Primary cutaneous follicle center lymphoma: A case report
Ayşe Akbaş1, Fadime K?l?nç1, Sertaç Şener1, Nuran Süngü2, Aydan K?l?nçaslan2, Ahmet Metin1
1Department of Dermatology, School of Medicine, Y?ld?r?m Beyaz?t University, Ministry of Health Atatürk Training and Research Hospital, Ankara, Turkey, 2Department of Pathology, School of Medicine, Y?ld?r?m Beyaz?t University, Ministry of Health Atatürk Training and Research Hospital, Ankara, Turkey
ABSTRACT
Primary cutaneous B-cell lymphomas are defined as malignantB-cell proliferations presenting with cutaneous involvement alone and no evidence of extracutaneous manifestationswhen complete staging has been performed. Primary cutaneous folicul centre cell lymphoma (PCFCCL) is a relatively rare entity. Here, we report a 66-year-old female patient presented with six mounts history of erythematous papules and nodules over the skin of neck and body PCFCCL was diagnosed by skin biopsies. No evidence of systemic involvement was present at the time of diagnosis. She was not taken terapy but ones six mounts was done control and she hasn’t got new lesions. Twelve months later she remains asymptomatic.
Key words:Primary cutaneous lymphoma; follicular centre cell lymphoma; cutaneous B cell lymphoma
INTRODUCTION
Primary cutaneous lymphomas show characteristic clinical and histopathological features and their biological behaviour is different from nodal lymphomas [1]. The majority of the lymphomas at different stages of development and which have not spread outside the skin are B-cell lymphomas. This type is more rarely observed than the primary T-cell lymphomas of the skin and comprise 20-25% of primary skin lymphomas. They are mostly low grade, progress slowly and have a good prognosis. The view that the lesions should stay limited to the skin for at least 6 months has lost its importance in recent years [2]. According to the classification by WHO-EORTC (World Health Organisation – European Organization for Research and Treatment of Cancer – Cutaneous Lymphoma Project Group), B-cell lymphomas of the skin can be classified into three main groups [3]:
- Primary cutaneous marginal zone lymphoma
- Primary cutaneous large B-cell lymphoma
- Primary cutaneous follicle centre cell lymphoma.
In this case report, a middle aged female patient with multiple, indurated, erythematous papules and nodules in the neck and back area and histopathologically diagnosed with primary cutaneous follicle centre cell lymphoma of the skin (PFMHL) is presented and the disease is discussed in the light of the current information.
CASE REPORT
A sixty year old patient presented to our clinic with a red rash in her neck and back which were present for six months. During the dermatologic examination, numerous erythematous and indurated red and purple papules and nodules were observed in her neck and back (Fig. 1). No lymphadenopathy or hepatosplenomegaly was observed during her systemic examination. Skin biopsies were taken from the lesions with the pre-diagnoses of cutaneous B-cell lymphoma, sarcoidosis, multiple myeloma, lymphomatoid papulosis, pseudolymphoma, cutaneous plasmacytoma, and mastocytosis.
Histopathologically, nodular lymphoid aggregates with large hyperchromatic nuclei and irregular contours, some with visible nucleoli and narrow cytoplasm, resulting from small to medium diameter, atypical neoplastic lymphoid cell proliferation and mixed with centrocytes and centroblasts were observed in the perivascular areas within the dermis (Fig. 2). Around these lymphoid aggregates, mantle zones were observed and tingible body macrophage loss was detected within the follicles.
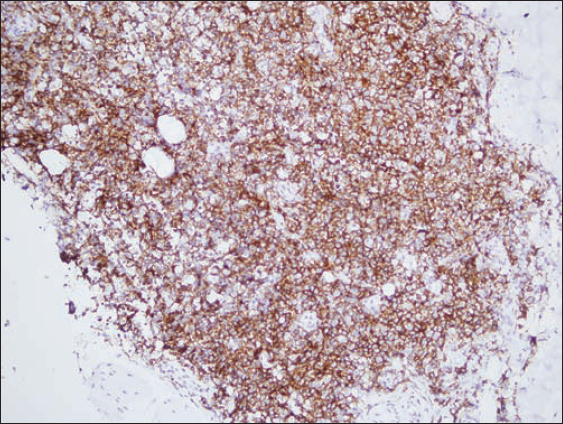
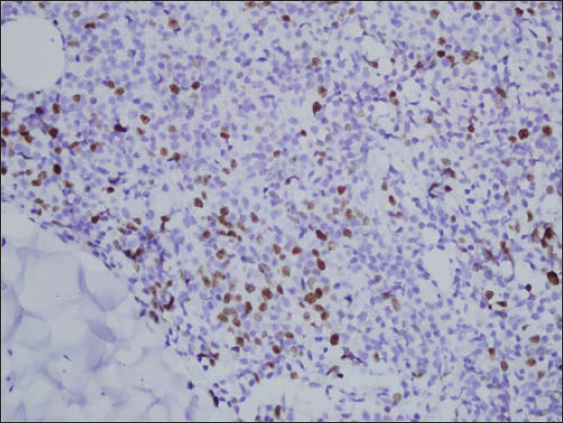
The immunohistochemical examinations revealed diffuse and strong staining with CD 20 (Fig. 3), CD79a, Bcl-2 and Bcl-6, and positive staining with CD23 in the focal areas. No immune reaction was observed with CD 10, Tdt and cyclin-D1. In a small number of mature lymphocytes, positive (+) staining was observed with CD3, CD4, CD8 and CD5. Only a few immunoblastic cells were stained using CD 30. The Ki-67 proliferation index was around 20-30% at its highest level (Fig. 4). Based on the morphological and immunohistochemical findings at hand, the patient was diagnosed with atypical cell proliferation and mainly with “follicular centre cell lymphoma”.
The patient was referred to the haematology clinic to investigate any systemic involvement. The tests revealed no pathological laboratory findings. The patient’s thoracic X-ray was normal. The peripheral smear and bone marrow aspiration and biopsy were evaluated as normocellular. The cervical and pelvic tomographies were observed to be normal. The biopsy of the lesion detected during the abdominal tomography, which was first thought to be a metastasis, pointed out a hemangioma. Since the scans did not reveal any foci, the haematology clinic did not start any treatment protocol and recommended follow up visits every 6 months. No systemic involvement was observed during the follow up. In the last visit, the patient stated that some of the lesions had disappeared, only to be replaced by new ones.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
PFMHL is the most frequently observed type of cutaneous B-cell lymphomas comprising approximately 40% of all the cases [1]. It features neoplastic B-cells morphologically and immunophenotypically resembling follicle centre cells and including the centrocytes and centroblasts in the skin. It is mainly located on the head and at the torso, and shows a slow progress. It usually grows diffusely and with few follicular growth patterns. Lesions located at the back are defined as “Crosti lymphoma” or “reticulohistiocytoma of the back” [2–5]. The dermatological examination reveals individual or grouped, red to brown coloured papules, plaques and tumours, while ring-shaped erythema may also be observed around certain lesions. Ulcerations are not commonly observed and the lesions are usually asymptomatic. They are frequently located on the hairy skin, forehead, neck and torso, while the lower extremities are rarely involved [6]. Multifocal lesions are not an indication of a bad prognosis. The clinical development of the disease shows a slow progress though the lesions may spread wider if left untreated. The disease rarely spreads to the other tissues than the skin. It is usually observed in the 5th and 6th decades of life [2], although cases observed in younger patients have also been reported [7]. The thoracic, abdominal and pelvic CT scans and the bone marrow biopsy performed for the purpose of staging is negative during the diagnosis [2].
The histopathological examination reveals diffuse or nodular infiltration in the reticular dermis and subcutaneous tissue. The epidermis is unaffected and there is no epidermotropism. A clear grenz zone is visible in the papillary dermis [2,4–6]. As the tumoral lesions progress, the diameter and number of the neoplastic B-cells increases, while the number of the reactive T-cells decreases. A mix of centrocytes, centroblasts and reactive T-cells is observed in early and small lesions. In large and rapidly growing tumours, monomorphic follicle centre cells, large centroblasts, multilobulated cells and rarely spindle cells are observed. During the immunophenotypic examination, 60-70% of the cases are positive in terms of monoclonal rearrangement. B-cell phenotypes CD19, CD20, CD22 and 79a are positive. While Bcl- 6 is positive, CD- 10 is frequently (+) and CD5 is (-). The negative Bcl-2 protein and no t(14: 18) translocation are the differentiating factors from systemic nodal follicular lymphomas during the diagnosis. The prognosis is disputable in the patients where more than 50% of the neoplastic B-cells produce Bcl- 2. Staining through the active markers of B-cells such as MUM- 1/IRF4 and FOXP1 is negative in most of the cases [2,5]. The t (14: 18) translocation is characteristic in the cytogenic examination of systemic follicular lymphomas [6]. While the t(14: 18) and Bcl- 2 expressions are negative in the majority of the follicle centre cell lymphomas, inactivation of the P15 and P16 tumour suppressor genes is rare. Pseudolymphomas are important in the differential diagnosis [2].
There are varying approaches to the treatment and different protocols are proposed. These include radiotherapy in the early stage; chlorambucil multiple chemotherapy (CHOP), and intralesional anti-CD20 monoclonal antibodies for middle stage; and interferon, IL- 2, systemic steroids in the advanced stage and in case of multiple lesions; and the excision of solitary lesions [1]. Radiotherapy may be added in case of repeating solitary lesions [5,6,8–10]. The prognosis is very good regardless of the growth patterns and the number of the blast cells and the 5-year survival rates are over 95% [3]. The lesions tend to recur in 30% of the cases, although it is not a sign of a poor prognosis [2].
We did not observe any systemic involvement in our patient during the diagnosis and the follow up.
The case of a primary follicle-centre cell lymphoma has been presented due to its rarity.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Ferahbaş A, Ulaş Y, Utaş S, Eser B, Primary Cutaneous Lymphomas: A Retrospective Evaluation Erciyes T?p DergisiErciyes Med J 2006; 28: 77-81.
2. Engin B, Kutlubay Z, Uzunçakmak TK, Tüzün Y, Primary cutaneous B cell lymphomas Dermatoz2012; 3: 29-32.
3. Çankaya H, Bozkuº F, A?ar Y, Yuca K, Çalka Ö, Diffuse large B-cell lymphoma case following wide ulceration on neck skin, T?p Araºt?rmalar?Dergisi2008; 6: 3181-185.
4. O?uz O, Tüzün Y, Gürer MA, Serdaro?lu S, O?uz O, Aksungur V, Derinin Lenfoproliferatif Hastal?klar?. Dermatoloji 2008; 3. Bas. ?stanbul: Nobel; 1963-1994.
5. Cerroni L, Kerl H, Bolognia JN, Jorizzo JL, Rapini RP, B- cell Lymphomas of The Skin. Dermatology’de 2003; Spain: Mosby; 1907-1920.
6. James WD, Elston DK, Berger RG, Cutaneous Lymphoid Hyperplasia, Cutaneous T-cell Lymphoma, Other Malignant Lymphomas and Allied Diseases Andrrews Disease of Skin 2011; c-32: 11th ed. Chine: Elsevier Saunders Company; 720-40.
7. Ar?can Ö, Önver N, Özpuyan F, Primary Cutaneous Follicle Center Lymphoma: Case ReportTurkiye Klin J Dermatol 2010; 20: 40-5.
8. Gulia A, Saggini A, Wiesner T, Fink-Puches R, Argenyi Z, Ferrara G, Clinicopathologic features of early lesions of primary cutaneous follicle center lymphoma, diffuse type: implications for early diagnosis and treatmentJ Am Acad Dermatol 2011; 65: 991.
9. Sokol L, Naghashpour M, Glass LF, Disclosures Primary Cutaneous B-Cell LymphomasRecent Advances in Diagnosis and Managemen Cancer Control2012; 19: 236-44.
10. Kalkan G, Takc? Z, Celile Gülfer Akbay G, Güngör E, Üner A, Ekºio?lu M, Primary cutaneous follicle center lymphoma in a 77-year-old womanJ Clin Exp Invest 2013; 4: 521-4.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.


Comments are closed.