Infantile Haemangioma – An unusual location
Yugandar Inakanti1, Thimmasarthi Venkata Narsimha Rao2
1Department of Dermatology, Venerology and Leprosy, P.E.S. Medical College, Kuppam, India, 2Department of Dermatology, Venerology and Leprosy, Guntur Medical College, Guntur, India
ABSTRACT
Infantile haemangiomas (IH) are benign vascular neoplasms that have a characteristic clinical course marked by early proliferation and followed by spontaneous involution. Haemangiomas are the most common tumours of infancy and usually are medically insignificant. Cutaneous haemangiomas at particular sites is more common at Head and neck followed by Trunk and Extremities. Extra cutaneous haemangiomas were more common in Liver, Gastrointestinal tract, Larynx, Central nervous system, Pancreas and Lungs. We represent an 8-month-old boy presented with a small but growing, strawberry-colour tumour over the right groin since birth.
Key words: Cutaneous vasculature; Groin; Haemangiomas; Vascular malformations
INTRODUCTION
A “haemangioma”(Greek for blood-vessel-growth) of Infancy is a benign overgrowth of blood vessel cells in the skin. It is also known as proliferative haemangioma because it is due to proliferating endothelial cells; these are the cells that line blood vessels. The incidence ranges from 1% in neonates to 12% [1]. These are known to appear soon after birth, proliferate for 8-18 months, and then slowly regress over the next 5-8 years, leaving behind normal or slightly blemished skin [2,3].
Haemangiomas are common birthmarks which are usually red or purple. They mostly occur on the head and neck areas and develop shortly after birth. One in 10 babies will develop a haemangioma and it is more common in girls. In literature of Dermatology, groin has been cited unusual site of occurrence.
CASE REPORT
An 8-month-old boy presented with a small but growing, strawberry-colour tumor over the right side of the groin. The mass had been present since birth, now measuring approximately 4 × 3 cm of Circular in shape. The parents were concerned about the tumours growth and appearance.
The boy had been born prematurely at 34 weeks’ gestation after premature contractions and prolonged rupture of membranes. No maternal fever, tachycardia, chorioamnionitis, or other complications had occurred. The boy had stayed in neonatal intensive care for 4 weeks because of feeding issues, and he had been transiently on nasal continuous positive airway pressure therapy, from which he was weaned to room air after 3 days of life. He was discharged at 38 weeks’ gestation. When the child had reached approximately 6 months of age, he had begun to scratch the haemangioma and rub it against toys and other items, resulting in severe ulceration of the lesion. The parents were anxious about the tumour’s rapid growth, and bleeding from minor trauma.
On admission, a thorough physical examination showed tumours growth of oval to circular in shape with diameter of 4 × 3 cm with red in colour over the right side of groin (Figs 1 and 2). Single linear ulcer with well defined borders of size 1cm was seen over tumourous growth. No other areas of body affected.
Figure 1: Multiple tumorous growth over right side of groin
Figure 2: Linear ulcer with well-defined border over tumorous growth.
The possible differential diagnoses are
- Cherry Haemangioma
- Cobb Syndrome
- Lipomas
- Capillary Malformation
- Lymphangiomas
- Lobular Capillary Haemangioma)
Routine Laboratory investigations followed by electrocardiogram, chest x-ray and local ultrasonography of the lesion using a high frequency probe. Laboratory investigations were within normal limits.
After discussing with parents and with their consent, Punch biopsy was performed.
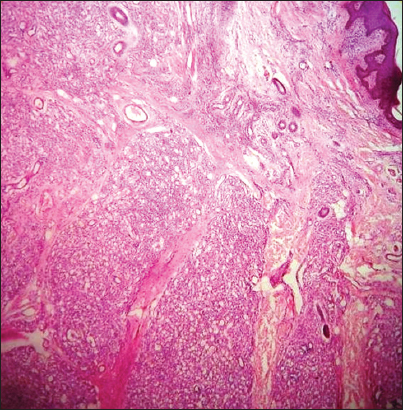
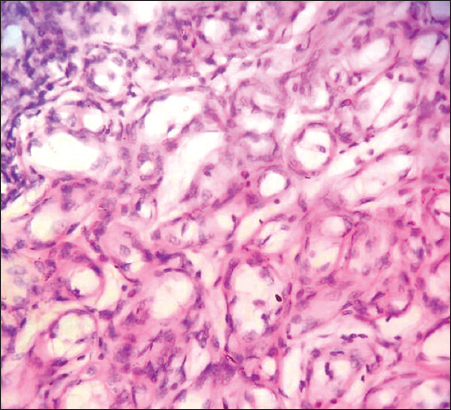
Histopathological examination of the specimen showed the Para keratinised stratified Squamous epithelium of varying thickness and the fibrous connective tissue with numerous endothelial lined capillaries of varied size and few blood vessels, which were yet to be lumenized (Figs 3–5). Tumour of the blood vessels of capillary calibre (no elastic fibres nor smooth muscle within the wall, size is variable) and undifferentiated endothelia. Diagnosis of capillary haemangioma was confirmed.
Figure 3: Para keratinised stratified Squamous epithelium of varying thickness and the fibrous connective tissue with numerous endothelial lined capillaries of varied size.
Figure 4: Fibrous tissue in between capillaries.
Figure 5: Endothelial cells lining capillaries.
After evaluating the boy and noting the haemangioma location and because of parent’s anxiety and apprehension the boy was referred to paediatric surgery.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
IH is a benign, self-involuting tumour of endothelial cells that usually appears during the first weeks to months of life [4]. It is one of the most common birthmarks among newborns. Most infantile haemangiomas reach a maximum size of 0.5-5 cm, but they can range from the size of a pinhead to greater than 20cm in diameter. Most infantile haemangiomas remain well circumscribed and focal. Haemangiomas are found in up to 10% of children by the age of 1 year and are more common in girls and premature infants. Their cause is unknown. In very rare instances, they may run in families, but they generally are not inherited.
Infantile haemangiomas are classified as superficial, deep or mixed lesions.
- The superficial infantile haemangiomas is also called capillary haemangioma, capillary naevus, strawberry haemangioma, strawberry naevus, and haemangioma simplex. The blood vessels in uppermost layers of the skin are dilated.
- Deep infantile haemangiomas are also called cavernous haemangiomas and are more deeply set in the dermis and sub cutis. They appear as a bluish soft to firm swelling.
- Both types of haemangiomas may occur together in mixed angiomatous naevi. A strawberry naevus overlies a bluish swelling.
Another variant is the infantile haemangioma with minimal or arrested growth (IH-MAG). These have been previously referred to as abortive, reticular, or telangiectatic IH. This variant has been seen in association with underlying vascular and other extracutaneous congenital anomalies PHACE and PELVIS syndromes [5].
Regulators of haemangioma growth and involution are poorly understood. During the growth phase, two major proangiogenic factors are involved: basic fibroblast growth factor (bFGF) and vascular endothelial growth factor (VEGF) [6]. Potential explanations for the therapeutic effect of propranolol (a non-selective beta-blocker) on IH include: vasoconstriction, which is immediately visible as a change in colour, associated with a palpable softening of the haemangioma; decreased expression of VEGF and bFGF genes through the down regulation of the RAF-mitogen -activated protein kinase pathway [7]. The response of IH to propanolol has been reported by Léauté-Labrèze et al [8].
IH usually involutes over time: 30% resolve by 3 years of age, 50% by 5 years of age, and 80% to 90% by 9 years of age. More than half of haemangiomas heal with excellent cosmetic results without treatment. Nevertheless, some haemangiomas require treatment, such as when a vital organ (e.g. eye, ear, trachea) is involved; when bleeding, ulceration, crusting, or infection is present; or when their rapid growth leads to deformity of surrounding tissues. IH in certain areas, particularly the face (especially the nose and lips), body folds, and groin, have a higher risk of complications.
The vast majority of IH do not require any medical or surgical intervention. Medical care of clinically significant IH has been limited to a few medications, including glucocorticosteroids (topical, intralesional and oral), interferon alfa [9] and, rarely, vincristine and topical Imiquimod [10]. Beta-blockers, most specifically propanolol, [11] have serendipitously been shown to induce involution of IH [8,12] Pulse dyed laser surgery, [13] other lasers frequency-doubled ND: YAG, and KTP lasers.
Certain benefits to early surgical excision include saving a life or preserving vision if it is near to eye and decreasing the negative psychosocial effects associated with a cosmetically disfiguring lesion during early childhood.
CONCLUSION
To our best of knowledge, this is the first reported case of a capillary haemangioma occurring in this location. We describe case of capillary haemangiomas, concluding that despite the rarity of these lesions, they should be considered in the differential diagnosis of lesions in the groin region.
CONSENT
Written informed consent was obtained from the patient guardian for publication of this case report and any accompanying images. The examination of patients is conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Sharma N, Panda SS, Singh A, Bajpai M, Use of oral prednisolone with or without propranolol in the management of infantile hemangioma: A critical appraisalIndian J Paediatric Dermatol 2013; 14: 19-22.
2. Mishra MB, Bishen KA, Yadav A, Capillary hemangioma: An occasional growth of attached gingivaJ Indian Soc Periodontol 2012; 16: 592-6.
3. Jadhav VM, Tolat SN, Dramatic response of propranolol in hemangioma: Report of two casesIndian J Dermatol Venereol Leprol 2010; 76: 691-4.
4. Sachdeva M, Kaur S, Nagpal M, Dewan SP, Cutaneous lesions in new bornIndian J Dermatol Venereol Leprol 2002; 68: 334-7.
5. Suh KY, Frieden IJ, Infantile hemangiomas with minimal or arrested growth: a retrospective case seriesArch Dermatol 2010; 146: 971-6.
6. Frieden IJ, Haggstrom AN, Drolet BA, Mancini AJ, Friedlander SF, Boon L, Infantile hemangiomas: current knowledge, future directions: Proceedings of a research workshop on infantile hemangiomas, April 7-9, 2005Pediatr Dermatol 2005; 22: Maryland, USA: Bethesda; 383-6.
7. Sulpice E, Bryckaert M, Lacour J, Contreres JO, Gerard Tobelem, Platelet factor 4 inhibits FGF2-induced endothelial cell proliferation via the extracellular signal–regulated kinase pathway but not by the phosphatidylinositol 3–kinase pathwayBlood 2002; 100: 3087-94.
8. Léauté-Labrèze C, Dumas de la Roque E, Hubiche T, Boralevi F, Thambo JB, Taïeb A, Propranolol for severe hemangiomas of infancyN Engl J Med 2008; 358: 2649-51.
9. Musumeci ML, Schlecht K, Perrotta R, Schwartz RA, Management of Cutaneous Hemangiomas in Pediatric PatientsCutis 2008; 81: 315-2.
10. Akinbami BO, Omitola OG, Akadiri OA, Pattern of presentation and management of orofacial and neck soft tissue tumors in a Nigerian tertiary health center – a preliminary studyIntern Med Inside 2013; 1: 9
11. Price CJ, Lattouf C, Baum B, McLeod M, Schachner LA, Duarte AM, Propranolol vs Corticosteroids for Infantile Hemangiomas: A Multicenter Retrospective AnalysisArch. Dermatol 2011; 147: 1371-6.
12. Siegfried EC, Keenan WJ, Al-Jureidini S, More on propranolol for hemangiomas of infancyN Engl J Med 2008; 359: 2846-7.
13. Srinivas C R, Kumaresan M, Lasers for vascular lesions: Standard guidelines of careIndian J Dermatol Venereol Leprol 2011; 77: 349-68.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.