A clinical study of the cutaneous manifestations of hyperthyroidism in Kashmir valley – India
Mohamad Abid Keen1, Mohamad Hayat Bhat2, Iffat Hassan1, Parvaiz Ahmad Shah2, Yasmeen Jabeen Bhat1
1Departments of Dermatology, STD & Leprosy, Government Medical College, University of Kashmir, Srinagar, India, 2Departments of Medicine, Government Medical College, University of Kashmir, Srinagar, India
ABSTRACT
Introduction: Thyroid hormones are instrumental in regulating the health and appearance of skin and when the thyroid gland becomes underactive or overactive, a variety of skin problems result. These dermatologic manifestations may occur secondary to the abnormal thyroid hormone levels or due to the presence of thyroid autoantibodies that interact with skin components.
Aims: The present study was designed to ascertain the varied cutaneous manifestations of hyperthyroidism.
Methods: This was a hospital based cross sectional study conducted over a period of one year. A total of forty diagnosed cases of hyperthyroidism constituted the subject material for the study and were evaluated for the presence of any cutaneous manifestation.
Results: In our study group of 40 patients, the predominant cutaneous symptom was increased sweating (80%), followed by heat intolerance (42.5%). The predominant cutaneous sign in hyperthyroid patients was increased skin temperature, noticed in 47.5% of patients. This was followed by soft, smooth and velvety skin (37.5%), palmar erythema (35%), fine thin hair (22.5%) and hyperpigmentation (10%).
Conclusions: The interaction between thyroid gland and skin is very complex. So, dermatologists need to be cognizant of the ways in which these two organs interact.
Key words: Thyroid hormones; Cutaneous; Hyperthyroidism
INTRODUCTION
Endocrine disorders may occasionally present with cutaneous manifestations. Thyroid disorders have a high prevalence in medical practice and are associated with a wide range of diseases with which they may or may not share the etiological factors. One of the organs which best shows this wide range of clinical signs is the skin [1]. In thyroid diseases, many symptoms arise on the skin and most of these symptoms disappear with the treatment of thyroid disease.
Some dermatological skin findings and diseases may be the first symptoms of thyroid diseases. Since most of these cutaneous manifestations of thyroid disorders are nonspecific, these do not allow diagnosis without the estimation of endocrine function [2].
There is a very limited data available in literature regarding the cutaneous changes associated with hyperthyroidism. So, the present study was designed to ascertain the varied cutaneous manifestations of hyperthyroidism.
METHODS
This study was a hospital based cross-sectional clinical study conducted in collaboration with the endocrinology division of SMHS Hospital (associated teaching hospital of Government Medical College Srinagar). The present study was conducted over a period of six months from February 2010 to July 2010. A total of forty consecutively diagnosed cases of hyperthyroidism were included in the present study. There was no age limit for inclusion in the study. The diagnostic criteria for hyperthyroidism were:
- Clinical manifestations of hyperthyroidism
- Depressed or negligible TSH levels
- Elevated serum T3 and T4 levels.
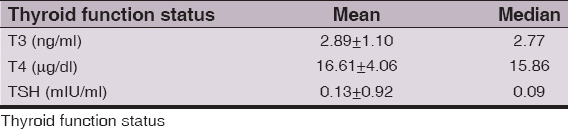
Diagnosis of hyperthyroidism was made by a suppressive TSH level in blood. Levels of T3 and T4 were also measured in blood and if one of both were elevated, the diagnosis was confirmed.
These patients were evaluated for the presence of any cutaneous manifestation. A detailed medical history pertaining to hyperthyroidism was elicited in each case with particular reference to the cutaneous complaints including duration, history of evolution and progression. An informed consent was taken from each patient, after which a general physical examination, systemic examination and a detailed dermatological examination was carried out and the relevant details recorded and tabulated. Apart from routine laboratory investigations, thyroid function tests (TSH, T3 and T4) were done by electro-chemiluminesense assay (ECLIA). Statistical analysis of the data was performed by appropriate statistical methods using Statistical Package for Social Sciences (SPSS Version 17) and inferences were drawn.
Ethics
This study was performed on human subjects; thus, all patients were aware of the presence of the study and they were fully informed about the drug and its side-effects.
RESULTS
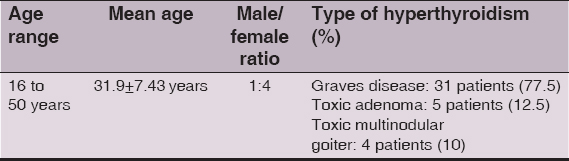
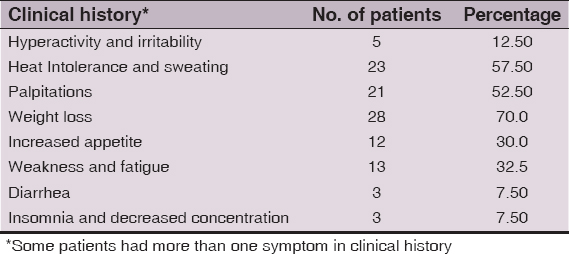
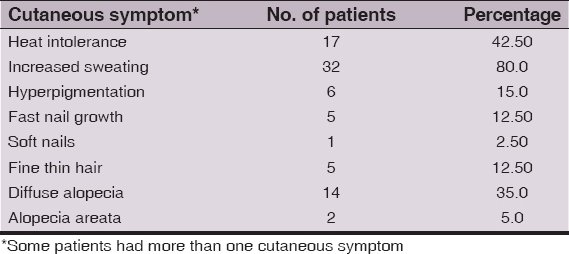
A total of 40 hyperthyroid patients were included in the study. Age range, mean age, male/female ratio and type of hyperthyroidism is depicted in (Table 1). The medical complaints in the history in our study group are depicted in (Table 2). The most common cutaneous symptom was increased sweating, complained by a total of 32 (80%) patients. This was followed by heat intolerance, reported by 17 (42.5%) patients. Diffuse alopecia was complained by a total of 14 (35%) patients and hyperpigmentation by 6 (15%) patients. Fast nail growth and fine thin hair were reported as a cutaneous symptom by 5 (12.5%) patients each. Soft and friable nails were noticed by just 1 (2.5%) patient. Alopecia areata was reported by 2 (5%) patients. Most of these patients had more than one cutaneous symptom (Table 3). We noticed 5 (12.5%) hyperthyroid patients, who had no cutaneous symptom as such.
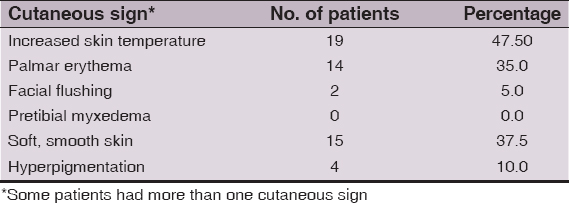
The predominant cutaneous sign in hyperthyroid patients was increased skin temperature, noticed in 19 (47.5%) patients. This was followed by soft, smooth velvety skin, which was seen in 15 (37.5%) patients. Palmar erythema (Fig. 1), was noticed as a cutaneous sign in 14 (35%) patients, while as hyperpigmentation in 4 (10%) hyperthyroid patients. The least common cutaneous sign was facial flushing, seen in only 2 (5%) patients. We did not observe pretibial myxedema in any patient. There were 9 (22.5%) hyperthyroid patients with no cutaneous signs on examination. The cutaneous signs in our patients are tabulated in (Table 4).
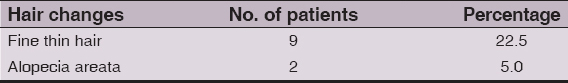
The predominant finding on examination of hair was fine thin hair with diffuse non-scarring alopecia (Fig. 2), seen in a total of 9 (22.5%) patients. Alopecia areata (Fig. 3) was noticed in just 2 (5%) patients. No hair changes were noticed in 29 (72.5%) of our hyperthyroid patients. Hair changes are depicted in (Table 5).
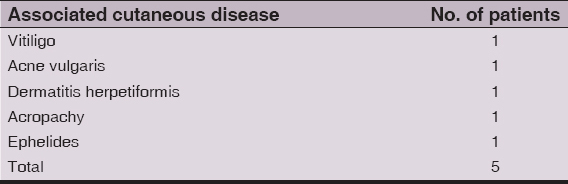
In our study group, the predominant nail change was fast nail growth, seen in 3 (7.5%) patients. Distal onycholysis (Plummer’s nail) was not noticed in any of our patients. The other associated cutaneous diseases which we noticed in the patients in the hyperthyroid group were vitiligo, acne vulgaris, dermatitis herpetiformis, acropachy (Fig. 4) and ephelides. The associated cutaneous diseases are depicted in (Table 6).
Mean and median values of TSH, T3 and T4 in our patients are shown in (Table 7).
In our study group, majority of the patients were on antithyroid drugs, few of them were receiving radioactive iodine and 2 patients were scheduled for surgery for toxic thyroid nodules. Most of these patients were lost to follow up, so the effect of various treatment modalities over various cutaneous manifestations of hyperthyroidism could not be ascertained.
DISCUSSION
The skin in hyperthyroidism is warm, moist and smooth, bearing a resemblance to infantile skin. Warmth can be attributed to increased cutaneous blood flow and peripheral vasodilatation, which may also lead to the commonly noticed facial flushing and palmar erythema seen in hyperthyroid patients. Generalized hyperhidrosis may be noted with a predilection for palms and soles.
Scalp hair is soft and fine and sometimes accompanied by diffuse, non-scarring alopecia [3]. Approximately 5% of patients may present with nail findings. Characteristic, though not pathognomonic, is the “Plummer’s nail” with a concave contour and distal onycholysis. Hyperpigmentation may be seen in a distribution resembling that seen in Addison’s disease, and is particularly pronounced in darker skin types [4]. Hyperpigmented eyelids have been described (Jellinek’s sign).
Grave’s disease is characterized by the cutaneous findings of hyperthyroidism in addition to distinctive cutaneous features including pretibial myxedema or dermopathy (0.5 to 4% of patients) and acropachy (1%). Clinical presentation may vary from a “peau d orange” appearance to the extensive infiltration resembling elephantiasis verrucosa nostra. Most often, lesions appear as bilateral asymmetric, raised, firm plaques or nodules varying in color from pink to purple-brown and sometimes accompanied by woody induration [5].
Grave’s dermopathy occurs less frequently than ophthalmopathy, and although it is usually seen to occur with ophthalmopathy, it may occur alone [5]. The vast majority of patients with dermopathy have Grave’s disease. Histologically, there is an accumulation of hyaluronic acid in the dermis more so than in the subcutis.
Thyroid acropachy is a triad consisting of distal clubbing, soft tissue swelling of hands and feet, and periosteal new bone formation. The first, second, and fifth metacarpals, the proximal phalanges of hands, and first metatarsal and proximal phalanges of feet are the most commonly affected. Pathognomic radiographic osseous changes are comprised of periosteal reaction of a lamellar type paralleling the diaphysis and has been described as “feathery”. The vast majority of cases are associated with Grave’s disease.
In our study group of 40 patients, there were 32 (80 %) females and just 8 (20 %) males. This was in concordance with the observations made by Rai D et al in their study, in which the percentage of females was found to be 83% [6]. This observation of female preponderance may be due to an increased association of autoimmune disorders in females, autoimmunity being an important cause of hyperthyroidism.
The most common cutaneous symptom in our hyperthyroid patients was increased sweating, seen in 80% of cases, followed by heat intolerance(42.5%). Comparable results were obtained by Rai D et al in their study. Hyperpigmentation was a cutaneous symptom in 15% of patients. Hair changes reported by our patients included fine thin hair (12.5%), diffuse alopecia (35%) and alopecia areata (5%). These findings were in contrast to the study by Rai D et al, in which hair changes were reported by 64% of cases [6]. Nail changes reported by our patients included fast nail growth (12.5%) and soft nails (2.5%).
We observed that the most common cutaneous sign in our hyperthyroid group of patients was increased skin temperature, seen in 47.5% of cases, followed by soft smooth skin (37.5%) and palmar erythema (35%). Ideally skin temperature can be assessed by either a wired skin electrode or a wireless skin temperature data logger or a more sophisticated thermal imaging system. Due to the non-availability of either of these in our institution, we could not record the skin temperature of the patients.
Hyperpigmentation was observed in 10% of hyperthyroid patients. None of our patients had pretibial myxedema, while as Leonhardt JM et al reported pretibial myxedema to be present in 0.5-4% of patients of Grave’s disease [7]. In our study, we observed that the predominant finding on examination of hair in hyperthyroid patients was fine thin hair (22.5%) and alopecia areata, noticed in 5% of cases. In other study, they noticed hair changes in just 2.6% of their cases [8]. In our hyperthyroid group, we observed that the predominant nail change was fast nail growth, seen in 7.5% of our cases. Distal onycholysis (Plummer’s nail) was not noticed in any of our patients whereas in some studies, nail changes were noticed in 5% of the cases [9]. We noticed acropachy in 1 patient (2.5%), while as some studies have reported acropachy to be present in 0.1-1% of cases [7].
Associated cutaneous manifestations in our hyperthyroid patients included vitiligo, seen in 1 patient similar to other studies [10]. We found one patient of hyperthyroidism with dermatitis herpetiformis as an associated cutaneous diseases similar to that in other studies [11,12].
We also found 1 hyperthyroid patient each with acne vulgaris and ephelides. We believe that these findings in our patients were coincidental.
CONCLUSIONS
We conclude that there definitely exists an association between cutaneous signs and symptoms with hyperthyroidism but this interrelationship is complex. Advances in molecular and immunological studies have heightened our understanding of the pathogenesis of some of the aspects of these disorders, although innumerable questions remain.
Limitations
- Our sample size was not large
- The complaints of the patients were subjective
- There was no follow up of our patients in order to ascertain the effects of various antithyroid treatment modalities on the cutaneous manifestations of hyperthyroidism.
Suggestions
Cutaneous signs suggestive of hyperthyroid state should be followed up by routine thyroid function studies. Should the thyroid disease be classified as autoimmune, the clinician should be vigilant for any of the potential associated disorders for which the patient may be at risk throughout the patient’s entire life. Optimal management of the cutaneous manifestations of hyperthyroidism relies on an understanding of their pathophysiology, early recognition and treatment.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Niepomnisczhe H, Ahad RH, Skin disorders and thyroid diseasesJ Endocrinol Invest 2001; 24: 628-38.
2. Burman KD, Mc Kinley-Grant L, Dermatologic aspects of thyroid diseaseClin Dermatol 2006; 24: 247-55.
3. Freinkel RK, Freinkel N, Fitzpatrick TB, Eisen AZ, Wolff K, Cutaneous manifestations of endocrine disordersDermatology in general medicine 1987; 3rd ed. New York: Mc Graw Hill; 2063-81.
4. Banba K, Hyperpigmentation caused by hyperthyroidism: difference from pigmentation of Addison’s diseaseClin Exp Dermatol 1999; 24: 196-9.
5. Anderson CK, Miller OF, Triad of exopthalmos, pretibial myxedema and acropachyJ Am Acad Dermatol 2003; 48: 970-2.
6. Rai D, Wahid Z, Zaidi AN, Cutaneous manifestations of thyroid diseaseJ Pak Assoc Dermatol 2000; 10: 8-22.
7. Leonhardt JM, Heymann WR, Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, Cutaneous manifestations of other cutaneous diseasesFitzpatrick’s dermatology in general medicine 2003; 6th ed. New York: McGraw Hill; 1664-1665.
8. Ramanathan M, Abidin NM, Muthukumarappan M, The prevalance of skin manifestations in thyrotoxicosis – a retrospective studyMed J Malaysia 1989; 44: 324-8.
9. Heymann WR, Cutaneous manifestations of thyroid diseasesJ Am Acad Dermatol 1992; 26: 885-902.
10. Ochi Y, De Groot L. J, Vitiligo in Grave’s diseaseAnn Int Med 1969; 71: 935-7.
11. Zettinig G, Weissel M, Flores J, Dudczak R, Vogelsang H, Dermatitis herpetiformis is associated with atrophic but not with goitrous variant of Hashimoto’s thyroiditisEur J Clin Invest 2000; 30: 53-7.
12. Cunningham MJ, Zone JJ, Thyroid abnormalities in dermatitis herpetiformis. Prevalence of clinical thyroid disease and thyroid autoantibodiesAnn Int Med 1985; 102: 194-6.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.





Comments are closed.