Pediculosis Capitis. Report of 2 cases
Patricia Chang1, Monica Vanesa Vásquez Acajabón2
1Department of Dermatology, Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala, 2Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala
Sir,
Pediculosis capitis is a common parasitic infestation of the scalp. pediculus humanus is the etiologic agent involved. We hereby present two classic cases of pediculosis capitis, for its numerous amount of parasites, in different stages of the disease. Both patients were treated with Ivermectin 200 mcg per Kg, a single dose.
CASE 1
Female patent 80 years who came to emergency due to urinary tract infection, during her clinical examination we found patient abandoned in poor hygienic conditions without any family or personal history importance.
During her clinical examination a patient in bad condition and neglected was found with the presence of numerous parasites on scalp and hair, observing many hairs with the presence of nits (Fig. 1 a–c) and microscopic view of the multiple nits (Fig. 2). Rest of the physical examination was normal
CASE 2
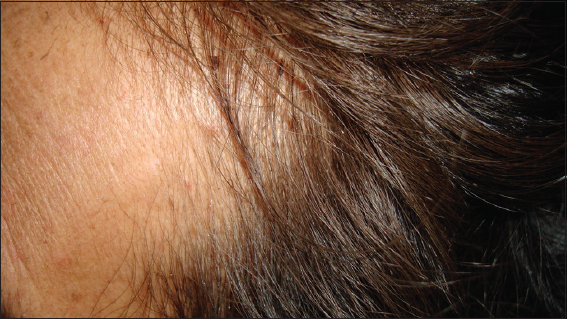
Female patient 45 years old hospitalized due to ovarian cancer, during her clinical examination head lice was seen, dermatological examination showed the presence of nits, lice walking on her hair (Fig 3), Dermatoscopic and microscopic view of parasite walking (Fig. 4) Rest of the physical examination was normal.
Both patient received ivermectin 200 mcg/kg one single dose and cured their pediculosis capitis.
DISCUSSION
Pediculosis capitis is a head lice infestation and it is an endemic parasitosis affecting many countries in the world. It is one of the most common infections in childhood, the incidence has been estimated to be 800 and 2400 new cases per 10 000 children every year [1].
The etiologic agent is the pediculus or lice, which come in three varieties, being Pediculus humanis capitis the one who causes head infection. The other two cause body and pubic infections. Pediculus human capitis can only propagate on human scalp [2,3] and if they are away from the host head for more than 2 days, they die.
Transmission of head lice requires intimate head to head contact, and it also occurs through fomites (combs, hats, clothing, etc) but it has less relevance [2,4]. It occurs that way because these wingless ectoparasites cannot jump, but they move from hair to hair quickly when the hair is dry [4].
Pruritus of the scalp is the most common symptom of head lice infestation, and it increases depending on the number of lice present and the duration of the scalp infestation [2,4]. Usually patients carry less than 20 mature head lice, which survive for 30 days [4] other signs may be reddish and itching papules frequently surrounded by erythema. These primary signs can be delayed for 4 – 6 weeks, which means that the infestation cannot be diagnosed on the early phase. In the case of reinfection, primary signs may appear within 24 – 48 hours due to the immune mediated reaction against the components of the lice saliva [2].
If the patient is not treated and continues scratching, secondary lesions as excoriations may appear, and they reduces the natural barrier function of the epidermis and this leads to a superinfection typically byStaphylococcus aureus and streptococci. The chronic infestation and persistent scratching may lead to chronic impeginization of the scalp or regional lymphadenopathy (less frequent) [2,4]. Many head lice infections cause no symptoms, and probably less than half cause itching, so this symptoms are unreliable as indicators of lice presence [3].
There are two methods to confirm the presence of pediculus human capitis on human scalp: visual inspection and diagnostic combing. In clinical practice the visual diagnosis is the most common, which consists in the direct observation of juvenile or adult head lice on the scalp. Detection combing can be performed on dry or wet hair. Combs must have parallel sided teeth and a distance of <0.3mm between teeth so that the even juvenile lice are caught [2,5]. The most important matter is to diagnose active head lice infestation in order to prescribe appropriate treatment, and the wrong diagnosis may lead to a potentially antilouse or pediculicide formulations over applied [5].
The treatment consists of manual removal and topical or systemic treatment. The first one consist in the extraction of the lice with a comb of short space between each teeth, there are also electric combs that can be used [6].
A pediculicide (lindane 1%, pyretrhin, permetrhin 1%, etc) should be applied, and all household members with a ctive infestation should be treated. A reapplication of the treatment is recommended 7-10 days after the initial procedure. In children under 2 years old, manual removal of lice, eggs and nits is recommended [4].
There are several different kinds of topical treatment available: chemical, physical and natural. Permetrhin is the most commonly used and the least toxic for humans. It should be applied during 10 to 30 minutes and the procedure must be repeated seven days later. Ivermectin may be used as oral treatment for pediculosis, and it must be administered as a single dose of 200mcg/kg.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Feldmeier H, Pediculosis captis: die wichtigste Parasitose des KindesaltersKinder – und Jugendmedizin 2006; 6249-259.
2. Feldmeier MD, Diagnosis of Parasitic Skin Diseases in Evidence Based Dermatology, USA, People’s Medical Publishing House2011; 73-6.
3. Canyon D, Speare R, Muller R, Spatial and Kinetic Factors for the Transfer of Head Lice (Pediculus capitis) Between HairsJ Invest Dermatol 2002; 119: 629-31.
4. Thappa DM, Clinical Pediatric Dermatology, India, EL SEVIER2009; 48-53.
5. Jahnke C, Bauer E, Hengge U, Feldmeier H, Accuracy of Diagnosis of Pediculosis Capitis, Visual Inspection vs Wet CombingArch Dermatol 2009; 1453: 309-13.
6. Chang P, Solares A, PediculosisDermatol Rev Mex 2013; 57: 485-90.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.