Rosacea-like tinea faciei
César Bimbi12, Piotr Brzezinski3
1Dermatological Comittee of State Medical Council of Rio Grande do Sul Brazil, 2Brazilian Society of Dermatology[3] Department of Dermatology, Military Support Unit, Ustka, Poland
ABSTRACT
Tinea faciei, is a facial superficial mycosis. The most frequent etiological agents are Microsporum canis, Trichophyton rubrum and T. tonsurans. It is often overlooked when considering the differential diagnoses of Rosacea. The most well known dermatology textbooks list acne, LE, perioral dermatitis, nasal sarcoidosis, carcinoid syndrom and other conditions but do not mention TF.
We describe 3 patients with lesions that clinically appeared to be Rosacea.
Key words: Tinea; dermatophytoma; Rosacea
INTRODUCTION
Tinea faciei (TF) is a dermatophyte infection of glabrous skin of the face sometimes displaying a wide and variable range of clinical features from erythema, patches, induration, vesicles, pustules, papular and circinate lesions. So, this infection is often deceptive and may clinically mimic other facial dermatoses. Discoid lupus erythematosus, lymphocytic infiltration, seborrheic dermatitis, granuloma annulare and contact dermatitis are the most frequent misdiagnoses [1].
We describe 3 patients with lesions that clinically appeared to be Rosacea.
CASE REPORT
Case 1
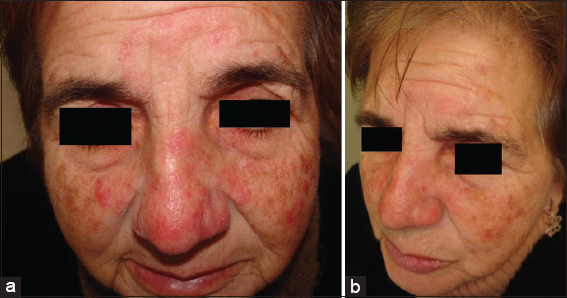
A 66-year-old woman complained of a 2 years history of facial eruptions – “ – an allergy “ – that had initiated by the nose (Fig. 1a). She was treated firstly with antibiotics for acne rosacea, but with no improvement, and then prednisone (20 mg daily) still for presumed acne rosacea was tried, also unsucessfully (Fig. 1a). Physical examination revealed extensive erythematous lesions on the face with some pustules. Clinically, the lesions appeared to be acne rosacea. The well defined delimited edges of the forehead lesion lead to the suspicion of tinea, and KOH examination was positive. The patient improved considerably in just two weeks of teatment. We used oral terbinafine and ciclopirox olamine cream.
Case 2
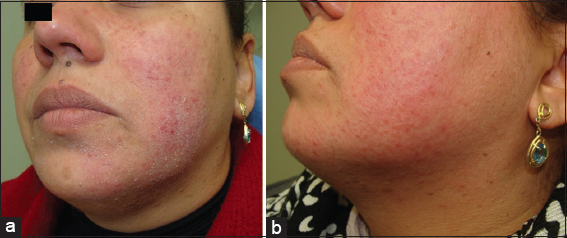
A 32-year-old woman came to the office with facial erythema to which had been prescribed cortisone creams and again no improvement was noted by the patient (Fig. 2a). Clinically, the lesions seemed to be irritant dermatitis, eczema or rosacea. This time, instead of well defined edges of case 1-patient, we could note a fine dusty scaling that suggested micotic scales and KOH examination was again positive. We used oral terbinafine and ciclopirox olamine cream. The patient returned 8 days after and already a good improvement was easily detected (Fig. 2b).
Case 3
A 68-year-old woman came to the office with facial erithema, telangiectasia and some papulo-granulomatous indurated lesions to which again had been prescribed betamethasone creams (Fig. 3). Clinically, the lesions seemed a bit of sarcoidosis or rosacea, but not tinea. Scales were scrapped and KOH examination was again hyphae positive. We used oral terbinafine and ciclopirox olamine cream. The patient still did not return but improvement is expected since this medication works well when direct mycologic test is positive.
DISCUSSION
Superficial fungal infections of the face seem not to be sufficiently or routinely investigated as differential diagnosis possibility and as a result, some facial dermatoses are often incorrectly diagnosed. As many as 70% of patients with tinea faciei are initially misdiagnosed as having other dermatoses. In a 20-year survey of tinea faciei, Nicola et al [2] examined 107 cases of tinea faciei. Typical forms were 57.1% whereas in 42.9% atypical forms were observed, mainly mimicking discoid lupus erythematosus (9 cases), polymorphous light eruption (8 cases) and Rosacea-like presentations [1,2]. In another study [1], in 100 cases of tinea faciei in adults, 52 mimicked a discoid lupus erythematosus, 15 lymphocytic infiltratation and four polymorphous light eruption
Although tinea faciei is tinea itself, some authors claim it as a distinct entity. Facial anatomy, physiology characteristics, exposure to sunlight, repeated washing and the use of cosmetics often determine atypical clinical presentation that leads to incorrect diagnosis.
“Four-in-one” anti: fungal-bacterial-histamine+ corticosteroid topical preparations are widely used by nondermatologists in the treatment of superficial fungal infections, but may be associated with persistent/recurrent infections [3].
Therapy with terbinafine associated with topical anti-fungal therapy leads to healing within 3–6 weeks without relapse or side effects. An added benefit of using ciclopirox and terbinafine is their anti-inflammatory effect [4].
Our patients had pruritic erythematous facial eruptions and had been treated for other dermatosis but with no improvement. Direct microscopy revealed multiple hyphae in all 3 cases. The first patient is a poor elderly woman coming from a peripheral village where it is difficult to get lab tests, so for practical purposes and the patient immediate relief we chose the commencement of treatment even to the detriment of a culture examination in order not to delay the relief of the symptoms. The patient improved considerably in just 8 days. Complete resolution is expected after 6 weeks of therapy. The same option was made for the other 2 patients.
Tinea faciei accounts for 3–4% of cases of tinea corporis and is often initially misdiagnosed and treated as other dermatoses in as many as 70% of patients [5]. It may be easily diagnosed or excluded by KOH preparation. It is important that we are aware of the possibility of tinea faciei and that diagnostic procedures are put in place to identify, or eliminate tinea facei from the final diagnosis.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Alteras I, Sandback M, David M, Segal R, 15-year survey of tinea faciei in the adultDermatologica 1988; 177: 65-9.
2. Nicola A, Laura A, Natalia A, Monica P, A 20-year survey of tinea facieiMycoses [serial online] 2010; 53: 504-8.
3. Alston SJ, Cohen BA, Braun M, Persisten/t and recurrent tinea corporis in children treated with combination antifungal/corticosteroid agentsPediatrics 2003; 111: 201-3.
4. Baxter DL, Moschella SL, Johnson BL, Tinea of the faceArch Dermatol 1965; 91: 184-5.
5. Torres-Guerrero E, Ramos-Betancourt L, Martínez-Herrera E, Arroyo-Camarena S, Porras-López C, Arenas R, Dermatophytic blepharitis due to Microsporum gypseum. An adult variety of tinea faciei with dermatophytomaOur Dermatol Online 2015; 6: 36-8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.