Tuberous sclerosis associated with a renal angiomyolipoma
Patricia Chang1, Tyson Meaux2, Marisol Gramajo Rodas3
1Department of Dermatology, Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala, 2Student, Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala, 3Department of Pathology, Hospital General de Enfermedades IGSS and Hospital Ángeles, Guatemala
Sir,
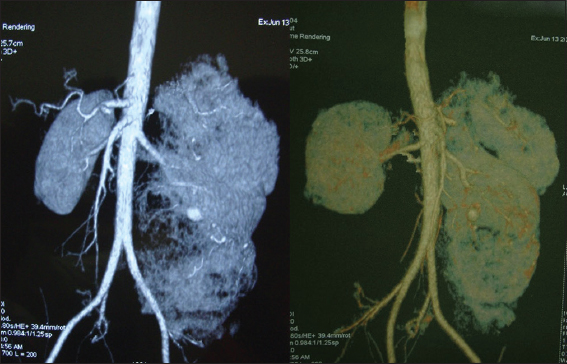
A 27 year-old male hospitalized in the department of urology awaiting left nephrectomy, after presenting with a four month history of feeling a mobile mass in his left abdomen. CT angiography of the bilateral kidneys showed the following: the right kidney is of normal dimensions with multiple lipomas no greater than 7mm, while the left kidney is enlarged, with multiple heterogeneous lipomas in the cortex and medulla, most likely representing an angiomyolipoma (Fig. 1).
Figure 1: CT angiography of the bilateral kidneys showed the following: the right kidney is of normal dimensions with multiple lipomas no greater than 7 mm, while the left kidney is enlarged, with multiple heterogeneous lipomas in the cortex and medulla, most likely representing an angiomyolipoma
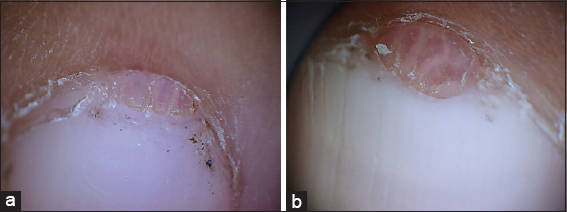
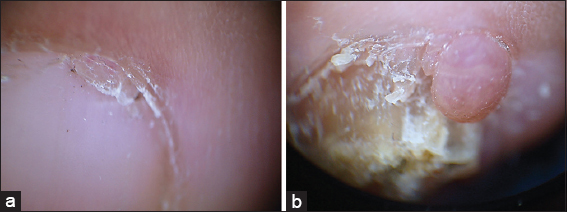
A through dermatologic examination demonstrated pink neoplasms in the proximal nail fold of the first, second, third and fourth toes of the left foot (Figs. 2 and 3), dermatoscopic view of the pink neoplasms of the proximal nail folds (Figs. 4ab and 5ab) and multiple, skin-colored neoplasms of the central face (Fig. 6). The remainder of the examination was within normal limits.
Figure 2: Pink neoplasms in the proximal nail fold of the first, second, third and fourth toes of the left foot
Figure 3: close up of the Koenen´s tumors of the proximal nail fold
Figure 4: (a and b) Dermatoscopic view of the neoplasms of the proximal nail fold
Figure 5: (a and b) Dermatoscopic view of the neoplasms of the proximal nail fold
Figure 6: Angiofibromas of the face
The patient reported that he has had the lesions on the face and left foot since he was very young. No other family member affected.
Past medical history and family history: negative and not consanguinity
With this clinical data, it was determined that the renal mass in this patient was associated with a diagnosis of tuberous sclerosis
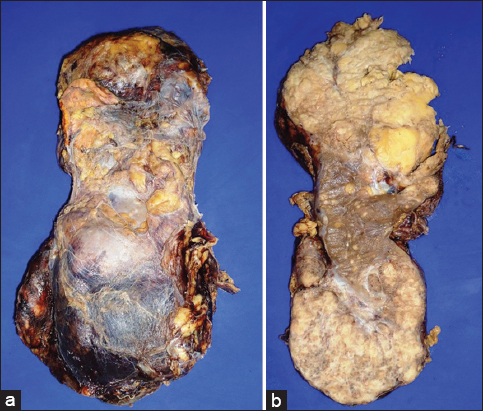
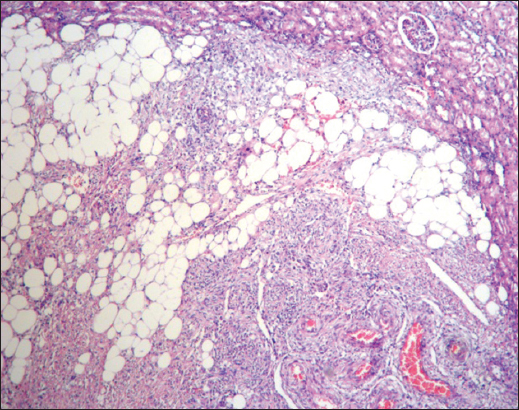
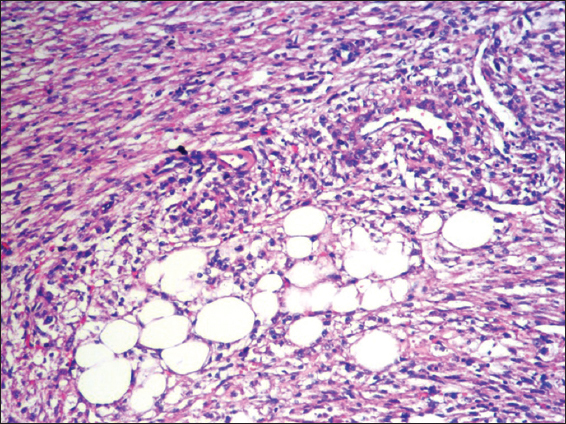
The renal mass was surgically removed. Macroscopic and histological images of the kidney are observed on its outer surface, note the increase in size and abnormal appearance (Fig. 7a) Cut surface of the macroscopic and histological images of the kidney are observed on its outer surface and at both poles, with some observable normal renal parenchyma (Fig. 7b), the microscopic image of the tumor shows that it is composed of neoplastic adipose tissue, smooth muscle and blood vessels, correlating well with the gross image (H & E 10X) (Fig. 8) Increased magnification of the neoplasm shows a group of adipocytes surrounded by prominent blood vessels and bundles of smooth muscle (H & E 40X) (Fig. 9).
Figure 7: (a) Macroscopic and histological images of the kidney are observed on its outer surface and increase in size and abnormal appearance (b) Macroscopic and histological images of the kidney are observed on its outer surface and at both poles, with some observable normal renal parenchyma
Figure 8: The microscopic image of the tumor shows that it is composed of neoplastic adipose tissue, smooth muscle and blood vessels, correlating well with the gross image (H & E 10X)
Figure 9: Increased magnification of the neoplasm shows a group of adipocytes surrounded by prominent blood vessels and bundles of smooth muscle, (H & E 40X)
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
What is interesting about this case is the association of tuberous sclerosis with a renal angiomyolipoma, which is not a very common clinical presentation.
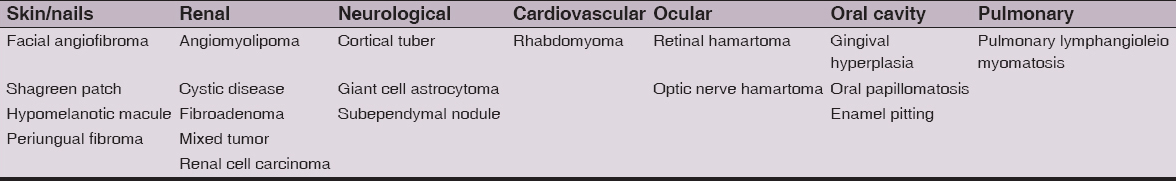
Tuberous sclerosis is an autosomal dominant genodermatosis, historically characterized by epilepsy, low intelligence, and hamartomatous lesions in many organs, including facial angiofibromas. Although reported as roughly 1 in 10,000, the exact prevalence of this disease is unknown, due to the fact that the classic triad mentioned above is only found in a minority of cases, making the diagnosis difficult [1]. Clinically, greater than 90 percent of affected patients have one or more classic skin finding, including facial angiofibromas, hypomelanotic macules, periungual fibromas, and Shagreen patches [2]. The percent of patients with tuberous sclerosis that present with the above-mentioned lesions are 90, 85, 50, and 40, respectively. Facial angiofibromas, or adenoma sebaceous, tend to first appear around four years of age, and are usually found symmetrically on the cheeks, nose, and forehead. They consist of 1-3 mm yellowish-red, discrete, waxy papules. Ash leaf, or hypomelanotic macules, may range in number from 1 to 100, commonly present in the first few decades of life, and tend to fade in late adulthood. “Knobby” patches or plaques of connective tissue, Shagreen Patches usually develop in the first decade of life. They vary in size from 1 to 8 cm in diameter, and are most found on the trunk, particularly the lumbosacral area. Periungual fibromas, also called Koenen tumors when associated with tuberous sclerosis, are small digitate, protruding neoplasms that tend to manifest during adolescence or adulthood, and despite their name, can be periungual and/or subungual (Table 1) [1,3]. In addition to cutaneous involvement, the kidneys are often affected in Tuberous Sclerosis. In one study, renal lesions were found in 80% of patients, with roughly 80% of those being angiomyolipomas (AML), 20% renal cysts, and 25 case reports of an associated renal cell carcinoma. It is a mutation in a tumor suppressor gene, either TSC1 or TSC2, which causes tuberous sclerosis. In general, both alleles of a tumor suppressor gene must be mutated to lead to disease, and hamartomas in tuberous sclerosis patients typically demonstrate this loss of heterozygosity. Interestingly, angiomyolipomas and renal cysts are more commonly associated with mutations in the TSC2 gene than the TSC1 gene. The diagnosis of tuberous sclerosis is usually suspected clinically, with confirmation by genetic testing. However, evidence of a mutation in TSC1 or TSC2 confirms the diagnosis even in the absence of physical findings. Biopsy is rarely needed, and is usually performed when the clinical picture is not classic for the disease [1,3,4]. When considering alternative diagnoses, the presence of multiple facial papules may indicate other genodermatoses, such as Cowden, Brook-Spiegle, or Birt-Hogg-Dubé syndrome [3]. Schaffer et. al describe a case of a patient with Birt-Hogg-Dubé syndrome, a rare autosomal dominant genodermatosis with an increased risk of renal tumors, whose major presenting sign was multiple facial angiofibromas [5]. Historically, surgery was considered to be the only viable option for treating the cutaneous lesions of tuberous sclerosis. More recently, topical rapamycin has been shown to improve the appearance of subungual fibromas and facial angiofibromas, lessening the need for surgery and subsequent scarring. In addition to topical treatment, systemic everolimus, approved for patients with tuberous sclerosis who have subependymal giant-cell astrocytomas or renal angiomyolipomas, has also proven to have positive effects on skin lesions [1,3,6,7].
Table 1: Different manifestations of the tuberous sclerosis
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from the patient for publication of this article.
REFERENCES
1. James WD, Berger TG, Elston DM, Genodermatoses and Congenital Anomalies in: Andrews’ Diseases of the Skin: Clinical DermatologySaunders Elsevier 2006; 542-3.
2. Zheng LQ, Huang Y, Han XC, Angiofibromas with multiple epidermoid cysts in tuberous sclerosis: new mutation or post-traumatic?J Cutan Pathol 2013; 40: 509-12.
3. Teng JMC, Cowen EW, Wataya-Kaneda M, Gosnell ES, Witman PM, Hebert AA, Dermatologic and Dental Aspects of the 2012 International Tuberous Sclerosis Complex Consensus StatementsJAMA Dermatol 2014; 150: 1095-101.
4. Rakowski SK, Winterkorn EB, Paul E, Steele DJ, Halpern EF, Thiele EA, Renal manifestations of tuberous sclerosis complex: Incidence, prognosis, and predictive factorsKidney Int 2006; 70: 1777-82.
5. Schaffer JV, Gohara MA, McNiff JM, Aasi SZ, Dvoretzky I, Multiple facial angiofibromas: A cutaneous manifestation of Birt-Hogg-Dubé syndromeJAAD 2005; 53: S108-S11.
6. Muzic JG, Kindle SA, Tollefson MM, Successful Treatment of Subungual Fibromas of Tuberous Sclerosis With Topical RapamycinJAMA Dermatol 2014; 150: 1024-5.
7. Romina M, Antonella C, Francesco G, Curatolo P, Is mTOR inhibition a systemic treatment for tuberous sclerosis?Ital J Pediatr 2013; 39: 57
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.