Chilhood leprosy: Clinical and epidemiological study in the Department of Dermatology, Clinicas Hospital, Faculty of Medical Sciences, National University of Asuncion-Paraguay, 2005-2014
Beatriz Di Martino Ortiz, María Laura Sánchez, Celeste Valiente, Gabriela Martínez, Mirtha Rodriguez Masi, Oilda Knopfelmacher, Lourdes Bolla de Lezcano
Department of Dermatology, Clinicas Hospital, Faculty of Medical Sciences, National University of Asuncion, Paraguay
DOI: 10.7241/ourd.20161.4
ABSTRACT
Introduction: Leprosy in childhood is not a common finding. The risk of a child to develop the disease is 4 times greater in contact with close people and 9 times higher among household contacts. The maximum risk observed is when the contact is Multibacillary (MB) and intradomicilliary. Leprosy in childhood reflects the clinical characteristics of adult, with some peculiar aspects. Non-contagious forms (IL and TT) are common during childhood. The contagious forms (BB, LB and LL) are less frequent due to higher required incubation period.
Aim: To describe the clinical and epidemiological characteristics of childhood leprosy in the Department of Dermatology, Clinicas Hospital from January 2005 to July 2014.
Methods: Retrospective, observational cross-sectional study with an analytical component.
Results: The total number of leprosy patients was 369, and of these 11 were pediatric patients (2.98%) with a predominance of males (8/11) from 3 to 16 years. The BI ranged from negative to 3+. 6/11 were MB. The evolution was good in all cases and two patients developed leprorreactions. The lesions were predominant in facial location. 6/11 patients had family contacts.
Conclusions: Leprosy in children is more common than is reported, especially in endemic areas. In <5 years, the disease is very rare. More than half of the cases of children with leprosy have a positive contact. It is considered that in <5 years the spread is always intradomiciliary; this shows the importance of monitoring contacts, which will be possible with the determination of all stakeholders in order to banish the undetected cases and prevent damage.
Key words: Hansen disease; Leprosy; Childhood hansen disease
INTRODUCTION
Hansen’s disease is a contagious disease of chronic course caused by Mycobacterium leprae that has tropism for the skin, mucous membranes and peripheral nerves. Other organs may also be compromised.
Because the consequences, degree of disability and deformity that occurs, are indispensable early diagnosis and treatment, allowing an endemic disease control.
In the field of pediatric dermatology leprosy remains a little described and undervalued in daily practice, so it becomes a diagnostic challenge because of the diversity of clinical manifestations that may occur, making necessary a thorough skin and neural examination in all children presenting suspicious lesions suggestive and an infectious source [1].
Aims
General
To describe the clinical and epidemiological characteristics of childhood leprosy in the Department of Dermatology, Clinicas Hospital, in the period from January 2005 to July 2014.
Specific
- To set the epidemiological characteristics of the study population.
- To determine the clinical characteristics of leprosy in childhood.
- To describe the type of treatment given and evolution.
MATERIALS AND METHODS
Design
Retrospective, observational cross-sectional study with an analytical component. The study was conducted at the Department of Dermatology of CH, FMS-NUA, between January 2005 and July 2014.
Reference Population
Asunción is the capital of the Republic of Paraguay and is located on the right bank of the Paraguay River (which divides the country into two regions) standing in the Eastern Region. Its metropolitan area called Gran Asunción has a population of 2,870,000 inhabitants. Its area is 118 km2 and population density 4,411 inhabitants/km2.
Inclusion Criteria
All patients with leprosy in childhood, diagnosed clinically and with pathological confirmation, that have consulted in the Department of Dermatology of CH. FMS-NUA.
Exclusion Criteria
No leprosy patients in pediatric age or no pathological confirmation of the disease.
Sources
Medical records of patients with diagnosis of Hansen’s disease in childhood.
RESULTS
- The total number of leprosy patients was 369, and of these 11 were in pediatric age (2.98%).
- The disease predominated in males.
- The age of onset was from 3 years to 16 years.
- Bacillary Index (IB) ranged from negative to 3+.
- Six of the eleven cases presented Multi bacillary forms; the TT and LL forms were 4 cases each.
- The evolution was good in all cases and two developed leproreactions.
- The predominant location of the lesions was on the face.
- Six of the eleven cases had a family contact.
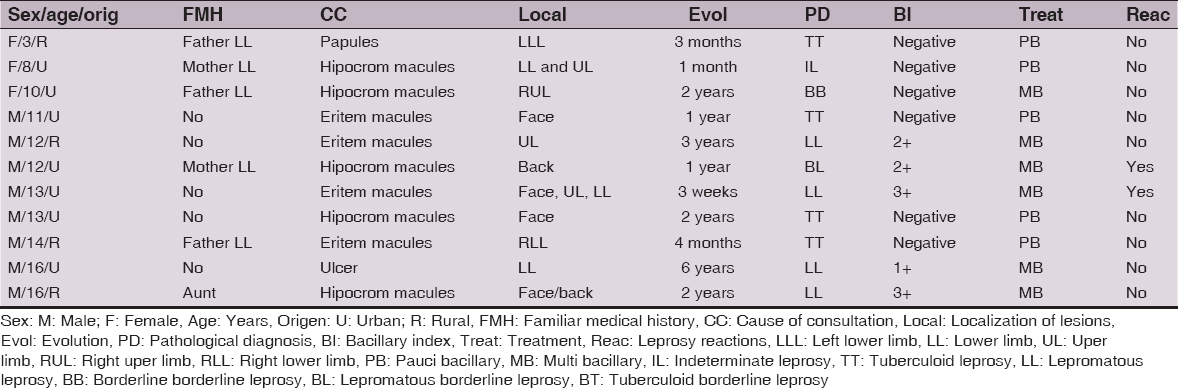
The summary of findings stated in Table 1.
DISCUSSION
Pediatric patients suffering from leprosy were 11, which corresponds to 2.98% of the total infected patients (369), lower than in other series, as Terencio de las Aguas (7.7%) and Fakhouri et al (17.3%) [1–5].
Among the children affected, males predominated coinciding with a national study of another service of dermatology; other authors did not find any differences in sex [4,5].
Ages of children affected ranged from 3-16 years, with school children (6-12 years) and adolescents the hardest hit, coinciding with the literature reviewed [1].
The BI ranged from negative to 3+, with 5 positive cases (45%), is inconsistent with the literature in which the positivity percentage is lower (2%). This is because the predominant number of MB cases in our study (6/11), opposite as usually PB cases described more frecquent in children [5,6].
Evolution was good in all cases and two developed leproreactions.
The elementary dermatological more frecquent lesion was a macule, with facial location, and in exposed areas, which is the most frequent site of occurrence in children with leprosy in other countries [7].
Six of eleven cases had a family contact. In most series this is the constant [1,3,8].
In developing countries, where leprosy is a public health problem, it is well accepted that children below five years are more likely to develop it than adults. About 17.13% of all cases of leprosy in India are in children under 15 years. Van Beers et al. show that the risk of a child developing leprosy is 4 times greater in contact with close people and 9 times higher among household contacts. The maximum risk is observed when the contact is Multibacillary and intradomicilliary [3].
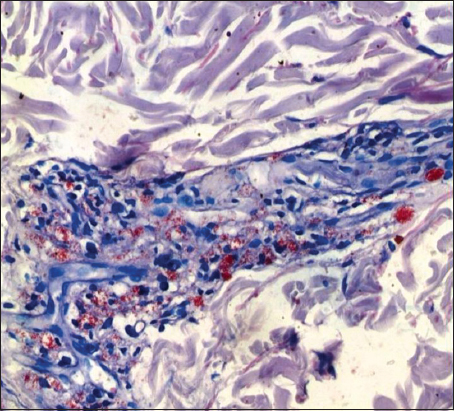
Leprosy in childhood presents with a variety of clinical and histological manifestations, which necessitate a thorough skin examination in every child with suggestive or suspicious skin lesions and an infectious source (Figs 1ab and 2). Many skin lesions are usually asymptomatic and often mimic other dermatologic pictures [1,3].
CONCLUSIONS
- Leprosy in children is more common than we tend to think, especially in endemic areas, as is our country [9]. In patients with less than five years, the disease is very rare [10].
- More than half of the cases of children with leprosy have a positive contact.
- It is consider that in patients with less than five years the spread is always intradomiciliary; this shows the importance of monitoring contacts, which will be possible with the determination of all stakeholders in order to banish the undetected cases and prevent damage.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Táquez A, Cerón C, Chaparro M, Sales A, Nery J, Miranda A, Lupi O, Lepra en la infancia. Desafío diagnósticoRev Argent Dermatol 2011; 92: 2-10.
2. Fakhouri R, Soto M, Manini M, Margarido L, Nodular leprosy of childhood and tuberculoid leprosy: a comparative, morphologic, immunopathologic and quantitative study of skin tissue reactionInt J Lepr Other Mycobact Dis 2003; 71: 218-26.
3. Di Martino Ortiz B, Rodriguez Masi M, Knopfelmacher O, Bolla de Lezcano L, Lepra infantil. Presentación de un caso. Childhoodleprosy. Report of a caseDermatol Online J 2011; 17: 13.
4. Terencio de las Aguas J, Situación de la lepra en el mundoMed Cután Iber Lat Am 2005; 33: 191-2.
5. Mata Jiménez O, Aguilar Aguilar N, Miranda A, Freitas de Souza M, Azulay R, da Costa Nery J, Lepra en la infancia: caracterización de parámetros clínicos en los estados reaccionalesMed Cutan Iber Lat Am 2006; 34: 263-9.
6. Dias Gomes C, Andrade Pontes M, SáGonçalves H, Oliveira G, PennaAn Bras Dermatol 2005; 80: 283-8.
7. Rodríguez E, Díaz O, Hernández E, Boletín Epidemiológico Semanal2013; 21: 1-13.
8. Martinez Braga G, Guglielmone C, Di Martino Ortiz B, Bolla de Lezcano L, Aldama A, Mendoza G, Lepra infantil: estudio clínico y epidemiológico en dos servicios de dermatología del Paraguay. Periodo 2005-2011Fontilles, RevLeprol 2012; 28: 293-301.
9. Rongioletti F, Gallo R, Cozzani E, Parodi A, Leprosy: a diagnostic trap for dermatopathologists in non endemic areaAm J Dermopathol 2009; 31: 607-10.
10. Dias Gomes CC, de Andrade Pontes MA, de Sá Gonçalves H, Oliveira Penna G, Clinical and epidemiological profile of patients diagnosed with leprosy in a reference center in the northeast of BrazilAn Bras Dermatol 2005; 80: supl 3S283-8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.