Study of basal cell carcinoma and its histopathological variants
Shivanand Gundalli1, Rutuja Kolekar2, Amit Kolekar3, Vikrant Nandurkar4, Kaveri Pai5, Sunita Nandurkar6
1Department of Pathology, S. Nijalingappa Medical College, Bagalkot, Karnataka, India,, 2Department of Obstetrics and Gynaecology, S. Nijalingappa Medical College, Bagalkot, Karnataka, India, 3Department of Surgery, ABVRH, Sawangi, Wardha, Maharashtra, India, 4Department of Surgery, Devraj urs Medical College, Kolar, Karnataka, India, 5Department of Anaesthesia, ABVRH, Sawangi, Wardha, Maharashtra, India, 6Department of Obstetrics and Gynaecology, Devraj urs Medical College, Kolar, Karnataka, India
ABSTRACT
Introduction: Basal Cell Carcinoma (BCC) typically affects older individuals with Predilection for sun-exposed skin (face, hands) small, well-circumscribed, pearly tan-gray papule devoid of scale lesions enlarge with time and tend to ulcerate (rodent ulcers). Basal cell nevus syndrome: multiple basaloid hamartomas on the cutaneous surface associated with palmar keratotic pits, jaw cysts, and basal cell carcinomas in non–sun-exposed locations. BCC rarely metastasize; when they do, the primary lesion is usually advanced.
Aim: The aim of our study was to determine the frequency of various types of BCCs encountered in our practice, to delineate the spectrum in our setup and to determine the different histological patterns, anatomical location, site predilection, and age and sex incidence.
Materials and methods: The present study was carried out in the department of pathology in a tertiary care centre. The study was prospective (2years) as well as retrospective (5 years) and was done during the period of September 2004 to September 2011 i.e., 7 years.
Results: In the present study 21 cases of BCC were seen and accounted for 26.25% of all the malignant tumors of skin.
Conclusions: In the present study majority (85%) of the lesions of BCC were located on head and neck region, average age of cases of basal cell carcinoma was 65.6 years, and solid type of BCC was most common type.
Key words: Basal cell carcinomas; Study; Age
INTRODUCTION
The first description of basal cell carcinoma (BCC) was by Jacob in 1827. BCC is the most common malignant skin tumor, but the incidence in Asian races is lower than in the white race. The incidence of BCC in Indian literature ranges from 12% to 30%. BCC is seen almost exclusively on hair bearing skin especially on the face. BCC generally occurs in adults. BCC may develop in children under following circumstances: Nevoid basal cell epithelioma syndrome, in pre-existing organoid nevus and in xeroderma pigmentosa [1].
There are five clinical types of Basal cell carcinoma which include [2]
- Nodulo-ulcerative
- Pigmented
- Morphea-like or fibrosing Basal cell carcinoma
- Superficial (multifocal)
- Fibroepithelioma of Pinkus.
Scriverer Y et al in his study on 13,457 patients with BCC have shown that nodular and morphoeiform types predominate on the forehead where as the trunk is the most common site for the superficial type [3].
Histopathology: BCC tend to share the common features of a predominant basal cell type, peripheral palisading of cell nuclei, a specialized stroma, and clefting artifact between the epithelium and the stroma.
Prognosis and predictive factors: BCC are locally invasive tumours and metastases occur in less than 1 in 10,000 tumours. Morbidity is increased with deeply invasive tumours which may extend into the deep tissue to bone and follow fusion planes particularly on the face where they follow nerves through bony channels. Morbidity also increases with neglected tumours that may measure more than 10 cm in diameter and have been described as giant basal cell carcinomas. Multiple recurrences with deep residual tumour on the head may be associated with particular morbidity as basal cell carcinomas can ultimately penetrate the cranium. Increased recurrences are associated with infiltrative, morphoeic and micronodular BCC as surgical margins may be underestimated. BCC recurrences are more common in lesions on the nose and nasolabial fold, this may be in part due to the difficulty in achieving adequate margins in these sites. Tumours recurring after radiotherapy are usually aggressive and infiltrative [4].
MATERIALS AND METHODS
The present study was carried out in the department of pathology in a tertiary care centre. This study included tumours of epidermis along with melanocytic tumours and adnexal tumours of skin including secondaries without restricting the study to any particular age limit. Mesenchymal tumours of skin, haematological tumours of skin, neural tumours of skin, nonneoplastic lesions of skin and all tumours arising from mucosal area of mucocutaneous junction such as glans penis and eyelid margin were excluded. The study was prospective (2years) as well as retrospective (5 years) and was done during the period of September 2004 to September 2011 i.e., 7 years. Data for retrospective study was obtained from departmental records, tissue blocks and slides. Data for prospective study was obtained from clinical records, tissue specimens, tissue blocks and slides Clinical details were obtained and maintained according to the proforma. All the biopsies and resected specimens received in the histopathology section were immediately fixed in 10% formalin for 24 hours. Gross features of the specimen were noted. Multiple sections of the specimen were taken. Then they were processed and embedded in paraffin wax. Three-five microns thick sections were prepared and then stained with Haematoxylin & Eosin. Detailed study of the sections was performed under the light microscope and then the final diagnosis was given.
Ethical clearance: Ethical clearance has been obtained from Ethical committee of institution. Statistical methods applied:
Following Statistical methods were applied in the present study.
- Number and percentage
- Descriptive statistics.
Prior to the study, every patient gave written consent to the examination and biopsy after having been informed about the procedure and aim of the study.
RESULTS
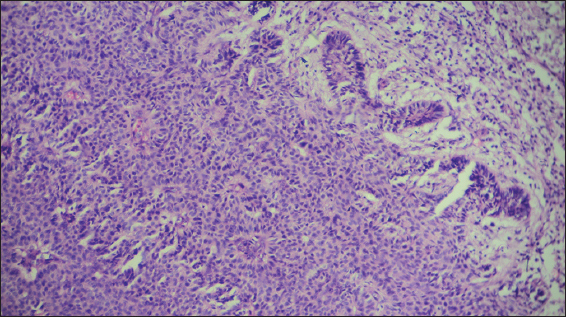
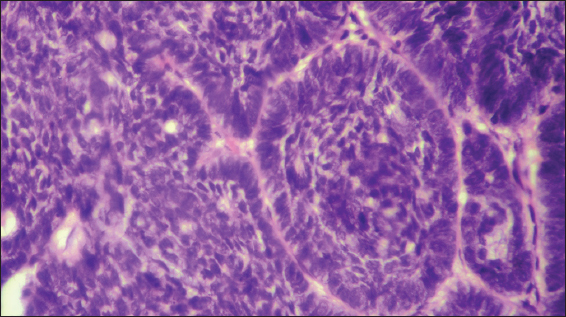
In the present study 21 cases of BCC were seen and accounted for 26.25% of all the malignant tumours of skin (Figs 1 – 6). Maximum number of cases were observed in 7th decade. Mean age of patients was 65.6 years.
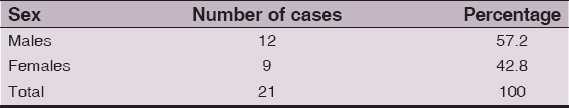
Table 1 shows sex distribution of BCC. This table shows predominance of BCC in males with male to female ratio 1.3:1.
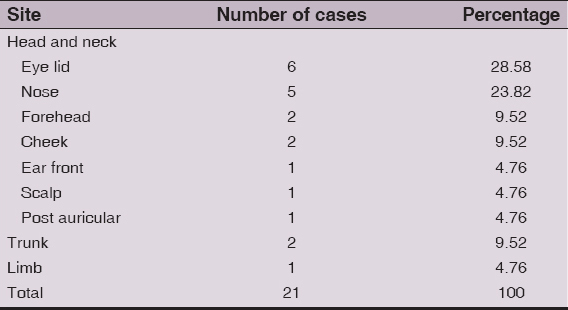
Table 2 show site wise distribution of BCC. As shown in this table, 85% of cases of BCC were located on head and neck region and majority were seen in the eye lids.
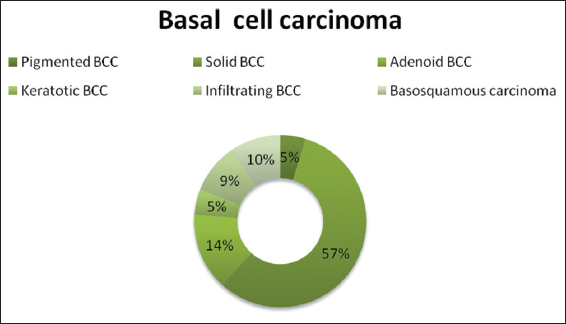
In figure 4 we presented histological types of BCC. As shown in the above chart, in the present study solid variant of BCC was the commonest (57.14%) histological type followed by adenoid type, infiltrating type and basosquamous type. BCC with no differentiation were categorized as solid basal cell carcinoma. Adenoid BCC showed cellular arrangement suggesting tubular structures. The cells were arranged in intertwining strands resulting in a lacelike pattern. Keratotic basal cell carcinoma showed keratinisation in the form of horn cysts. In the infiltrating variant of BCC the basaloid cells were arranged in cords and showed deep infiltration in the dermis. Two cases of basosquamous carcinoma were found in the present study. Both of them showed combined features of basal cell carcinoma and squamous cell carcinoma. Both cases were females of 63 and 65 years age presented as ulcer over the scalp and ulcer on left nostril.
Table 3 show age distribution of malignant tumours of skin compared with BCC. As shown in this table maximum number of cases that is 63 (78.75%) among 80 malignant BCC sincluding secondaries belonged to the age group of 6th to 8th decade.
DISCUSSION
Frequency of occurrence of BCC with respect to malignancies of skin in various other studies show table 4.
In the present study the frequency of occurrence of basal cell carcinoma was 26.25% of all the malignant tumours of skin. The frequency of occurrence of basal cell carcinoma in other studies ranged from 18% to 30%. Our findings are comparable to others studies.
In the present study majority (85%) of the lesions of BCC were located on head and neck region, which is similar to the observations of Solanki et al [5] (94%), Chakravorthy et al [6] (90%) and Budhraja et al [7] (78%).
In the present study male to female ratio in the patients of BCC was 1.33:1. Solanki, et al found a male to female ratio of 1.26:1. Hence our findings are comparable with Solanki, et al [5].
And in present study the average age of cases of BCC was 65.6 years. Scrivener, et al noted average age as 65 years. Hence our findings are comparable to Scrivener, et al [3].
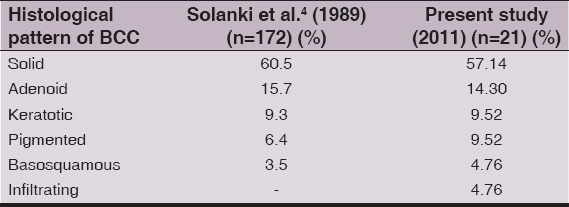
Table 5 shows comparison of histological types in BCC.
In the present study solid type of BCC was most common type which is comparable to the study of Solanki et al [5] as he also noted the solid type as most common type of BCC in his study of 172 cases.
BCCs constitute a small but significant proportion of patients with cancer. The skin is a complex organ. Because of its complexity a wide range of diseases develop from the skin including tumors from surface epidermis, epidermal appendages and dermal tissue.
The diagnosis of BCCs presents unique difficulties, in part, related to the wide variety of tumors and the complicated nomenclature. The study of histogenesis of the basal cell carcinomas is interesting, fascinating and challenging because of wide range of differentiation.
Histopathological study is one of the most valuable means of diagnosis in dermatopathology and the diagnosis of BCCs can be done by correlating clinical features, gross and histological appearances.
The present study emphasizes the various patterns of skin neoplasms in this geographic location in and around city.
Finally the quintescence of the subject of study of basal cell carcinomas is it’s vastness, it’s enormity and its interesting histomorphology.
CONCLUSIONS
In the present study majority (85%) of the lesions of BCC were located on head and neck region, average age of cases of basal cell carcinoma was 65.6 years, and solid type of BCC was most common type.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Kirkham N, Tumours and cysts of epidermisIn Lever’s histopathology of skin 2005; 9th ed. Philadelphia: Lippincott Raven; 805-866.
2. Mckee PH, Brenn T, Tumours of surface epithelium. In pathology of skinElsevier Mosby 3rd ed. 1153-1237.
3. Scrivener Y, Grosshans Cribier B, Variations of BCC according to gender, age, location and histological typeBr J Dermatol 2002; 147: 41-7.
4. LeBoit PE, Burg G, Weedon D, Sarasin A, Pathology and genetics of skin tumoursIn World health organisation classification of tumours 2006; Lyon: IARC press; 1-300.
5. Solanki RL, Anand VK, Gaur SK, Arora HL, Gupta R, Neoplasms of hair follicleIndian J Dermatol Venereol Leprol 1989; 55: 33-7.
6. Charkravorthy RC, Choudhuri DR, Malignant neoplasms of the skin in Eastern IndiaIndian J Cancer 1968; 5: 133-44.
7. Budharaja SN, Pillai VCV, Periyanagam WJ, Kaushik SP, Bedi BMS, Malignant neoplasms of skin in Pondicherry- a study of 102 casesIndian J Cancer 1972; 284-95.
Notes
Source of Support: Nil
Conflict of Interest: None declared.





Comments are closed.