O’Brien’s Granuloma in a 50-year-old Chinese male
Loai Sami, Huang Changzheng
Department of Dermatology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
ABSTRACT
O’Brien’s actinic granuloma is clinically characterized by grouped red papules that may coalesce into annular plaques on sun damaged skin such as the head and neck, chest, and arms. There is no gender predilection, and patients tend to be middle-aged or older giving the association with significant actinic damage. We presented a 50-year-old male with multiple annular lesions on the neck of four years duration, associated with prolonged sun exposure. A biopsy confirmed the clinical suspicion of O’Brien’s granuloma and excluded other possibilities.
Key words: O’Brien’s; granuloma; actinic
INTRODUCTION
O’Brien’s granuloma is a rare skin disease that presents clinically by grouped red papules that may coalesce into annular plaques on sun damaged skin. The annular plaques have raised erythematous borders (3-5 mm)and slightly atrophic center [1]. The hypo pigmented central regions are distributed mainly in sun-exposed areas. The sites of predilection include the neck, face, chest and arms. Early on, skin-colored or pink papules may be identified singly or in small groups before they coalesce into annular plaques. Individual lesions measure 1-10 cm in diameter. A single plaque lasts for months to years, after which spontaneous remission may occur, leaving mottled dyspigmentation or normal-appearing skin [2].
O’Brien’s granuloma must however, be differentiated from granuloma annulare which is a distinct entity. Lesions of granuloma annulare occur most commonly on the dorsa of the hands and feet. Interestingly, a variant of granuloma annulare has been described in which the lesions occur on the sun-exposed areas [3].
CASE REPORT
A 50-year-old male presented with multiple annular lesions on the neck of four years duration, associated with prolonged sun exposure.
Since four years ago, the patient started to develop small erythematous papules on the back of the neck, which increased in size and healed centrally to form many annular lesions on the back and the sides of the neck, at sun exposure area.
Exposure to the sun followed by erythema and mild itching but no pain.
The patient was otherwise healthy. He had no past history of skin diseases or medical diseases, no family history of skin or medical diseases. Drug history was negative. No application of any topical agents was found. The patient exposed to the sun several hours daily for many years.
Physical examination showed pink papules arranged into annular form with slightly atrophic center. There were several rings on the back and sides of the neck ranging between one to five centimeters in diameter. The surface of the lesions was smooth, shiny and firm (Figs 1-a, b and c).
Figure 1: The clinical pictures of O’Brien’s granuloma: Fig.1a and 1b: small erythematous papules on the back of the neck, which increased in size and healed centrally to form many annular lesions. There were several rings on the back and side of the neck ranging between one to five centimeters in diameter on the back and the side of the neck. Fig.1c: Close up view revealed significant pink papules arranging into annular form with slightly atrophic center. The surface of the lesions was smooth, shiny and firm.
A full blood count, ESR, routine biochemistry and urinalysis were normal. Angiotensin converting enzyme levels were within normal limits and antinuclear antibodies were negative. The intradermal tuberculin test was nonreactive. A chest X-ray did not reveal any abnormalities.
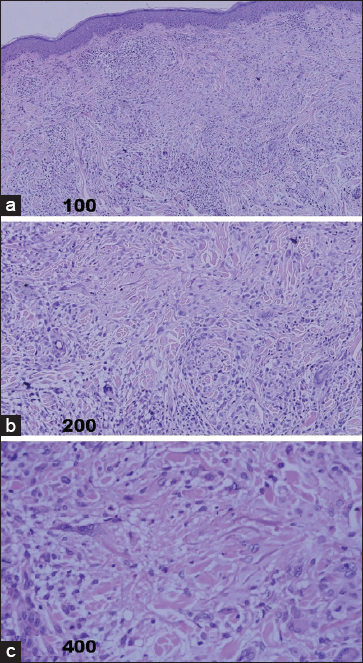
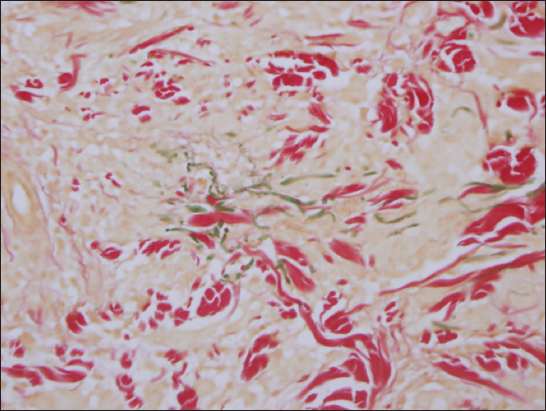
Biopsy of a plaque on the neck showed histological changes consistent with the diagnosis of O’Brien’s granuloma. In the dermis, there were granulomas composed of histiocytes and a few multinucleated giant cells which arranged with no typical palisading pattern in the periphery as seen in granuloma annulare. Occasionally mild collagen degeneration in the center of the granuloma could be seen (Figs 2-a, b and c). Alcian blue staining showed no significant mucin deposition in the center of granuloma (Fig. 3). Decreased and broken fragments of elastic fibers could be found in the center of granuloma. However, Elastophagocytosis was not seen (Fig 4).
Figure 2: (HE stain)In dermis, there were granulomas composed of histiocytes and a few multinucleated giant cells, (Fig.2a×100). The histiocytes and multinucleated giant cells showed no typical palisading pattern in the periphery of the granuloma. Rarely, mild collagen degeneration could be found in the center of the granuloma, (Fig.2b×200; Fig.2c×400).
Figure 3: (Alcian blue staining)showed no mucin deposition in the center of granuloma.
Figure 4: (Masson stain): there were a few broken fragments of elastic fibers in the center of granuloma.
Based on the history especially the lesions are associated with sun light and the special location, a diagnosis of actinic granuloma was established.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure.
DISCUSSION
O’Brien granuloma is a rare disorder develop in an area of solar elastosis [4]. O’Brien used‘actinic’ in the name of this disorder because he believed that its etiology was linked to ultraviolet and infrared radiation. This theory was rejected by Hanke et al [5], whose patients did not all demonstrate significant solar elastosis histologically but otherwise fit O’Brien’s clinical and histopathologic descriptions. These authors coined the descriptive term annular elastolytic giant cell granuloma in 1979. Upon review of the literature, both O’Brien and Hanke realized that the diseases they were describing had previously been reported under other names, including atypical necrobiosis lipoidica of the face and scalp [6],
O’Brien’s granuloma is an annular inflammatory reaction with giant cell dermal infiltrate, which is characterized clinically by lesions develop in the exposed skin [7]. They start insidiously as small, pink papules, which progress slowly to form an annular, firm, superficial, smooth dermal thickening, the ring may expand up to 6 cm in diameter with slightly atrophic center, usually asymptomatic [4].
The pathology shows three distinct zones in the dermis. In the external ‘normal’ skin, there is actinic elastosis. In the thickened edges, there is a histiocytic and giant cell inflammatory reaction in relation to elastotic fibers, and in the center, within the annulus, little or no elastic tissue remains [8]. The cellular infiltrate slowly expands outwards, leaving behind a central area from which elastic fibers have been removed by ‘elastoclasis’. The epidermis may be normal or it may show signs of actinic damage [9–11].
O’Brien’s granuloma must, however, be differentiated from granuloma annulare which is a distinct entity. Lesions of granuloma annulare occur most commonly on the dorsa of the hands and feet. Interestingly, a variant of granuloma annulare has been described in which the lesions occur on the sun-exposed areas [2].
However, granuloma annulare is characterized by foci of necrobiotic collagen surrounded by palisades of histiocytes which are not features of actinic granuloma. In further contrast with lesions of actinic granuloma, elastosis and elastoclastic giant cells are absent and mucin deposition is usually more obvious from granuloma annulare [12].
Annular elastolytic giant cell granuloma was characterized clinically by erythematous papules and plaques which may arise anywhere on the body, but the diagnosis is usually reserved for those that occur on areas without severe actinic damage. They may often be annular in appearance. Most patients are over 40 years old, and children are almost never affected. Histologically there are dermal granulomas with prominent multinucleated giant cells. Elastophagocytosis is a common feature. Necrobiosis and mucin deposition are absent, and there should not be a significant degree of palisading. As the lesions progress, more elastic fibers are destroyed eventually leading to a complete absence of elastic fibers in affected areas. An elastin stain will highlight the elastic fibers and help identify elastophagocytosis [1].
O’Brien argued that actinic granuloma to Miescher’s granuloma of the face, atypical necrobiosis lipoidica of the face and scalp, and granuloma multiforme were, in fact, the same, although distinct from granuloma annulare. He speculated that they resulted from a common sequence of events in which primary elastin damage was followed by a giant-cell-mediated phagocytic repair process. It is generally accepted, however, that at least some of the conditions do represent true variants in the well-recognized necrobiosis lipoidica-granuloma annulare spectrum of granulomatous reactions. Specific disease entities might result from different types of dermal injury, with some degree of overlap [13].
Granuloma multiforme is a chronic granulomatous skin condition, characterized clinically by firm papules aggregated into plaques or forming the edges of annular lesions mainly occurring in middle Africa, and histologically by focal areas of necrobiosis, with loss of elastic tissue, surrounded by histiocytes. Multinucleated giant cells are usually a prominent feature. There is a perivascular lymphocytic infiltrate with variable numbers of plasma cells and eosinophils [14,15].
CONCLUSION
We presented a 50-year-old male with O’Brien’s actinic granuloma, who present clinically as multiple annular lesions on the neck of four years duration, associated with prolonged sun exposure. Our patient was compatible with the aforementioned clinical and histopathologically features of O’Brien’s granuloma and excluded other possibilities. This is further supported by the fact that the condition is more common in sunny countries and in fair-skinned and actinically damaged individuals.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Hawryluk EB, Izikson L, English JC, 3rdNon-infectious granulomatous diseases of the skin and their associated systemic diseases: an evidence-based update to important clinical questionsAm J Clin Dermatol 2010; 11: 171-81.
2. Leppard B, Black MM, Disseminated granuloma annulareTrans St Johns Hosp Dermatol Soc 1972; 58: 186-90.
3. O’Brien JP, Actinic granuloma ±An annular connective tissue disorder affecting sun and heat damaged (elastotic)skinArch Dermatol 1975; 11: 460-6.
4. Lazzarini R, Rotter A, Farias DC, Muller H, O’Brien’s actinic granuloma: an unusually extensive presentationAn Bras Dermatol 201: 86339-42.
5. Hanke CW, Bailin PL, Roenigk HM, Annular elastolytic giant cell granulomaJ Am Acad Dermatol 1979; 1: 413-21.
6. Stain JA, Fangman B, Strober B, Actinic granulomaDermatol Online J 2007; 13: 19
7. Delgado-Jimenez Y, Perez-Gala S, Peñas PF, Fraga J, Garcia-Diez A, Fernandez-Herrera J, O’Brien actinic granuloma presenting as alopeciaJ Eur Acad Dermatol Venereol 2006; 20: 226-7.
8. Gartmann H, Groth W, Kuhn A, Elastofibroma dorsiZ Hautkr 1988; 63: 525-8.
9. Yamazaki K, An ultrastructural and immunohistochemical study of elastofibroma: CD 34, MEF-2, pronine 2 (CD33), and factor XIIIa- positive proliferating fibroblastic stromal cells connected by Cx43-type gap junctionsUltrastruct Pathol 2007; 31: 209-19.
10. Mortman KD, Hochheiser GM, Giblin EM, Manon-Matos Y, Frankel KM, Elastofibroma dorsi: clinicopathologic review of 6 casesAnn Thorac Surg 2007; 83: 1894-7.
11. Lazzarini R, Rotter A, Farias DC, Muller H, O’Brien’s actinic granuloma: an unusually extensive presentationAn Bras Dermatol 2011; 86: 339-2.
12. Agarwal S, Takwale A, Bajallan N, Berth-Jones J, Charles-Holmes S, Co-existing actinic granuloma and giant molluscum contagiosumClin Exp Dermatol 2000; 25: 401-3.
13. Ratnavel RC, Grant JW, Handfield-Jones SE, Norris PG, O’Brien’s actinic granuloma: response to isotretinoinJ R Soc Med 1995; 88: 528-9.
14. Garrett AS, Granuloma multiforme (called Nkanu disease in the 1940s and Mkardisease in 1964)Int J Lepr Other Mycobact Dis 1999; 67: 172-4.
15. Sandhu K, Saraswat A, Gupta S, Shukla R, Handa S, Granuloma multiformeInt J Dermatol 2004; 43: 441-3.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.


Comments are closed.