Intravascular fasciitis in foot – a rare entity in a rare site
Ashitha Nanaiah1, Padmapriya Jaiprakash1, Annappa Kudva2, Kanthilatha Pai1
1Department of Pathology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India, 2Department of Surgery, Kasturba Medical College, Manipal University, Manipal, Karnataka, India
ABSTRACT
Intravascular fasciitis is a rare lesion involving blood vessels, showing proliferation of myofibroblasts, involving the superficial or deep fascia. We report a case of middle aged male patient presenting with callosity over the toe, with features of intravascular fasciitis, which is a rare site.
Key words: Intravascular; Fasciitis; Foot
INTRODUCTION
Intravascular fasciitis is a rare benign condition, involving arteries and/or veins, characterized by reactive myofibroblastic proliferation arising from the superficial or deep fascia [1]. Intravascular fasciitis was first described by Patchefsky and Enzinger in 1981 [2]. It is a rare variant, seen in less than 3% of nodular fasciitis [3]. It usually occurs in the small veins and arteries of the limbs, trunk, head and neck region. Only a few cases involving the foot have been reported [4].
CASE REPORT
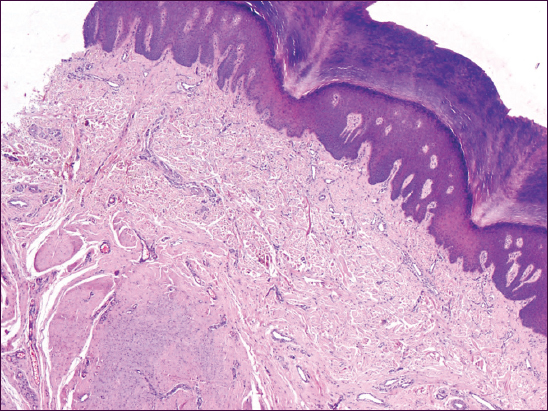
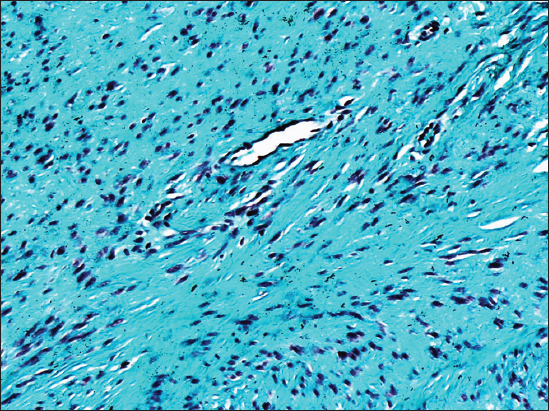
A 56 year old male was referred to the surgical outpatient with a callosity over the left great toe and a skin patch on the left thigh. The clinical diagnosis was papilloma and corn respectively. Laboratory investigations revealed high cholesterol and triglyceride levels, with all other parameters being within normal limits. The patient underwent excision under local anesthesia and specimen was sent for histopathological examination. The gross specimen consisted of a skin covered tissue bit, which weighed about 2 gm, measured 3×0.5×1 cm. The cut section showed gray white, grey brown and haemorrhagic areas. Microscopy showed hyperkeratotic stratified squamous epithelium overlying dermal papillae along with few blood vessels with slit–like lumen, (Fig. 1) surrounded and compressed by an ill-circumscribed lobulated lesion composed of a mixture of fibroblasts and myofibroblasts in a myxoid background (Fig. 2), suggestive of intravascular fasciitis. Masson Trichrome stain showed the fibrous nature (Fig. 3) of the lesion. The associated papilloma of right thigh was histologically diagnosed as fibroepithelial polyp of Molle.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
Intravascular fasciitis is a rare tumour with only thirty three cases being currently reported in literature [1]. Intravascular fasciitis is most commonly seen in adolescent and young adult patients. Females and males are equally affected [3]. The predisposing factors may include thrombosis, trauma and pregnancy-related hormonal changes [1]. The most common anatomic locations of the lesion are the upper extremities, head and neck, occurring rarely in the foot [3]. The size of the lesions vary from 0.6 to 5 cms. The patient usually presents as a painless subcutaneous mass which is gradually increasing in size for a duration varying from 2 weeks to 8 years [3,5].
Microscopically, intravascular fasciitis is characterized by plump spindle cells arranged in intersecting fascicles, a storiform pattern, or in a haphazard manner. The lesion may be present inside the lumen or associated with the walls of arteries or veins of all sizes. The separation of mass from the vessel wall may cause clefts [3,5]. Patchefsky and Enzinger reported that among their cases, the soft tissue component often was more prominent than the vascular component [2]. Though the infiltrative growth pattern resembles a sarcoma, it can be differentiated by the absence of significant cytologic pleomorphism and abnormal mitotic figures and the overlying epidermis is usually intact [1]. The background stroma varies from a dense hyalinized to edematous, myxoid appearance. Often associated are scattered multinucleated giant cells, lymphocytes and red blood cells [2].
The proliferative cells in intravascular fasciitis are of myofibroblastic phenotype, being positive to both vimentin and a-smooth muscle actin expression and negative for keratin, S100 protein, desmin, CD31, CD34, and c-kit. The multinuclear giant cells were CD68 positive, confirming the histiocytic origin. CD31 and CD34 can demonstrate the highly vascular stromal background and the vascular location of the lesion. Special stains for elastic fibers can be used to demonstrate the walls of associated vessels [2].
The pathogenesis of intravascular fasciitis is currently under study. According to Patchefsy and Enzinger [5], the lesion was due to the proliferation of myofibroblasts from the walls of systemic arteries and veins and they attributed the frequent extension into perivascular connective tissue to the ‘‘field effect’’ of myofibroblastic transformation [2]. The myofibroblastic origin of the spindle cells is confirmed by immunohistochemistry. Factors initiating myofibroblast proliferation may be preceding trauma, thrombosis, and high levels of estrogen and has to be further studied [1].
In the present case, the diagnosis was made by histology and use of special stains like Masson Trichrome. Differential diagnosis include sarcoma, benign fibrous histiocytoma, organizing thrombus, pyogenic granuloma, peripheral nerve tumours, spindle cell carcinoma, spindle cell melanoma, myxoid liposarcoma, fibrosarcoma and leiomyosarcoma [4]. This entity has been described as ‘‘pseudosarcoma’’ due to the misinterpretation of intravascular growth as vascular invasion by a sarcoma in addition to increased mitotic activity, involvement of muscle and infiltrative borders of soft tissue [2].
The clinical behavior of this lesion is usually benign but a few cases have been reported to recur after excision. Since the soft tissue component comprises a much greater proportion of the tumor than the vascular component, diagnosis may be difficult in small biopsy specimens [1]. If blood vessel walls cannot be seen easily, the multinodular or serpentine growth pattern may be useful along with special stains for elastic fibers and smooth muscle [2].
CONCLUSION
Intravascular fasciitis is a rare variant of nodular fasciitis involving with blood vessels. The recognition of intravascular growth is required for diagnosis on small biopsy specimens and may be facilitated by special stains for elastic fibers or immunohistochemical stains for vascular markers. This case is reported with the intention of creating awareness of this lesion to avoid misdiagnosis and aggressive treatment.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Zheng Y, George M, Chen F, Intravascular fasciitis involving the flank of a 21-year-old female: a case report and review of the literatureBMC Research Notes 2014; 7: 118.
2. Chi AC, Dunlap WS, Richardson MS, Neville BW, Intravascular Fasciitis: Report of an Intraoral Case and Review of the LiteratureHead Neck Pathol 2012; 6: 140-5.
3. Enzinger Weiss Sharon W. Weiss, John R. Goldblum, Benign fibroblastic/myofibrolblastic proliferationsSoft tissue tumours 2008; 5th ed. Elsevier; 175-225.
4. Sugaya M, Tamaki K, Does Thrombosis Cause Intravascular Fasciitis?Acta Derm Venereol 1987; 369-70.
5. Patchefsky AS, Enzinger FM, Intravascular fasciitis: a report of 17 casesAm J Surg Pathol 1981; 5: 29-36.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.