Pilomatricoma of the orbit
Rafael Corredor-Osorio1, Moravia Suarez-Tata1, María Eugenia Orellana2
1EL Viñedo OphthalmologicClinic, Valencia, Carabobo State, Venezuela, 2Ocular Pathology Section, Pathology Institute “Dr Jose A O’Daly”, Universidad Central de Venezuela, Caracas, Venezuela
ABSTRACT
Pilomatricoma is an uncommon, benign skin neoplasm, originating from the matrix of the hair root. These lesions are typically found in the head and neck region, but also occur in the upper extremities and are rarely report in the other sites. It is most commonly seen in children and adolescents with female predominance, but extremely rare in middle age on eyelid or eyebrow. We report a 41-year old male, who developed a single, subcutaneous tumor that gradually and progressively grew over one year period. On physical examination, there was a, firm, painless, non- ulcerated, nodule in the right orbit. Upon computed tomography (CT) scan, well- circumscribed enhancing nodulewas found. The presumed diagnosis of dermoid, epidermoid cyst was made. An excisional biopsy performed for definite diagnosis and treatment. Histopathologic examination with hematoxylin-eosin staining confirmed that mass to be pilomatricoma. Pilomatricoma of the eyelids and orbit is often misdiagnosed clinically and is extremely rare en middle age. This is a report of unusually pilomatricoma in orbit of an adult male. The patient has no symptoms or sign suggestive of recurrence at 5 years after nodule excision.
Key words:Pilomatricoma; Eyelid; Skin neoplasm
INTRODUCTION
Pilomatricoma or calcifying epithelioma of Malherbe is a relatively uncommon originating from the matrix of the hair root [1–4]. Pilomatricoma may be located in any part of the body [4–6] except the palms and soles but, has a predilection for de upper lid and eyebrow [1,3].
It is most commonly seen in children and adolescents [3]. Forty percent of them develop in the first decade of life and other 20% in the second decade [1,7] although can occur at any age. It is more common in female by radio of 3:2, but rarely seen in male adults on the eyelid and eyebrow region [1,5].
Pilomatricoma is usually not considered in differential diagnosis of firm skin nodule on eyelid and orbit. This is a report of an unusually, single, firm, nodular, non-ulcerated, painless orbital pilomatricoma located under right lower eyelid of an adult man. This entity has to be considered in the differential diagnosis of such lesions involving orbit.
CASE REPORT
A previously healthy 41-year old male had a large but asymptomatic lesion in the right orbit (Fig. 1a). He had first noted a small papule that gradually and progressively grew over 1 year period.
On physical examination, the right orbit lesion was a firm, hard, mobile, 10×10- mm nodule in subcutaneous tissue. There was no significant medical or surgical history. The remaining ocular examination was normal. Upon CT scan, there was a circumscribed nodule with peripheral enhancement located at the right eyelid (Fig. 1b).
A presumptive diagnosis of dermoid or epidermoid cyst was made. An anterior orbitotomy was performed under local anesthesia. A skin incision was undertaken in the infraciliar margin. The lesion was meticulously dissected of the surrounding tissues and its complete removal was accomplished (Fig. 1c).
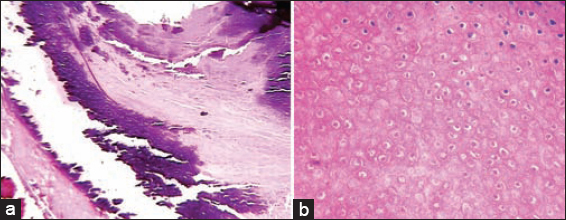
Gross pathology revealed brown-yellowish firm tissue, measuring 11×7×6 mm. Histopathology showed fibroadipose tissue with well demarcated nodule, comprised of basaloid and shadow cells with adjacent areas of intralesional calcification (Figs. 2a and 2b). The overall histological findings were suggestive of pilomatricoma. There was no evidence of recurrence at 5 years after nodule excision.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
Pilomatricoma is a benign skin tumor arising from cells of the hair follicle [1,7–9]. Its incidence is 1/800-1000 cutaneous tumors, affecting predominantly women [10]. Four clinical variants have been described: and eruptive type, a perforating type, a familial type associated with myotonic dystrophy and Gardner syndrome [11].
Clinically presents as a firm, single, stony hard slow-growing subcutaneous or intradermical nodule, asymptomatic, adherent to the skin, but not fixed to underlying tissue [1,11–13]. Lesions are usually skin color, but reddish-blue, lesions have been observed probably resulting from the hemorrhage [5].
Periocular tissues are involved in 10-17% of cases and 5% of cases are multifocal [7]. The size of the pilomatricoma varies from the 0.5 – 3.0 cm but giant periorbital lesions up top 3.0 cm have been rarely reported [5].
Most of the eyelid pilomatricoma reported so far have been in young adults and rarely in older patients [5] and female predominance ranging from 55 – 75% [13]. The appearance of multiples pilomatricoma has been occasionally associated with myotonic dystrophy (Steinert disease), Turner syndrome, Gardner syndrome, sarcoidosis [10,13–15] trisomy 9 [12].
Differential diagnosis of pilomatricoma was varied among the three age groups: pilomatricoma in children may be mistaken for epidermoid cyst, sebaceous cyst, dermoid cyst or hemangioma [8]. Differential diagnosis of adult an elderly cases was considered as fibrohistiocytic proliferation (dermatofibroma or fibroma), dermal nevus, adnexal tumor, cutaneous metastases [13] keratoacanthoma [13,14,16] and basal cell carcinoma [1,4].
Preceding trauma, surgery, infection or insect bite [4,12] intramuscular injection at the site of occurrence of tumor has been reported [9]. In general pilomatricoma is not hereditary [4,12] Etiology has been linked to mutations such as B catenin and bcl-2 [15]. It has been showed trisomy 18 as a consistent feature in pilomatricoma [17].
Histopathology examination reveals grossly well circumscribed and firm gritty nodule [7] with basaloid cell and keratinized eosinophilic shadow cells located towards the center of the tumor and occasionally foreign giant body cell reaction [7,11,13]. Calcification (70-80%), ossification (15-50%) were common features. Although can showed cellular evolution toward the other parts of the hair follicle, such as the other an inner root sheaths, sebaceous and infundibular components, therefore, can be considered a panfollicular neoplasm [18].
However, malignant transformation of pilomatricoma was rare, and tended to occur in middle-age or elderly cases [13]. The histopathological features that distinguish a pilomatrixcarcinoma from the pilomatricoma are: asymmetry of the tumor, infiltrative borders, and predominance of basaloid cells with atypical mitoses, nuclear pleomorphism, and necrotic foci, invasion of vessels and nerves and infiltration into underlying structures [11,13].
The characteristic computed tomography appearance has been described to be that of a non-contrast enhancing, sharply, well-demarcated subcutaneous nodule [15] soft-tissue mass adherent to the skin with or without visible calcifications [11]. The treatment of pilomatricoma including a complete excision biopsy with narrow margin, is usually satisfactory [4,7,9].
The present case has showed no recurrence or metastases for 5 years since the resection.
In conclusion, periocular pilomatricoma is often misdiagnosed clinically and correct diagnosis is only established after excision and histopathological examination, so, it should also be considered in the differential diagnosis of the lesion involving eyelids and orbit.
Most of pilomatricoma have a predilection for the upper lid, eyebrow and canthal area, occur more frequently in children with female predominance and rarely seen in male adults. We have described in middle-age man an extremely rare pilomatricoma of the orbit under the right lower eyelid as this case is showed.
Most case reports were documented in pediatrics, otolaryngology, dermatology literature, ophthalmologists may not be familiar with this entity, and consider it in the differential diagnosis of subcutaneous nodule in the periocular region. The present case has showed no recurrence or metastases for 5 years since resection.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles written informed consent was obtained from the patient for publication of this article and any accompanying image.
REFERENCES
1. Chapman FN, McGhee CNJ, McCarthy J, An unusual impediment to spectacle wear: pilomatrixomaBr J Ophthalmol 1995; 79: 1143-4.
2. Ferrari-Marback E, Cardoso C, Nossa Moitinho LM, Lorens Marback R, Estudio clínico-patológico do Pilomatrixoma palpebral: experiencia no hospital universitario Prof. Edgard SantosArq Bras Oftalmol 2007; 70: 501-3.
3. Mathen LC, Olver JM, Cree IA, A large rapidly growing Pilomatricoma on a lower eyelidBr J Ophthalmol 2000; 84: 1203-4.
4. Guinot-Moya R, Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C, Pilomatrixoma: review of 205 casesMed Oral Patol Oral 2011; 16: e552-5.
5. Risvi SAR, Naim M, Alam MS, A giant upper eyelid ossifying PilomatricomaIndian J Ophthalmol 2008; 56: 509-11.
6. Izquierdo-Rodríguez C, Mencia-Gutiérrez E, Gutiérrez-Díaz E, Suárez-Gauthier A, Presentación inusual en el parpado de PilomatrixomaArch Soc Esp Oftalmol 2006; 81: 483-6.
7. Ali MJ, Honavar SG, Naik MN, Vemuganti GK, Malherbe´s calcifying epitelioma (Pilomatrixoma): an uncommon periocular tumorInt J Trichology 2011; 3: 31-3.
8. Rosa N, Lanza M, Cennamo G, Accardo M, Pilomatricoma of the eyelidJ Dermatology Case Rep 2008; 2: 21-3.
9. Malpathak VD, Zawar VP, Chuh AA, Ghadi PS, Giant Pilomatricoma (Pilomatrixoma) following an intramuscular injectionJ Dermatol Case Rep 2008; 29: 11-3.
10. Solivetti FM, Elia F, Drusco A, Panetta C, Amantea A, Di Carlo A, Epithelioma of Malherbe: new ultrasound patternsExp Clin Cancer Res 2010; 29: 42.
11. AbdEL-Gawad MM, Zaghloul AB, Yousef AA, Giant peduncular Pilomatricoma (calcifying Epithelioma of Malherbe). An interesting caseGulf J Dermatol Venereol 2011; 18: 50-2.
12. Passi N, Chawla U, Jyoti Khurana AK, Pilomatrixoma of the eyelid in a middle agedNepal J Ophthalmol 2011; 3: 88-90.
13. Ching-Ju H, Ji-Haw Y, Su-Fen W, Pilomatricoma of the eyelid and eyebrow in an adult maleTaipei City Med J 2007; 4: 196-203.
14. Castelo-Soccio L, Katowitz WR, Katowitz JA, Shah KN, Treat JR, Yan AC, Picture of the month. Eyelid pilomatricomaArch Pediatr Adolesc Med 2009; 163: 955-6.
15. Li Chan JJ, Liang Tey H, Multiple pilomatricomas: case presentation and review of the literatureDermatol Online J 2010; 16: 2.
16. Kang HY, Kang WH, Perforating pilomatricoma resembling keratoacanthomaEur J Dermatol 2000; 10: 63-4.
17. Agoston AT, Liang CW, Richkind KE, Fletcher JA, Vargas SO, Trisomy 18 is a consistent cytogenetic feature in pilomatricomaMod Pathol 2010; 23: 1147-50.
18. Simi CM, Rajalakshmi T, Correa M, Pilomatricoma: a tumor with hidden depthsIndian J Dermatol Venenereol Leprol 2010; 76: 543-6.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.