmaniasis; Scabies; Communicable diseases; Service
INTRODUCTION
For the first time since 1999 Germany was the World’s largest recipient of individual asylum application [1]. This has a manifold impact on society and last not least on health care. Health care is regulated by law and this is also the case for asylum seeker, i.e. national Law on Services for Asylum Seekers (AsylBLG sections 4 and 6). Health care service based on this law is free for asylum seekers.
Since the German health care system does not collect data on health status and health care provision to asylum seekers important data are missing to deal with this growing problem for planning organizing and optimizing health care efforts [2]. Searching on PUBMED® we could identify a single paper on dermatologic problems in asylum seekers from Turkey [3] but none from Germany.
Therefore, we present here an empiric study from Dresden, Germany.
MATERIAL AND METHOD
The increasing numbers of asylum seekers coming from Syria, Iraq, Libya, Eritrea, Afghanistan, Pakistan and Eastern Europe has been a challenge for Europe and in particular for Germany. This has resulted in emergency situations to provide shelter for asylum seekers. On July 23rd, 2015 the German Red Cross (DRK) and the Federal Agency for Technical Relief (THW) established overnight a temporary Refugee Camp with 33 tents, where during the following weeks until October 9, 2015, up to 1,100 asylum seekers found shelter. Each tent had space for about 30 people which translates into 1.5 m2 per person. Due to the circumstances, no systematic preparation of the health care needs was possible. The first local service was provided within the camp by volunteers. With some delay a stable arrangement of first aid services in the camp could be established.
The nearest hospital was the Hospital Dresden-Friedrichstadt, where the Department of Dermatology and Allergology provided dermatologic support. Initially the hospital was the only professional provider of health service except for volunteers. The circumstances caused an additional work load for nurses and doctors mainly in the morning and night shift. Patients usually were companioned by several other people. Health services were free for the asylum seekers.
The major cause for consultations, in- and outpatient treatment was communicable disorders (bacterial and viral infections, scabies and mycosis) in our setting.
Demographics of asylum seekers
On average 60% of asylum seekers were adult males, 20% adult females and 20% children and adolescents. The male to female ratio of all asylum seekers was 5.3. 46% of asylum seekers were married, 11% unmarried, and in 6% the status was unknown.
About 40% of asylum seekers came from Syria, 15% from Afghanistan, 10% from Iraq, 5% from Pakistan, and 30% of various other countries.
Dermatologic service
Dermatologic service was provided as counselling, outpatient treatment and inpatient treatment. Dermatologic service was requested in 19% of all asylum seekers treated by the hospital. Consultations were ordered 8 times for scabies (2x), skin ulcers (2x), Varicella (1x), allergic sting reaction (1x), acute urethritis (1x), and xerosis cutis (1x).
A significant issue is availability of interpreters. English was not spoken by many of the refugees, Arabic interpreters were available. More difficult was communication with people speaking Dari, Pashto, Urdu or Tigrinya. Interpreters were generated from hospital staff and municipal interpreter service (Gemeinde-Dolmetscherdienst).
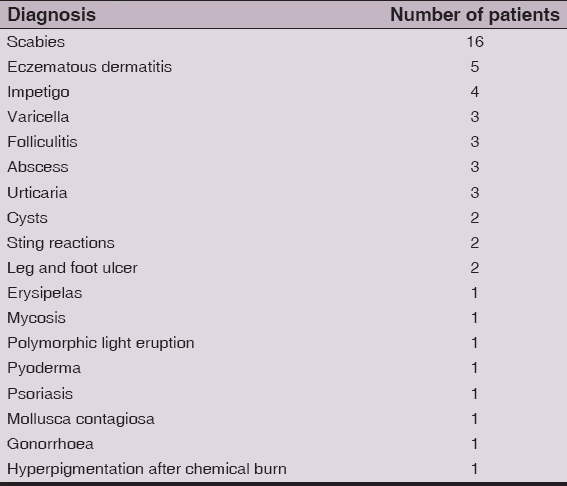
Outpatient care was the dominant type of service engaged. We saw 52 patients with a wide range of skin diseases. The leading diagnosis was scabies (16x), followed by eczematous dermatitis (5x), and impetigo (4x). About 65% of outpatient diagnoses were infectious diseases and infestations. For further details see Table 1.
Follow-up was realized by the Health Service that had been established in the refugee camp later. After closure of the tent camp and accommodation of refugees in houses, a central outpatient health service was opened in Dresden (https://www.slaek.de/de/01/03Empfehlungen/08Asylbewerber.php).
Inpatient treatment
Only 4 patients needed an inpatient treatment. Three of them had infectious diseases (Varicella, cheek abscess, impetiginized eczema). The other patient suffered from anaphylaxis after an insect sting.
DISCUSSION
There are currently more displaced people around the world since 2nd World War. This has led to emergency situations with an enormous impact on Europe.
In 2011 the Civil War in Syria has started. This had a great impact on neighboring countries such as Jordan, Lebanon, and Turkey. In a study from the southeastern Turkish city of Kahramanmaraş, a more than six-fold increase of cutaneous leishmaniasis had been observed between 2011 and 2013.4 Studies from Jordan where a large population of refugees from Syrian Civil War found shelter suggest that there is a significant percentage of patients with non-communicable diseases, in particular chronic diseases like cardiovascular, diabetes or chronic respiratory [4].
In our specific situation in Dresden, the establishment of an emergency refugee camp in from 23 July to 9 October 2015, with up to 1,100 inhabitants has challenged the organization and structures of the neighboring hospital due to a lack of other official structures of health care. Volunteers cannot replace official and stable infrastructure of health service [5].
More than 65% of dermatological cases were due to communicable infectious (bacterial, viral and mycotic) diseases and scabies. Surprisingly, we did not observe cutaneous leishmaniasis amongst those asylum seekers, although a major part came from Syria. Syria is one of the hotspots for cutaneous leishmaniasis among the Mediterranean countries with Leishmania major and Leishmania tropica as the main aetiological agents [6]. Other hotspots are Afghanistan and Pakistan with a rising prevalence [7]. Although we found no case of cutaneous leishmaniasis in the temporary refugee camp, the disease will not stop at the borders and we must be aware of this disease [8].
The high prevalence of scabies and infectious disorders argues for a screening when displaced people enter a refugee camp. This was not established in the first weeks after opening of the camp. By this important tool, however, spread of communicable diseases can be prevented.
In case of endemic scabies ivermectin is an alternative to permethrin [9]. In Germany, ivermectin is off-label for scabies. Therefore the treatment was realized by topical permethrin for index patients and family members.
Health service, however, can only be successful when the communication with asylum seekers and health care professionals can be ensured. This is not restricted to the service of interpreters but other issues like overcome of cultural barriers [10].
This is the first empirical study of dermatologic health care needs in refugees/asylum seekers in Germany. Our study is limited by the fact of a temporary tent camp, what will not reflect the situation after prolonged stay of people, and the single center experience. Nevertheless, the data argue for the importance of dermatologic care and treatment in displaced people [11,12].
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. United Nations High Commissioner for Refugees: UNHCR global trends report 2013 [http://www.unhcr.org/statistics.]
2. Schneider C, Mohsenpour A, Joos S, Bozorgmehr K, Health status of and health-care provision to asylum seekers in Germany: protocol for a systematic review and evidence mapping of empirical studiesSystem Rev 2014; 3: 139.
3. Inci R, Ozturk P, Mulayim MK, Ozyurt K, Alatas ET, Inci MF, Effect of the Syrian Civil War on prevalence of cutaneous leishmaniasis in southeastern Anatolia, TurkeyMed Sci Monit 2015; 21: 2100-4.
4. Doocy S, Lyles E, Roberton T, Akhu-Zaheya L, Oweis A, Burnham G, Prevalence and care-seeking for chronic diseases among Syrian refugees in JordanBMC Public Health 2015; 15: 1097.
5. Pich H, Erstaufnahmeeinrichtung: Drinnen und draußenÄrztebl Sachsen 2015; 26: 369-72.
6. Haddad N, Saliba H, Altawil A, Villinsky J, Al-Nahhas S, Cutaneous leishmaniasis in the central provinces of Hama and Edlib in Syria: Vector identification and parasite typingParasit Vectors 2015; 8: 524.
7. Afghan AK, Kassi M, Kasi PM, Ayub A, Kakar N, Marri SM, Clinical manifestations and distribution of cutaneous leishmaniasis in PakistanJ Trop Med 2011; 2011: 359145.
8. Wollina U, Koch A, Schönlebe J, Tchernev G, Chokoeva AA, Lotti T, Non-healing facial lesions: cutaneous old world leishmaniasis in DresdenJ Biol Regul Homeost Agents 2015; 29: Suppl 199-102.
9. Wollina U, ScabiesÄrztebl Sachsen 2015; 26: 373-6.
10. Jonzon R, Lindkvist P, Johansson E, A state of limbo–in transition between two contexts: Health assessments upon arrival in Sweden as perceived by former Eritrean asylum seekersScand J Public Health 2015; 43: 548-58.
11. Ryan TJ, The International Society of Dermatology’s Task Force for Skin Care for All: Community DermatologyInt J Dermatol 2011; 50: 548-51.
12. Fuller LC, Hay R, Morrone A, Naafs B, Ryan TJ, Sethi A, Guidelines on the role of skin care in the management of mobile populationsInt J Dermatol 2013; 52: 200-8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.
Comments are closed.