Bilateral linear nevus comedonicus on eyelids – A rare presentation
Vijay Zawar1, Swati Zawar2, Antonio Chuh3
1Department of Dermatology, Tulsi Eye Hospital, Nashik, Maharashtra State, India, 2Department of Ophthalmology, Tulsi Eye Hospital, Nashik, Maharashtra State, India[3] School of Public Health, The Chinese University of Hong Kong and the Prince of Wales Hospital, Hong Kong
ABSTRACT
We describe a female child with linear comedone-like lesions over both the eyelids which histologically confirmed Naevus Comedonicus. She only partially responded to topical tretinoin cream. There was no clinically evident overt systemic association in our case.
Key words: Developmental defects; Eye lids; Hair Follicle; Nevus comedonicus; Tretinoin
INTRODUCTION
Naevus Comedonicus (NC) is an uncommon developmental defect of the pilosebaceous apparatus (or rarely, may be of the sweat duct) characterised by group of slightly elevated papules which have central, dark, firm hyperkeratosis plug resembling a comedo [1]. It was first described by Kofmann in 1895 [2]. It commonly affects scalp, face, trunk and uncommonly the genitalia [3], palms and soles [4]. Usually it is unilateral and an isolated cutaneous defect. Widespread cutaneous involvement or giant lesions are exceptional as are the systemic associations such as skeletal defects, cataract, cerebral anomalies [1,5,6] and arterio-hepatic dysplasias (Alagille syndrome) [7].
CASE REPORT
An 8-years old female child was brought by her parents for asymptomatic “string of black dots” on both of her eyelids noticed since six months which were slowly progressive.
She was otherwise healthy. There was no history of similar eruptions in the other family members. Her past health was good. There was no preceding history of trauma or eyelid surgery. There is no history of convulsions, headache or jaundice. There is no history of usage of mascara, eyeshadows or other cosmetics. We also specifically asked about the history of topical application of steroid creams.
On examination, there were multiple, firm, pin-head sized papules with a keratotic, pigmented centre with linear configuration on the upper eyelids starting 1cm supero-medially to the medial canthus, extending upto the medial third of the length of upper eyelids on each side. (Fig. 1). The lesions had more or less, a symmetrical distribution. These were non-tender and not adherent to the deeper structures. There were no lesions on other areas of skin. Her gait and posture was normal. Her complete ocular, cutaneous and systemic examinations were normal.
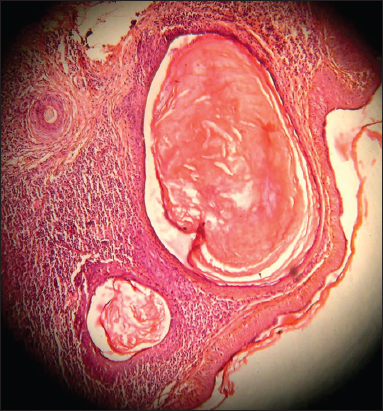
Skin biopsy revealed multiple dilated follicular infundibuli below the epidermis, surrounded by dense mononuclear inflammatory infiltrate. Individual dilated follicular opening was filled with eosinophilic, keratinous material (Fig. 2). Overlying epidermis was unaffected. Her baseline work up including blood counts, sugar, urinalysis and liver function tests was normal. She was prescribed topical tretinoin cream 0.025% twice daily, which resulted in partial flattening of comedones at the end of three weeks. She was further lost to follow-up.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
NC usually has unilateral, grouped or linear configuration. Symmetrically bilateral linear affection is rare [8]. NC may result into cosmetic disfigurement especially when the lesions are large and are on the exposed areas such as face. NC may be confused at times with the other linear eruptions such as epidermal naevus (which may actually be associated with NC), linear adnexal tumours, lichen planus, porokeratosis, lichen striatus, lipoid proteinosis or tattoo reactions. However, a distinctive clinical appearance of linear papules with central dark, keratin plug is virtually diagnostic. In atypical cases, the diagnosis is resolved on histopathogical examination. The lesions of NC may occasionally have acute inflammatory component with or without secondary infection, may then result into scarring.
NC is usually treated with topical retinoic acid. However, it may be fairly resistant to the topical therapy [8–11]. Topical treatments with keratolytics including salicylic, lactic and tartaric acids [8], pore-strip packs [10], Ammonium lactate solution [9] and Tacalcitol [8] dermabrasion; manual extraction of the comedones [11] and surgical excision [11] with or without plastic reconstruction are the other modalities of the treatment. Tissue expansion has been tried in one patient with giant NC [11].
Ophthalmologists may be the first physician to see cutaneous problems such as NC in their patients. It is, therefore, prudent to know of the conditions which are diagnostic by their morphological appearance so as to facilitate early clinical diagnosis and associated serious systemic defects, if any. The patient of NC may be informed about possible complications like inflammation, abscess formation which may result in scar formation and likely onset of cataracts in young age [12].
To our best knowledge, only one case of bilateral NC on eyelids is reported on pubmed in a 79-yrs old male patient [13]. The cause in this patient was unclear. In contrast, our case of NC in a child truely represents a developmental defect and therefore, is certainly unique.
In conclusion, bilateral linear NC on the upper eyelids is an extremely rare presentation. It causes significant cosmetic concern, which may be associated with anxiety of the parents of the affected children.
Consent
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Patrizi A, Neri I, Fiorentini C, Marzaduri S, Nevus comedonicus syndrome: a new pediatric casePediatr Dermatol 1998; 15: 304-6.
2. Kofmann S, Ein Fall von seltener Localisation und Verbreitung von ComedonenArch Derm Syph 1895; 32: 177-8.
3. Gonzalez-Martinez R, Marin-Bertolin S, Martinez-Escribano J, Amorrortu-Velayos J, Nevus comedonicus: report of a case with genital involvement: Cutis1996; 58: 418-9.
4. Harper KE, Spielvogel RL, Nevus comedonicus of the palm and wrist. Case report with review of five previously reported casesJ Am Acad Dermatol 1985; 12: 185-8.
5. Filosa G, Bugatti L, Ciattaglia G, Salaffi F, Carotti M, Naevus comedonicus as dermatologic hallmark of occult spinal dysraphismActa Derm Venereol 1997; 77: 243.
6. Seo YJ, Piao YJ, Suhr KB, Lee JH, Park JK, A case of nevus comedonicus syndrome associated with neurologic and skeletal abnormalitiesInt J Dermatol 2001; 40: 648-50.
7. Woods KA, Larcher VF, Harper JI, Extensive naevus comedonicus in a child with Alagille syndromeClin Exp Dermatol 1994; 19: 163-4.
8. Wakahara M, Kiyohara T, Kumakiri M, Kuwahara H, Fujita T, Bilateral nevus comedonicus: efficacy of topical tacalcitol ointmentActa Derm Venereol 2003; 83: 51.
9. Milton GP, DiGiovanna JJ, Peck GL, Treatment of nevus comedonicus with ammonium lactate lotionJ Am Acad Dermatol 1989; 20: 324-8.
10. Inoue Y, Miyamoto Y, Ono T, Two cases of nevus comedonicus: successful treatment of keratin plugs with a pore stripJ Am Acad Dermatol 2000; 43: 927-9.
11. Marcus J, Esterly NB, Bauer BS, Tissue expansion in a patient with extensive nevus comedonicusAnn Plast Surg 1992; 29: 362-6.
12. Whyte HJ, Unilateral comedo nevus and cataractArch Dermatol 1968; 97: 533-5.
13. Mendoza PR, Jakobiec FA, Townsend DJ, Bilateral nevus comedonicus of the eyelidsOphthal Plast Reconstr Surg 2013; 29: e95-8.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.

Comments are closed.