Giant lipoma of the upper back: A case report
Sancar Serbest1, U?ur Tiftikçi1, Engin Kesgin2, Hac? Bayram Tosun3
1Department of Orthopaedics and Traumatology, Faculty of Medicine, K?r?kkale University, K?r?kkale, Turkey, 2Department of Orthopaedics and Traumatology, Anamed Private Hospital, Mersin, Turkey, 3Department of Orthopaedics and Traumatology, Faculty of Medicine, Ad?yaman University, Ad?yaman, Turkey
ABSTRACT
Lipomas are the most frequent benign tumors of mesenchymal origin. Lipomas may become giant masses, due to usually asymptomatic, painless, slow growing soft tissue tumours. They are more common 5-10 times in males and appearing to avarage age fifth decade of life. Although differantion between lipoma and liposarcoma of low grade malignancy conflict, total surgical excision is adequate treatment. ?n this case report, we present 70 years old male with giant back of left shoulder mass as lipoma after surgical excision and histopathological examination.
Key words: Giant lipoma; Shoulder; Surgery
INTRODUCTION
Lipomas originated from the adipose tissue are common, encapsulated and benign neoplasms [1]. They are seen more frequently in the back, shoulder and neck regions. Although their clinical diameters are a few centimeters, they can reach to much larger sizes. Generally, they are seen as a slow-growing, asymptomatic, and painless mass. Even though distribution of men and women is equal, often detected in the fifth decade [2]. To classify lipomas as the giant, they must have 10cm width at least or weight above 1000g [3].
In this study, the lipoma case reached to giant sizes on the localized right shoulder posterior was presented.
CASE REPORT
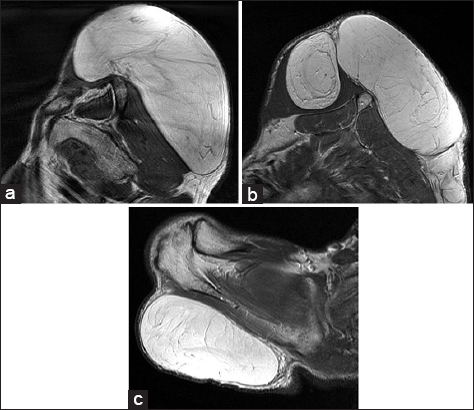
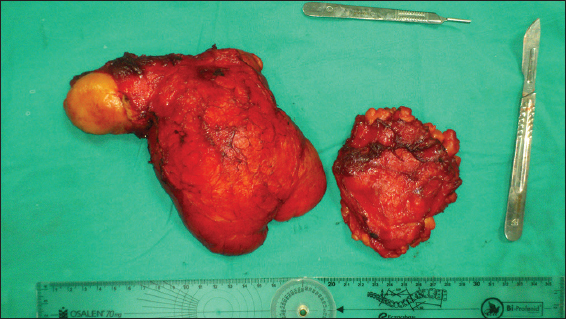
Seventy years old male patient consulted our polyclinic with painless, slow-growing tumescence complaints which has been existed on the right shoulder for six years. There were also a limitation of shoulder movements and lying back difficulty complaints and no any additional disease or previous trauma history of the patient. During the physical examination, soft viscous mass in the form of two lobes -approximately 25×20×6 cm and 8×10×10 cm- was detected on the dorsal right shoulder (Figs 1a – c). In the radiography, an increase was detected in the soft tissue density in the right shoulder area (Fig. 2). At the contrast-enhanced magnetic resonance imaging (MRI) findings, T1 and T2 weighted images had the same signal with normal adipose tissues. In the fat suppressed images, there were similar kind of suppression with lipomatous tissue (Figs 3a – c). In the MRI of the shoulder joint posterior, there was a view that contains septation and diffuse at the subcutaneous tissue. The mass showed an extension into supraspinotus muscle. At the inferior of the mass, there was also an another lobe which was diffuse, septated, and located at subcutaneous tissue (Fig. 4). Under general anesthesia, it was entered into the incision along the extension of the mass to includes the right shoulder joint of the patient who was lying on the left side. The mass was dissected from subcutaneous tissues, the other part extended into supraspinotus muscle was removed as a mass with the dimensions of 20×18×6 cm. A mass which was 8×8×3 cm and localized as seperate lobe was excised (Fig. 5). During the one year follow-up, no recurrence was observed at the patient who was previously reported with the giant lipoma in the histopathological study.
DISCUSSION
Although etiopathenogenesis of lipomas has not been demostrated completely, endocrine, genetic, and traumatic factors are the most accepted causes. Genetically, the possible correlation between lipoma formations and deletion and translocation of 12. chromosome has been informed [4]. The stimulation of secondary inflammatory mediators, fat necrosis, and release of local growth factors are the other factors in charge of the trauma which occurs during the differentiation of mesenchymal precursor cells to adipocytes at the subcutaneus tissues [5].
Lipomas are soft viscous, slow-growing, mobile masses which show no sensitivity during the physical examination, create no differences above the skin, may be seen with various sizes depend on their localization and time, and exist for a long time [6]. By reaching large sizes in the body part where they located, they may lead to not only aesthetic but also functional problems. Patients usually consult a doctor because of poor appearence depending on the size of lesion [7].
According to histopathological characteristics, bening lipomatous lesions could be classified as a classic lipoma, a fibrolipoma, an angiolipoma, an infiltrative lipoma, a pleomorpfic lipoma, an intramuscular lipoma and a hibernoma. The study of Üstünda? and Dervişo?lu [8] which covered 843 cases of lipomatous tumor series reported that the malignity was detected only at 44 cases and 75% of benign cases were diagnosed as classic lipomas.
Radiography, ultrasound, computed tomography (CT), and MRI are examination methods used in lipoma diagnosis. Although the radiography is not much sensitive, low density fat opacities can be seen. Ultrasound is easily accessible and the first preferred method because of that it is noninvasive. In the ultrasound, lipomas are generally seen as well circumscribed encapsulated masses. Even though their echogenicities are highly variable, they are iso or hyperechoic according to the muscle. The vascularization is not monitered at Doppler examination. In CT examination, the lipoma is observed as an encapsulated, low density homogen mass. A low density is the definitive diagnostic for the lipoma. MRI imaging is the most frequently used method because of the fact that it has high soft tissue resolution and can show the distribution and depth. Lipomas are not stained with any contrast substance in MRI and CT examinations [9].
The general treatment form of lipomas is a surgical excision. They can be excised due to aesthetic or functional causes. They do not show recurrence after total resection and for this reason additional treatment is not needed [7]. Liposuction is another treatment modality used rarely for giant lipomas [10]. We performed total resection to our case and called the patient for controls. Postoperative consultations at forth and twelfth months were evaluated as normal. To conclude, despite the fact that lipomatous lesions have benign characteristics clinically, defining the histopathological nature of lipomas is absolutely necessary. Difficulty of diagnosis in certain lesions which were evaluated as a simple lipoma by clinicians should be considered.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Kumar V, Abbas AK, Fausto N, Robbins SL, Cotran RS, Robbins and Cotran pathologic basis of disease2005; XV: 7th edition. Philadelphia: Elsevier Saunders; 1317.
2. Kohler S, Bolognia Jl, Jorizzo Jl, Rapini RP, Muscle, adipose and cartilage neoplasmsDermatology 2003; Edinburgh: Mosby; 1883-98.
3. Ghidirim G, Mishin I, Gutsu E, Gagauz I, Danch A, Russu S, Giant submucosal lipoma of the cecum: report of a case and review of literatureRom J Gastroenterol 2005; 14: 393-6.
4. Turc CC, Dalcin P, Boghosian L, Breakpoints in benign lipoma may be at 12q13 or 12q14Cancer Genet Cytogenetic 1988; 36: 131-3.
5. Copcu E, Sivrioglu N, Posttraumatic lipoma: Analsis of 10 cases and explanation of possible mechanismsDermatol Surg 2003; 29: 215-8.
6. Copcu E, Sivrio?lu N, Posterior cervical giant lipomasPlast Reconstr Surg 2005; 115: 2156-7.
7. Silistreli OK, Durmus EU, Ulusal BG, Oztan Y, Gorgu M, What should be the treatment modality in giant cutaneus lipomas? Review of the literature and report of 4 casesBr J Plast Surg 2005; 394-8.
8. Üstünda? N, Dervişoglu S, Recently described lipomatous tumours and our 11 year-experience on lipomatous tumoursCerrahpaşa J Med 2003; 34: 119-26.
9. Cree Gaskin M, Clyde A, Helms. Lipomas, lipoma variants and well-differentiated liposarcomas (atypical lipomas): Results of MRI evaluations of 126 consecutive fatty massesAJR Am J Roentgenol 2004; 182: 733-9.
10. Nichter LS, Gupta BR, Liposuction of giant lipomasAnn Plast Surg 1990; 24: 362-5.
Notes
Source of Support: Nil
Conflict of Interest: None declared.



Comments are closed.