A case of onychomadesis following hand, foot, and mouth disease
Hristo Dobrev, Reni Hristova
Department of Dermatology and Venereology, Medical University, Plovdiv, Bulgaria
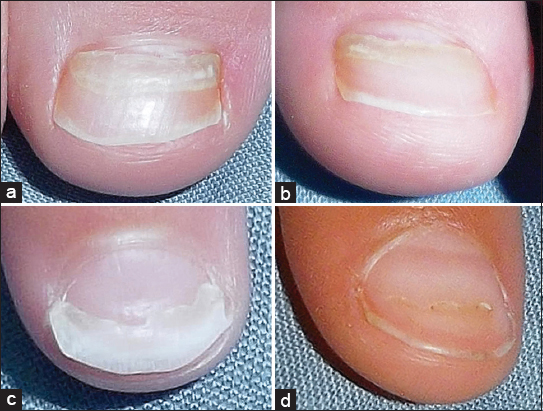
We report a 3-year-old girl with onychomadesis on big toes, 2nd left finger, and 1st right finger since 4 weeks (Fig. 1). Five weeks before that, she suffered from fever, maculopapular and vesicular rash involving his hands, feet and mouth that was diagnosed as Hand-foot-mouth disease (HFMD). Onychoscopy with polarized light and magnification ×20 well demonstrated the separation of nail plate from the proximal nail bed with subsequent shedding of the nails (Fig. 2).
HDMD is an acute infection caused most often by Coxsackie A virus type 6 and Enterovirus 71. It is more common among children than elderly. The disease is characterized by maculopapular and vesicular lesions on the hands, feet, and mouth. Onychomadesis is a shedding of the nail beginning at its proximal end, caused by temporary arrest of the function of the nail matrix. Since the first description in 2000, there are several reports of nail changes following HFMD. Recently, Shin et al. observed a group of 13 children with median age of 33 months. They found an average interval from HFMD to the nail changes 5.9 weeks (range, 3 to 12 weeks), average number of involved digits 7.4 (range, 2 to 14) and the most common involvement of left great toe (85%). The nail changes varied from transverse ridging of the nail plate (Beau’s lines) up to complete nail shedding (onychomadesis). The mechanism of nail involvement remains unclear but it is considered that the inhibition of nail matrix proliferation is due to direct inflammation spreading from skin eruptions around nail. This was supported by the observation of Shikuma et al. that onychomadesis was developed only on the fingers and toes having cutaneous eruptions around nails. Onychomadesis occurring after HFMD is temporary with spontaneous normal regrowth [1–4].
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Clementz G, Mancini A, Nail matrix arrest following hand-foot-mouth disease: a report of five childrenPediatric Dermatology 2000; 17: 7-11.
2. Shin JY, Cho BK, Park HJ, A Clinical Study of Nail Changes Occurring Secondary to Hand-Foot-Mouth Disease: Onychomadesis and Beau’s LinesAnn Dermatol 2014; 26: 280-3.
3. Shikuma E, Endo Y, Fujisawa A, Tanioka M, Miyachi Y, Onychomadesis Developed Only on the Nails Having Cutaneous Lesions of Severe Hand-Foot-Mouth DiseaseCase Rep Dermatol Med 2011; 2011: 324193.
4. Chiriac A, Birsan C, Chiriac AE, Pinteala T, Foia L, Hand, Foot and Mouth disease in northeastern part of Romania in 2012Our Dermatol Online 2013; 4: 226-9.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.