A case of purpura annularis telangiectodes of Majocchi
Havva Ozge Keseroglu1, Müzeyyen Gönül1, Hasan Benar1, Unsal Han2
1Department of Dermatology, Dişkapi Yildirim Beyazit Education and Research Hospital, 06510, Ankara, Turkey, 2Department of Pathology, Dişkapi Yildirim Beyazit Education and Research Hospital, 06510, Ankara, Turkey
Sir,
Pigmented purpuric dermatoses (PPD) are a group of disorders which have histopathologically similar but morphologically different appearance. The five main clinical subtypes of PPD has been described. The perivascular lymphocytic infiltration of superficial dermal vessels with extravasations of red blood cells are common histopathological characteristics for all types of PPD. The etiopathogenesis of disease remains obscure yet [1,2]. We report a case of purpura annularis telangiectodes of Majocchi (PATM), a very rare type of PPD, with possible drug etiology of diclofenac sodium.
A 52-years-old man presented with asymptomatic skin eruption that had been present for two months. The patient had a history of oral diclofenac sodium intake ten days before the lesions appeared. He also had hepatitis B infection recognized at childhood and he had been followed by gastroenterology department with regular interval. The physical examination revealed several, symmetrical, nonpalpable, nonblanchable, erythematous, annular purpuric patches with a peripheral rim of dark red telangiectatic puncta distributed symmetrically on the upper legs and inguinal areas. The annular patches showed central clearing with minimal hyperpigmentation and atrophy (Fig. 1).
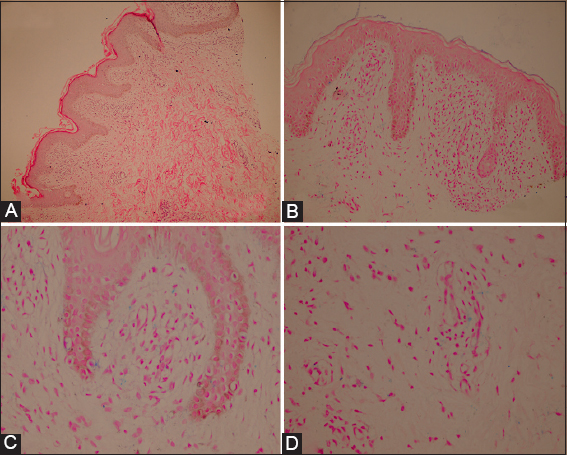
The laboratory investigations were within normal limits except hepatitis B antigen positivity. The histopathological examination revealed a moderately bandlike infiltration accompanying a prominent perivascular lymphocytic infiltration in superficial dermis. There was no evidence of vasculitis (Figs. 2A and 2B). Also, hemosiderin deposits was demonsrated within papillary dermis and macrophages by using prussian blue staining (Figs. 2C and 2D). These findings suggested a diagnosis of pigmented purpuric dermatosis. Together with clinical and histopathological appearance, diagnosis of purpura annularis telangiectodes of Majocchi was made. The drug was discontinued and topical corticosteroid was started as a treatment. Partial healing was obtained after 2 weeks of therapy.
PATM is an uncommon clinical variant of pigmented purpuric dermatosis [2]. A variety of diseases had been suggested to be associated with PPD, including Hepatitis B and C infection [3]. We consider that the skin eruption of our patient might not occur as a result of Hepatitis B virus, because he was positive for hepatitis B antigen since childhood but the lesions appeared first time two month before, after taking diclofenac sodium tablets.
A wide variety of medications including NSAIDs, diuretics, sedatives, stimulants antibiotics, cardiovascular drugs, vitamins, antihyperglycemics, isotretinoin have been implicated as drugs responsible for the development of PPD [4,5]. It was suggested that as a result of antigen-antibody complex deposition in which drugs act as a hapten, an immune system-mediated vascular damage occur and this results in capillary leakage and erythrocyte extravasation [5]. The skin eruption of our patient appeared at 10th day of oral diclofenac sodium treatment. So, we thought it might be the possible cause of skin eruption in our patient. Also, as in our case, the drug induced cases are more likely to resolve after discontinuation of drug in contrast to chronic or relapsing nature of idiopathic ones [5]. Due to possible risk of provocation of a systemic reaction [4] we couldn’t confirm the diagnoses by oral challenge test or patch test.
We intended to present this case because of the rarity of the PATM and it should be kept in mind that diclofenac sodium could play role in etiopathogenesis.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Sardana K, Sarkar R, Sehgal VN, Pigmented purpuric dermatoses: an overviewInt J Dermatol 2004; 43: 482-8.
2. Hoesly FJ, Huerter CJ, Shehan JM, Purpura annularis telangiectodes of Majocchi: case report and review of the literatureInt J Dermatol 2009; 48: 1129-33.
3. Dessoukey MW, Abdel-Dayem H, Omar MF, Al-Suweidi NE, Pigmented purpuric dermatosis and hepatitis profile: a report on 10 patientsInt J Dermatol 2005; 44: 486-8.
4. Díaz-Jara M, Tornero P, Barrio MD, Vicente ME, Fuentes V, Barranco R, Pigmented purpuric dermatosis due to pseudoephedrineContact Dermatitis 2002; 46: 300-1.
5. Kaplan R, Meehan SA, Leger M, A case of isotretinoin-induced purpura annularis telangiectodes of Majocchi and review of substance-induced pigmented purpuric dermatosisJAMA Dermatol 2014; 150: 182-4.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.