The impact of psoriasis on the lifequality: a cohort of 140 Moroccan patients
Awatef Kelati1, Mariame Meziane1, Mounir Jaafari2, Fatima Zahra Mernissi1
1Department of Dermatology, Hospital Hassan II of Fez, Fez, Morocco, 2Department of Psychiatry, Hospital Hassan II of Fez, Fez, Morocco
ABSTRACT
Introduction: The alteration of the life quality in psoriasis is currently proved.
Aim: To evaluate the particularity of this impact in Moroccan psoriatic population.
Methods: It was a prospective cohort of 140 psoriatic patients who filled the 16-Skindex questionnary to evaluate this alteration of the life quality.
Results: The life quality was significantly affected in patients having severe or old psoriasis and in young females, also it was related to the low Socioeconomic level and the living in rural areas, to the presence of psoriatic arthritis, to the scalp, the nails and mucosal involvement and to the use of systemic treatments. However, the emotional life, theimpact on daily activities and the sleep quality were not affected in our population.
Conclusions: we had a low negative impact on the sleep quality and the emotional life which may be explained by the role of the family support in our society.
Key words: Psoriasis; quality of life; Prospective cohort study
INTRODUCTION
The Psoriasis is an inflammatory, systemic and multifactorial skin disease affecting about 2% of the Moroccan population [1]. It is considered as an autoimmune disease with abnormality of mitosis and differentiation of keratinocytes where the cyclic nucleotide and lipid mediators play a key role [2,3].
This systemic disease is also known linked to a great number of comorbidities especially metabolic [4] and psychiatric [5] ones.
The alteration of the life quality of psoriatic patients has been shown in many epidemiological studies in adults and in children [6–14]. So the aim of our study was to evaluate this psycho-social impact of psoriasis in Moroccan psoriatic patients.
MATERIALS AND METHODS
It was a descriptive, analytical, unicentric and prospective study of 140 psoriatic patients treated in the Department of Dermatology ofthe Hospital Hassan II of Fez, during a period of 1 year: 2013/2014. Epidemiological andclinical data were collected in the psoriasis consultation by our doctors of the Department of Dermatology.
Psoriasis severity was calculated based on the Psoriasis Area Severity Index (PASI): Mild psoriasis: PASI <7, Moderate psoriasis: PASI between 8 and 12 and Severe psoriasis: PASI> 12.
we used the 16-Skindex as a questionnary for the evaluation of the impact of psoriasis on the life quality of psoriatic patients which include several items: pruritus, psychological impact: “No improving and recidivism, fear of worsening or persisting lesions or scars, frustration, shame, depression and anger “, relationships with others and the integrity in society, Emotional life, impact on daily activities and hobbies.
We estimated that a low impact on the life quality is a score of Skindex<10, a moderate impact on the life quality if the Skindexis between 10 and 50, and a significant impact on the life quality if the Skindex> 50.
Data analysis was performed using the SPSS 20 software, 2 kinds of analysis were carried out: Descriptive and univariate analysis.
In the univariate analysis: we analyzed the epidemiological and clinical data significantly related to each item of the Skindex.
RESULTS
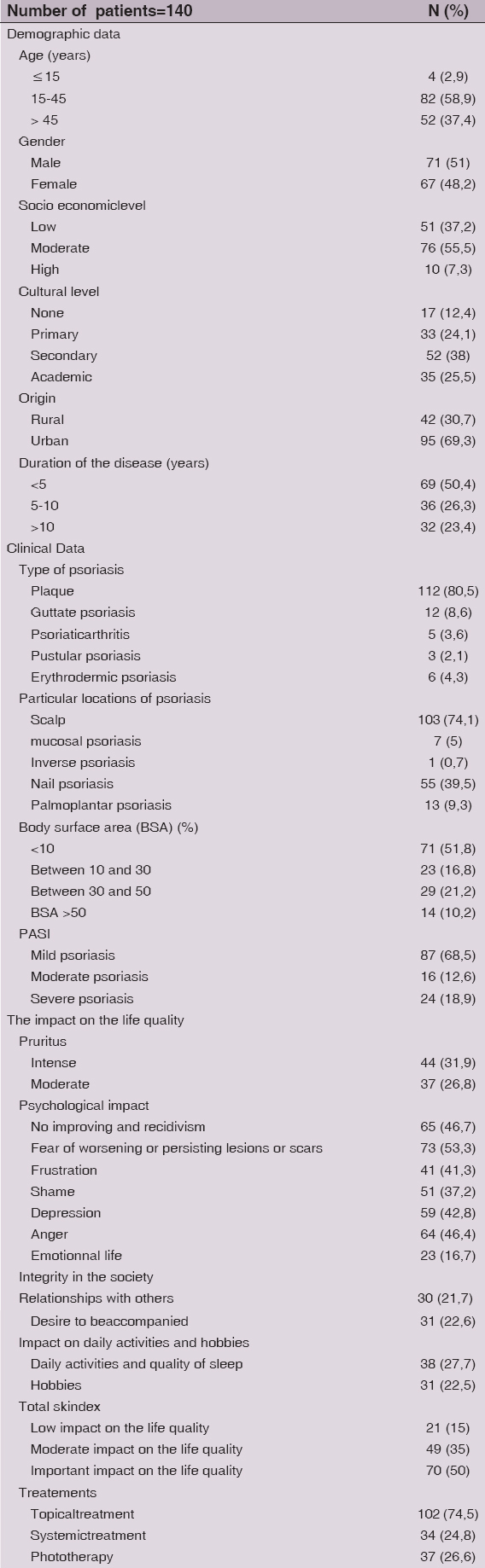
We collected 140 patients with psoriasis for this study, the mean age was 30.5 years.
58.9 % of our patients were young (between 15 years and 45 years old) and we had a slight male predominance (51 %). Our patients had a moderate socioeconomic level in 55.5 % of cases and 50,4 % of them had a recent psoriasis.
Plaque psoriasis was the most frequent form (80,5%) and we had a scalp involvement in 74.1 % of cases. 51,8% of patients had a mild psoriasis while 31.4 % had a severe one.
Besides, severe itching was present in 31,9% of our patients and 26,8% of patients had moderate pruritus.
Furthermore, 50% of our patients had an important impact on the life quality, 35 % had a moderate impact and 15 % of patients had a low impact on the life quality.
Concerning the treatments used in our patients: 74.5 % of patients used topical treatments, 24.8 % used systemic treatments (30 patients: methotrexate, 2 patients: Infliximab (Remicade) for Psoriatic arthritis, 2 patients: Retinoids), and 26.6% of patients used phototherapy UVB TL01 (Table. I).
In the Univariate Analysis
The characteristics of psoriasis significantly related to the Pruritus in our population study were: the low SEL (p= 0,05), the Mild psoriasis (p=0,011) and the living in rural areas (p=0,05) while the No improving and recidivism was significantly associated with Young age (p=0,000), Female gender (p=0,000), Psoriatic arthritis (p= 0,004) and Psoriasis of the scalp, the nails and mucosal psoriasis (p=0,000).
The Fear of worsening or persisting lesions or scars was more frequent in women (p=0,05) and the Shame was significantly related to the Young age (p=0,02) and Severe psoriasis (p=0,006). Anger was significantly related to severe psoriasis (p=0,013), old one (0,07) and the use of systemic treatments (p=0,046).
Besides, Relationships with others was altered in female patients (p=0,041), young patients (p=0,019) and patients having Severe psoriasis (p=0,056), and generally, the quality of life was significantly altered in patients having severe psoriasis (p=0,016) and old psoriasis (p=0,009).
However, the following items were not significantly affected or related to a particular characteristics of psoriasis: the frustration, the emotional life, the desire to be accompanied, the impact on daily activities, the sleep quality and Hobbies (Table. II).
DISCUSSION
Psoriasis is a complex multifactorial skin disease which is known linked to manymetabolic [15], autoimmune and psychiatric [10] comorbiditiesthat must be taken into account in the management of this disease [16].
The psychological impact of psoriasis and the alteration of the life quality iscurrently proven in many studies, There are even some series that have proven that this negative impact is stronger than other chronic dermatitis such as atopic dermatitis [17], and that this impact of psoriasis is similar to other dangerous diseases such as breast cancer and certain serious heart diseases [18]. Other studies proposed a theory that this alteration of the life quality is compounded by the other comorbidities of psoriasis. Furthermore, a recent study proved that this alteration of the quality of life affects not only psoriatic patients but also their families [19].
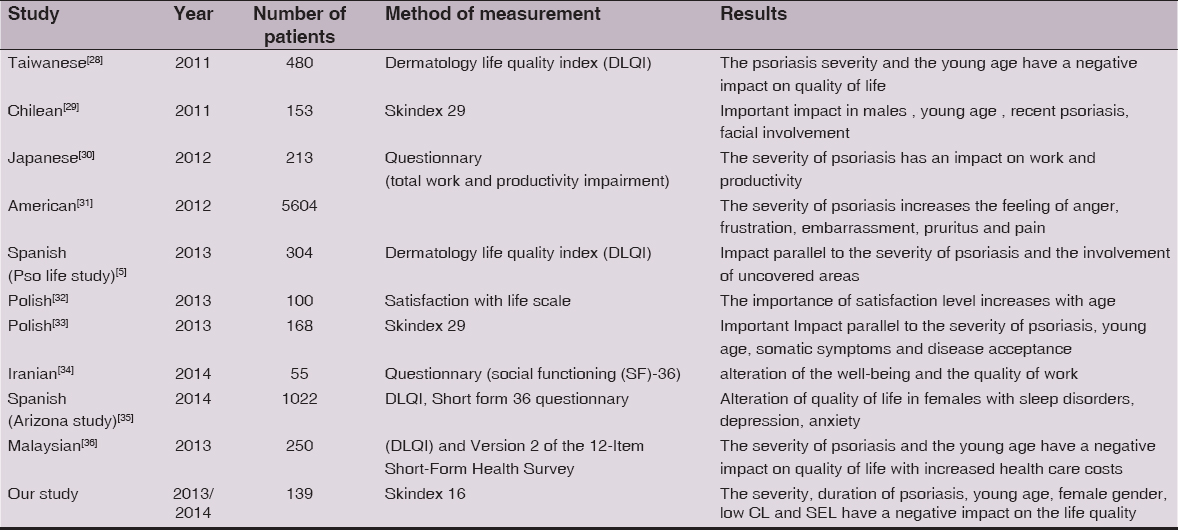
In our study, we aimed to evaluate this alteration of the life quality in Moroccan patients, we didn’t study the life quality on psoriatic patients families, or the relationship of this impact and comorbidities. So we noticed that the Severity and theduration of psoriasis are the two characteristics significantly related to the general alteration of the life quality which is almost the same for other studies (resumed in Table III).
This impact is also increased by the scalp and nailsinvolvement which affects the general health, emotional life, and increase the severity of psoriasis [20–22]. In our psoriatic patients, the scalp and nail involvement were significantly related to the fear of recurrence and persistence of lesions which may be explained by the fact that these areas of the body are the symbol of beauty especially in women.
Besides, there is currently a great interest in the psoriatic arthritis (PSA) and his negative impact on the life quality, especially if it complicates skin psoriasis, So several scales for assessing the quality of life of these patients were validated [23,24].
Furthermore, many studies proved the alteration of the life quality in patients with PSA than patients with cutaneous psoriasis only [25,26], except one study which noticed that there was no change in the impairment of the quality of life with the presence of PSA in patients with cutaneous psoriasis using the PSAQOL questionnary [27]. In our study, we had a small sample of PSA with skin psoriasis (5 patients) because these patients are also followed by Rheumatologists especially those without skin psoriasis. Despite this fact, we proved that it affected significantly the life quality of our patients especially the fear of no improving and recidivism.
Pruritus
Psoriasis is known among the most pruritic inflammatory dermatoses according to the results of several studies [37–41]. Furthermore, this pruritus increases the negative impact of psoriasis on the life quality such as sleep disorders, sexual, appetite and concentration troubles and the alteration of the quality of work [42–44].
In our study, Pruritus was present in 58,7% of our patients and was intense in 31,9%. It was significantly related to the Lower SEL, the origin from rural regions of and it increases the severity of psoriasis.
Depression
If psychiatric comorbidity is important in psoriasis, depression is by far the most common psychiatric illness encountered [45–47]. The links between psoriasis and depression are not only psychopathological, biological factors may explain this association (elevated levels of substance P and TNF, decreased serotonin levels) [48]. There is thus a vicious circle “psoriasis- alteration of the life quality- depression” which may further complicate the management of psoriasis, because the treatment of psoriasis doesn’t improve necessarily the depression. On the contrary, it is obvious that depressed psoriatic patient could not treat correctly his psoriasis [49].
A UK population-based cohort study of 146,042 patients [50] demonstrated an increased incidence of diagnoses of depression, anxiety and suicidality in psoriasis; the authors estimated that over 10400 diagnoses of depression, 7100 diagnoses of anxiety, and 350 diagnoses of suicidality were attributable to psoriasis each year, while Gupta [51] found that 5.5% of patients with psoriasis had active suicidal ideation and that 9.5% expressed a death wish and that this depression is increased by the pruritus. Another study demonstrated an increased use of antidepressant drugs in psoriasis [52].
In our study, Depression was significantly observed in patients with severe psoriasis and fortunately we had no cases of suicidality.
Sleep Quality
the sleep quality is among the domains the most affected in patients with psoriasis and this Sleep disturbances can cause significant quality of life impairment, which was proved in many studies (koo and al [53]; Delfino and al [54]; Hu and al [55]. This sleep impairment in psoriasis is known linked to many reasons such as the pruritus, the psychological burden and the obstructive sleep apnea which is a common and an increasingly prevalent sleep disorder that is receiving attention in terms of a potential association with psoriasis, psoriatic arthritis and rheumatoid arthritis [56].
In our study, this sleep quality was not significantly affected, maybe because of spiritual and religious reasons and the role of the family support in our society.
Relationships and Social Integrity
Human kind is known very sociable, but this sociability could be injured in some situations that makes the person want to be alone and distant from others. This situation could be in some chronic diseases like psoriasis. In the same time, psoriasis may attract attention and cause avoidance and public rejection which may cause a disturbance in the social integrity in psoriatic patients.
This social integrity disturbance is proven in some epidemiological studies [57,58] like the survey of Poot [59] that found severe family dysfunction in these patients in comparison with families without a psoriasis. Even in our study, we noticed an alteration of relationships with others especially in young female patients and patients with severe psoriasis with a significant persistence of the desire to be accompanied.
The psoriasis affects also sexual functioning. In Gupta’s cross –sectional survey [60] of 120 inpatients, 40% reported a decline in sexual activity since the onset of psoriasis. Another survey of Sampogna and al [61] proved this sexual dysfunctioning.
In our study the sexual life has not been well exploited but psoriasis did not influence significantly the emotional life of our patients.
Anger
Anger is also among the most psychological troubles that we can observe in chronic diseases, unfortunately, it’s association with psoriasis has not been well described.
In anIndian recent study [62] of 48 psoriatic patients, the prevalence of anger was estimated: 58.3%, and in another American study, the prevalence of anger was more important: 89% [63].
In our study, we had a low prevalence of anger in comparison with others which may be explained by the religious convictions of our patients.
However, anger was significantly related to severe and old psoriasis and the use of systemic treatments in our patients.
Othersitems: like the fear of no improving and recidivism; the fear of worsening or persisting lesions or scars and the shame were items proved related to psoriasis in our population but were not described in other publications according to our knowledge.
Besides, the frustration and the desir to be accompanied were not related to psoriasis in our population and it were not described enough in the literature since there is just one descriptive American study of 75000 patients that reported the frustration in 89% of psoriatic patients [63].
CONCLUSION
In our study, Severe and old psoriasis causes an important impact on the life quality especially in young females which leads us to insist on the psychiatric approach of these patients to complete the global management of this chronic disease by the realization of a team work containing a psychologist in the special consultation of psoriasis patients.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Ouahidi FE, Hocar O, Akhdari N, Amal S, Formes graves du psoriasis: étude rétrospective de 42 casAnn Dermatol Vénéréol 2013; 140: Suppl 1S83.
2. Azfar RS, Gelfand JM, Le psoriasis et les maladies métaboliques: épidémiologie et physiopathologie. Current Opinion in Rheumatology, volCurr Opin Rheumatol 2008; 20: no.204416-422.2008:416-22
3. Denis J, Psoriasis as a chronic inflammatory syndromeAnn Dermatol Venerol 2008; 135: S296-S300.
4. Zindanc? I, Albayrak O, Kavala M, Kocaturk E, Can B, Sudogan S, Prevalence of Metabolic Syndrome in Patients with PsoriasisScient World J 2012; 312463: 1-5.
5. Dauden E, Herrera E, Impact of active and stable psoriasis on health-related quality of life: the PSO-LIFE studyActas Dermosifiliogr 2013; 104: 685-93.
6. Eskin M, Savk E, Social problem-solving, perceived stress, negative life events, depression and life satisfaction in psoriasisJ Eur Acad Dermatol Venerol 2014; 28: 1553-9.
7. Feldman SR, Disease burden and treatment adherence in psoriasis patientsCutis 2013; 92: 258-63.
8. Ekelund M, Mallbris L, A higher score on the dermatology life quality index, being on systemic treatment and having a diagnosis of psoriatic arthritis is associated with increased costs in patients with plaque psoriasisActa Dermvenereol 2013; 93: 684-8.
9. Tang MM, Chang CC, Quality of life and cost of illness in patients with psoriasis in Malaysia: a multicenter studyInt J Dermatol 2013; 52: 314-22.
10. Rabin F, Bhuiyan SI, Psychiatric and psychological comorbidities in patients with psoriasis- a reviewMymensingh Med J 2012; 21: 780-6.
11. Böhm D, Stock S, Perceived relationships between severity of psoriasis symptoms, gender, stigmatization and quality of lifeJ Eur Acad Dermatol Venereol 2013; 27: 220-6.
12. Varnj JW, Globe DR, Health-related quality of life of pediatric patients with moderate to severe plaque psoriasis: comparisons to four common chronic diseasesEur J Pediatr 2012; 171: 485-92.
13. Ganemo A, Wahlgren CF, Quality of life and clinical features in Swedish children with psoriasisPediatrdermatol 2011; 28: 375-9.
14. Basavaraj KH, Navya MA, Stress and quality of life in psoriasis: an updateInt J Dermatol 2011; 50: 783-92.
15. Shapiro J, Cohen AD, Weitzman D, Roy T, Michael D, psoriasis and cardiovascular risk factors: a case control study on inpatients comparing psoriasis to dermatitisJAAD 2012; 66: 252-8.
16. Mrowietz U, Steinz K, Psoriasis: to treat or to manage?Exp Dermatol 2014; 10: 705-9.
17. Chernyshov PV, Health related quality of life in adult atopic dermatitis and psoriatic patients matched by disease severityG Ital Dermatol Venereol 2014; Jun14
18. Bhutani T, Patel T, Koo B, A prospective,interventional assessment of psoriasis quality of life using a nonskin-specific validated instrument that allows comparison with other major medical conditionsJAAD 2013; 69: 79-88.
19. Martinez-Garcia E, Arias-santiago S, Quality of life in persons living with psoriasis patientsJAAD 2014; 71: 302-7.
20. Phillipp S, Koerber A, Nail and scalp involvement in plaque type psoriasis affects patients’ quality of life but can be improved by adequate systemic therapy: A German studyJAAD 2014; AB176.
21. Klaassen KM, Van de Kerkhof PC, Nail Psoriasis, the unknown burden of diseaseJ Eur Acad Dermatol Venereol 2014; 28: 1690-5.
22. Zampieron A, Buja A, Fusco M, Linder D, Bortune M, Piaserico S, Quality of life in patients with scalp psoriasisG Ital Dermatol Venereol 2015; 150: 309-16.
23. Coacioli S, Bruno AA, Validation of an origin questionnaire for patients with psoriatic arthritis: the psoriatic arthritis impact profile (PAIP)Clin Ter 2014; 165: 100-8.
24. Torre-Alonso JC, Gratacos J, Development and Validation of a New Instrument to Measure Health-related Quality of Life in Patients with Psoriatic Arthritis: The VITACORA-19J Rheumatol 2014; 41: 2008-17.
25. Ekelund M, Mallbris L, A higher score on the dermatology life quality index, being on systemic treatment and having a diagnosis of psoriatic arthritis is associated with increased costs in patients with plaque psoriasisActa Dermvenereol 2013; 93: 684-8.
26. Boehncke WH, Menter A, Burden of disease: psoriasis and psoriatic arthritisAm J Clin Dermatol 2013; 14: 377-88.
27. Tezel N, Yilmaz Tasdelen O, Bodur H, Gul U, Kulcu Cakmak S, Oguz ID, Is the health-related quality of life and functional status of patients with psoriatic arthritis worse than that ofpatients with psoriasis alone?Int J Rheum Dis 2015; 18: 63-9.
28. Lin TY, See LC, Quality of life in patients with psoriasis in northern TaiwanChang Gung Med J 2011; 34: 186-96.
29. Valenzuela F, Silva P, Epidemiology and quality of life of patients with psoriasis in ChileActas Dermosifiliogr 2011; 102: 810-6.
30. Hayashi M, Impact of disease severity on work productivity and activity impairment in Japanese patients with psoriasisJ Dermatol Science 2013; 72: 183-201.
31. Armstrong AW, Schupp C, Quality of life and work productivity impairment among psoriasis patients: findings from the National psoriasis foundation survey data 2003-2011Plos One 2012; 7: e52935.
32. Jankowiak B, Sekmistrz S, Satisfaction with life in a group of psoriatis patientsPost Dermatol Alergol 2013; 2: 85-90.
33. Miniszewska J, Juczynski Z, Health-related quality of life in psoriasis: important role of personal ressourcesActa Derm Venereol 2013; 93: 551-6.
34. Darjani A, Heidarzadeh A, Quality of Life in Psoriatic Patients: A Study Using the Short Form-36Int J Prev Med 2014; 5: 1146-52.
35. Sanchez-Carazo JL, Lopez-Estebaranz JL, Comorbidities and health-related quality of life in Spanish patients with moderate to severe psoriasis: a cross-sectional study (Arizona study)J Dermatol 2014; 41: 673-8.
36. Nyunt WW, Low WY, Determinants of Health-Related Quality of Life in Psoriasis Patients in MalaysiaAsia Pac J Public Health 2015; 27: NP662-73.
37. Gupta M. A, Gupta A. K, Kirkby S, Weiner H K, Pruritus in psoriasis. A prospective study of some psychiatric and dermatologic correlatesArch. Dermatol 1988; 124: 1052-7.
38. Yosipovitch G, Goon A, Wee J, Chan Y H, The prevalence and clinical characteristics of pruritus among patients with extensive psoriasisBr J Dermatol 2000; 143: 969-73.
39. Szepietowski JC, Reich A, Wiśnicka B, Itching in patients suffering from psoriasisActa Derm Venereol 2002; 10: 10216-221.
40. Amatya B, Wennersten G, Nordlind K, Patients’ perspective of pruritus in chronic plaque psoriasis: A questionnaire-based studyJ Eur Acad Dermatol Venereol 2008; 22: 822-6.
41. Stinco G, Trevisan G, Pruritus in chronic plaque psoriasis: a questionnaire-based study of 230 Italian patientsActa Dermatol Venereol 2014; 22: 122-8.
42. Reich A, Hrehorów E, Szepietowski J C, Pruritus is an important factor negatively influencing the well-being of psoriatic patientsActa Derm Venereol 2010; 90: 257-63.
43. Lewis-Beck C, Abouzaid S, Analysis of the relationship between psoriasis symptom severity and quality of life,work productivity and activity impairment among patients with moderate -to -severe using structural equation modelingPatient Pref Adheren 2013; 7: 199-205.
44. Remröd C, Sjöström K, Pruritus in Psoriasis: A Study of Personality Traits, Depression and AnxietyActa Derm Venereol 2015; 95: 439-43.
45. McDonough E, Avearst R, Depression and anxiety in psoriatic disease: prevalence and associated factorsJ Rheumatol 2014; 41: 887-96.
46. Bangemann K, Depression and anxiety disorders among psoriasis patients: Protective and exacerbating factorsHautarzt 2014; 65: 1056-61.
47. Dominguez PL, Han J, Depression and the risk of psoriasis in US womenJ Eur Acad Dermatol Venereol 2013; 27: 1163-7.
48. Bouguéon K, Misery L, Dépression et psoriasisAnn Dermatol Venerol 2008; 135: 254-8.
49. Misery L, Dépression et psoriasisAnn Dermatol Venerol 2012; 139: S53-7.
50. Kurd SK, Troxel AB, Crits-Christoph P, Gelfand J M, The risk of depression, anxiety and suicidality in patients with psoriasis: a population-based cohort studyArch Dermatol 2010; 146: 891-5.
51. Gupta MA, Gupta AK, Quality of life of psoriasis patientsJ Eur Acad Dermatol Venereal 2000; 14: 241-2.
52. Dowlatshahi EA, Wakkee M, Increased antidepressant drug exposure in psoriasis patients: a longitudinal population-based cohort studyActaderm Venereol 2013; 93: 544-50.
53. Koo J, Population-based epidemiologic study of psoriasis with emphasis on quality of life assessmentDermatol Clin 1996; 14: 485-96.
54. Delfino M, JrHolt EW, Taylor CR, Wittenberg E, Qureshi AA, Quality-of-life domains in psoriasis: a pilot studyJ Am Acad Dermatol 2008; 59: 439-47.
55. Hu SW, Holt EW, Husni ME, Qureshi AA, Willingness-to-pay stated preferences for 8 health-related quality-of-life domains in psoriatic arthritis: a pilot studySemin Arthritis Rheum 2010; 39: 384-97.
56. Smitha G, Ogoldblum OM, Vaughn McCall W, Factors affecting sleep quality in patients with psoriasisJ Am Acad Dermatol 2010; 63: 114-23.
57. Eghlileb AM, Davies EEG, Finlay AY, Psoriasis has a major secondary impact on the lives of family members and partnersBr J Dermatol 2007; 156: 1245-50.
58. Moon HS, Mizara A, Psoriasis and psycho-DermatologyDermatol Ther (Heidelb) 2013; 3: 117-30.
59. Poot F, Antoine E, A case control study on family dysfunction in patients with alopecia ariata, psoriasis and atopic dermatitisActa Derm Venereol 2011; 91: 415-21.
60. Gupta MA, Gupta AK, Psoriasis and sex: a study of moderately to severely affected patientsInt J Dermatol 1997; 36: 259-62.
61. Sampona F, Gisondi P, impairment of sexual life in patients with psoriasisDermatology 2007; 214: 144-50.
62. Sarkar S, Psoriasis and Psychiatric Morbidity: a Profile from a Tertiary Care Centre of Eastern IndiaJ Family Med Prim Care 2014; 3: 29-32.
63. Armstrong AW, Schupp C, Wu J, Bebo B, Quality of Life and Work Productivity Impairment among Psoriasis Patients: Findings from the National Psoriasis Foundation Survey Data 2003–2011PLoS One 2012; 7: e52935.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.