Balanoposthitis as a cutaneous marker of diabetes mellitus in an apparently healthy male
Virendra Saoji1, Amit Achliya2
1Department of Dermatology, Dr. PDM Medical College, Amravati, India, 2Medicine Dermatology, Dr. PDM Medical College, Amravati, India
ABSTRACT
Background: Balanoposthitis inflammation of the glans penis, which often involves prepuce is a common condition and are usually managed symptomatically without considering a possible association diabetes. Acquired balanoposthitis may be the first clinical presentation of undiagnosed diabetes mellitus.
Methods: We enrolled 100 subjects with balanoposthitis with no history of diabetes mellitus in the past. Random blood sugar was done in all subjects, those with random blood sugar more than 140 mg/dl underwent fasting and 2 hour post prandial blood sugar estimation.
Result: Out of 100 patients having balanitis,7 patients were detected to have diabetes mellitus for the first time, while another 4 patients were found to have impaired glucose tolerance for the first time.
Conclusion: In conclusion, we must bear in mind that balanoposthitis may be the first clinical sign of diabetes mellitus in males and hence appropriate blood glucose testing should be carried out when assessing men with balanoposthitis.
Key words: Balanitis; Balanoposthitis; Diabetes mellitus
INTRODUCTION
Diabetes mellitus is a major public health problem in India and its incidence is rapidly increasing and it has had an increasing impact on urological practice. Balanitis defined as inflammation of the glans penis, which often involves prepuce (known as balanoposthitis) is a common condition and are usually managed symptomatically without considering a possible association diabetes. Acquired balanoposthitis may be the first clinical presentation of undiagnosed diabetes mellitus [1].
AIMS
To establish the incidence of undiagnosed diabetes mellitus in men presenting with balanitis.
MATERIALS AND METHODS
Study was conducted in the period 01.01.2014 to 31.10.2014. Patients were enrolled in the study if they met following criteria:
- Age 20-70 years.
- Clinical findings consistent with the diagnosis of Balanoposthitis.
- No History of Diabetes Mellitus in the past.
A total of 100 patients were enrolled in the study who met the above mentioned criteria. Each eligible patient then underwent thorough physical examination and local examination of Genital region. Patients were then subjected to laboratory investigations CBC, Random Blood Sugar and complete urine analysis. Those patients with abnormal Random blood sugar (more than 140 mg/dl) underwent Fasting and 2 hour post prandial blood glucose estimation on subsequent day. Diabetes Mellitus and Impaired Glucose Tolerance was diagnosed as per ADA guidelines.
Balanoposthitis was treated by personal hygiene, oral fluconazole 150 mg once a week for 2 week, cefpodoxime 200 mg twice daily for five days and metronidazole 400 mg thrice daily for five days. Newly detected Diabetic patient were given medication for diabetes as per ADA guidelines.
Ethics
This study was performed on human subjects; thus, all patients were aware of the presence of the study and they were fully informed about the drug and its side-effects.
RESULT
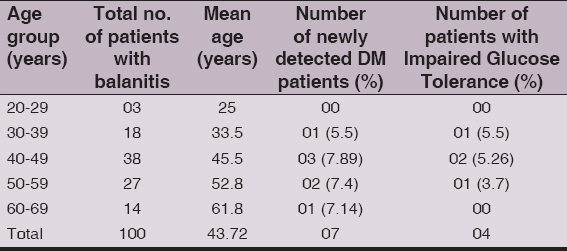
Baseline demographic characteristics of 100 enrolled patients are summarized in (Table I). Mean age was 43-72 years. Maximum number of patients (38) were in the age group 40-49 years, followed by 27 in age group 50-59 years. Out of 100, Eleven patients had increased random blood sugar levels and these eleven patients underwent fasting and post prandial blood sugar estimation. Out of eleven patients with increased random blood sugar,7 patients were newly detected to have Diabetes Mellitus (Fasting Blood Glucose > 126 mg/dl and/or Post prandial blood glucose >200 mg/dl) and 4 patients were detected to have impaired glucose tolerance(Post prandial blood glucose 140-199 mg/dl). Maximum number of newly detected diabetic patient (03) were in age group 40-49 years (Tabl. 1).
Table 1: Demographic charecteristics and incidence of newly detected diabetes patients in study group
Thus Type 2 Diabetes Mellitus was newly diagnosed in 7% men presenting with balanitis and no history of a glycaemic disorder in past. A further 4% were diagnosed with impaired glucose tolerance. Urine analysis was positive for glucose in all new diagnoses of glycaemic disorders.
DISCUSSION
Balanitis is defined as inflammation of the glans penis, which often involves the prepuce (balanoposthitis). Balanitis can occur at any age, but the prevalence of specific etiologies is age dependent. It is a common condition affecting 11% of male genitourinary clinic attendees [1] and it can be a recurrent or persistent condition. Etiology is usually fungal or bacterial, but remains undetermined in a large proportion of patients. Balanitis symptoms often evolve over three to seven days. The condition may present as pain, tenderness, or pruritus associated with small erythematous lesions on the glans and/or the prepuce (Fig.1). These lesions can be ulcerated or scaly (Fig.2). Thick foul smelling purulent exudate is often produced. Edema may develop if symptoms are allowed to progress without treatment. The combination of inflammation and edema can result in adhesions, with adherence of the prepuce to the glans. Persistent inflammation may result in scarring of the foreskin. Treatment of Balanitis is often empirical, and involves use of antifungal and antibiotic agents. If not properly treated, this process can evolve into a tightening of the prepuce, known as phimosis.
Figure 1: Patient with balanitis
Figure 2: Patient with ulcerative balanits
It is well established that diabetes is related to balanoposthitis and acquired phimosis [2]. Acquired balanoposthitis can be the first clinical sign of DM in uncircumcised males. In a recent study from Britain, 26% of adult patients with balanitis were found to suffer from type II DM [3]. The diagnosis of DM was made for the first time in 8% of these patients which means that balanoposthitis in an apparently healthy male is a cutaneous marker of DM. Another 15% of males had impaired glycemic control. Diabetes caused balanoposthitis is more of a problem in India than sexually acquired balanoposthitis. In our study of 100 patients with balanitis, Type 2 Diabetes Mellitus was newly diagnosed in 7% men presenting with balanitis and no history of a glycaemic disorder in past. A further 4% were diagnosed with impaired glucose tolerance. These findings are consistent with previous studies.
Chih-Chun Ke et al reported that a volcano-like appearance of balanoposthitis with generalized erythema, a dry glazed appearance, acquired phimosis and surrounding fissures may be a typical finding in diabetic balanoposthitis [4]. The presentation may be more severe in patients with underlying diabetes mellitus than those without, with edema and fissuring of the foreskin, which may become non-retractile [5]. Preputial fissures, a hallmark of this condition, can be explained by the accumulation of advanced glycation end products (AGEs) in the foreskin [6]. AGEs content is increased in particular by inadequate glycemic control in diabetics. AGEs impair production of collagen and extracellular organization that is associated with a lowered hydroxyproline content and superoxide dismutase activity. In addition, this causes deleterious effects such as a greater impairment and alteration of biomechanical properties of the skin, namely, elasticity and hydration. There is also loss of surface lipids of skin due to impairment of sebaceous gland function and a tendency of reduced hydration in the stratum corneum. Repeated retracting the stiff foreskin during urination or sexual intercourse can be responsible for vertical fissuring of the foreskin, and this can further lead to fibrosis in the form of phimosis.
Balanoposthitis should be viewed as a manifestation of an immunocompromised state, which can occur at any age [7], and need not be limited to sexually active men.
Numerous studies have reported the growing impact of diabetes on dermatological practice with erectile dysfunction, voiding dysfunction and urinary tract infections all more common in diabetic than non-diabetic patients [8]. In 2006 Drivsholm et al have found that abnormal thirst (63%), fatique (61%), frequent urination (53.9%), unintended weight loss (34.8%), general itching (27.2%) and balanitis (12%) were the most common prediagnostic symptoms in diabetic patients [9]. These clinical conditions might be the initial presentation of previously undiagnosed diabetes. It is important to recognize this condition early to avoid later complications.
CONCLUSION
In conclusion, we must bear in mind that balanoposthitis may be the first clinical sign of diabetes mellitus in males. Diagnosing Diabetes in these men may not only reduce operative complications, but also prompt appropriate diabetic management and reduce long term complications. Therefore it is important that appropriate blood glucose testing should be carried out when assessing men with balanoposthitis.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Hattem VS, Bootsma AH, Thio HB, Cleve Clin J Med 2008; 75: 772-7.
2. Verma SB, Wollina U, Looking through the cracks of diabetic candida balanoposthitis!Int. J Gen Med 2011; 4: 511-3.
3. Bromage SJ, Crump A, Pearce I, Primroses as a presenting feature of diabetesBJU Int 2008; Feb101: 338-40.
4. Chen C-H, Chen J-J, Wang C-C, Balanoposthitis with a Volcano-like Appearance May be the First Clinical Presentation of Undiagnosed DiabetesIncant Pelvic Floor Dysfunct 2011; 5: 120-1.
5. Pandya I, Shinojia M, Vadukul D, Marfatia YS, Approach to balanitis/balanoposthitis: Current guidelinesIndian J Sex Transm Dis 2014; 35: 155-7.
6. Verma SB, Wollina U, Looking through the cracks of diabetic candidial balanoposthitis!Int J Gen Med 2011; 4: 511-3.
7. Kalra S, Sharma A, Bharti Hospital, Karnal: Case ReportIndia Int J Clin Cases Invest 2010; 1: 46
8. Goldstraw MA, Kirby MG, Bhardwa J, Kirby RS, Diabetes and the urologist: A growing problemBJU Int 2007; 99: 513-17.
9. Drivsholm T, de Fine Olivarius N, Nielsen AB, Siersma V, Symptoms, signs and complications in newly diagnosed type 2 diabetic patients, and their relationship to glycemia, blood pressure and weightDiabetologia 2005; 48: 210-14.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.


Comments are closed.