Porokeratosis of the scrotum
Khalifa E. Sharquie1, Raafa K. AL-Hayani2, Waqas S. Abdulwahhab2
1Department of Dermatology & Venereology, College of Medicine, University of Baghdad, Baghdad, Iraq, 2Department of Dermatology &Venereology, Baghdad Teaching Hospital, Baghdad, Iraq
ABSTRACT
Porokeratosis (PK) is disorder of keratinization characterized by annular lesions surrounded by raised sharply marginatedkeratotic borders with a characteristic histopathological finding named cornoid lamella. PK of genitalia is very rare condition and mostly reported among Asian population. The aim of present report is to document a new patient with localized scrotal PK with his father suffering from the same disease in the scrotum.
Key words: Porokeratosis; Cornoid lamella; Genitalia; Neurodermatitis
INTRODUCTION
PK is disorder of keratinization characterized by annular lesions surrounded by raised sharply marginatedkeratotic borders with a characteristic histopathological finding named cornoid lamella. It consists of a heterogeneous group of disorders inherited in a autosomal dominant fashion. PK has a wide variety of manifestations including classical plaque-type porokeratosis of mibelli, disseminated superficial actinic porokeratosis, linearporokeratosis, porokeratosispalmaris, plantaris, etdisseminata and punctate porokeratosis [1].
In Iraq, a special variety of pk has been reported affecting the face only called solar facial porokeratosis [2]. Localized pk of the genitalia is a rare in occurrence with 24 cases reported in the literature [3]. The aim of present report is to document anew patient with his father suffering from localized scrotal PK.
CASE REPORT
55-year-old male patient presented to Department of Dermatology, Baghdad Teaching Hospital in 20-8-2012 suffering from severely itchy genital lesions. Since 1982 the patient described a rash on the scrotum which was gradually enlarging in size and increasing in number. Also he mentioned the occurrence of exactly the similar disease of his father (dead) in genital area and this in favor of autosomal dominant inheritance. All the lesions are persistent with no history of spontaneous resolutions of any them. On examination, numerous papules, nodules and plaques distributed over the scrotum (>40 lesions) with none of them on the shaft of penis (Fig. 1). Those lesions were indurated skin colored while others were dark with typical annular configurations as the borders seemed more active while the center had the tendency towards atrophy. Some of the lesions showed thickened surface with pigmentation without the typical annular ring of the most of the lesions and looked like neurodermatitis (Fig. 2).
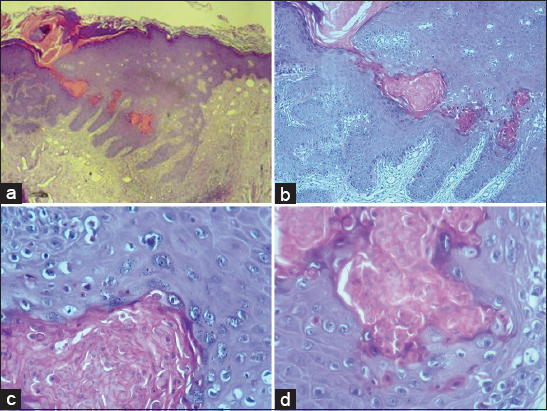
The histopathology of the disease as follow: theepidermis wasacanthotic with basket weave hyperkeratosis. There was invagination of epidermis by column of keratin reaching the basal layer of epidermis. At the site of invagination there was absence of granular layer. This column consisted of parakeratotic cells, forming a typical feature of cornoidlamella. Many individual dyskeratoticcells were seen under the base of lamella reaching almost the basal layer of epidermis. While the dermis consisted of many dilated blood vessels with severe inflammatory reaction at the base of cornoid lamella, consisting of many lymphoid cells. In addition pieces of manydartos muscles were observed in the dermis (Fig. 3).
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
Porokeratosis of genitalia is very rare condition and mostly reported among Asian population [3–5]. The present report is the first case study that is being reported in Arab region. Family history of the present case was positive as his father had the similar condition and this might support the autosomal dominant inheritance like other types of pk. Itching is a prominent feature of present case and this was similarly reported [4]. There are many dermatosis involvingthe genital area like psoriasis, lichen planus and dermatitis and these are usually associated with itching. Lichen simplex is commonly superimposed on the top of these skin diseases [6]. Accordingly the present case was diagnosed and treated for 30years by most of dermatologists as case of lichen simplex chronicus. In most of reported genital pk, the lesions were scanty (1-3) while in our patient, numerous lesions were seen that widely distributed over the scrotum. Malignant transformation of pk had been reported [7], but fourtounitly no malignant changes were observed in present case.
There are no effective therapies of pk but many treatment had been suggested like topical steroid, cryotherapy, electrocautry, Co2 laser and others. We recommend Co2 laser removal as one of most effective modality [8,9], in order to relieve the patient complaint and to prevent the possibility of malignant changes.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Spencer LV, Porokeratosis last accessed on 2006 oct 9Available from: http://www.emedicine.com/derm/topic 343 htm.
2. Sharquie KE, AL-Baghdady BA, Solar facial porokeratosisJ Dermatol 2003; 30: 216-21.
3. Valdivielso-Ramo M, Genital porokeratosis: Case ReportsActas Dermosifiliog 2008; 99: 217-20.
4. Chen T, Chou Y, Chen C, Kuo T, Hong H, Genital porokeratosis: a series of 10 patients and review of the literatureBr J Dermatol 2006; 155: 325.
5. Sengupta S, Das J, Gangopadhyay A, Porokeratosis confined to the genital area: a report of three casesIndian J Dermatol Venereol Leprol 2008; 74: 80.
6. Lynch PJ, Lichen simplex chronicus (atopic/neurodermatitis) of the anogenital regionDermatol Ther 2004; 17: 8.
7. Maubec E, Duvillard P, Margulis A, Bachollet B, Degois G, Avril M-F, Common skin cancers in porokeratosisBr J Dermatol 2005; 152: 1389.
8. Trcka J, Pettke-Rank CV, Brocker EB, Hamm H, Genitoanocruralporokeratosis following chronic exposure to benzeneClin Exp Dermatol 1998; 23: 28-31.
9. Huang SL, Liu YH, Chen W, GenitoglutealporokeratosisJ Eur Acad Dermatol Venerol 2006; 20: 899-900.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.


Comments are closed.