Pruritus in hemodialysis patients: Results from Fresenius dyalisis center, Banja Luka, Bosnia and Herzegovina
Zoran Vrucinic1, Biljana Jakovljevic2, Ljubisa Preradovic3
1Department of Dermatology, University Hospital Clinical Center, Banja Luka, Bosnia and Herzegovina, 2Fresenius Medical Care Dialysis Center, Banja Luka, Bosnia and Herzegovina, 3Faculty of Architecture, Civil Engineering and Geodesy, University of Banja Luka, Bosnia and Herzegovina
ABSTRACT
Introduction: Uremic pruritus (UP) is a common and distressing complication of end-stage renal disease (ESRD). A global cross-sectional study of 18,000 hemodialysis patients reported a 42% prevalence of moderate or extreme UP, which was strongly associated with sleep disturbance, depression, impaired quality of life, and mortality. Pruritus is commonly encountered in individuals with end-stage renal disease (ESRD) on hemodialysis (HD).
Material and Methods: This cross-sectional study was performed in order to find out the prevalence of pruritus in patients on regular maintenance hemodialysis (HD) as well as to analyze its relationship to age, sex of the patient, duration of hemodialysis in months per patient, serum levels of phosphate, PTH, KT/V (index of dialysis dose), parameters in the beggining of the study and six months after. The data were analyzed by descriptive statistics-Wilcoxon Signed Rank Test and Chi-square test with Yates correction factor.
Results: Sixty and two patients with ESRD (age ranging from 31 to 87 years) free from systemic, skin or psychiatric disorders and other secondary causes attributable to pruritis, undergoing maintenance HD (duration on HD 4-348 months; mean 86.97 and median 79,5 months) at Fresenius dialysis center, Banja Luka, Bosnia and Herzegovina were evaluated for pruritus. Pruritus has been discovered in 21 out of 34 males (54,8%) and 6 out of 28 females (22,2%). Our study as many others showed that pruritus is very common (45.2%) in HD patients. Applying χ2 test with Yates correction factor is highly statistically significant (χ2 = 8.003, p = 0.005) by gender. Research of the gender revealed that pruritus appeared more in men analysis. There were no significant differences between other measured markers: to age, duration of hemodialysis in months per patient, serum levels of phosphate, PTH, KT/V (index of dialysis dose) in patients with pruritus and in patients without pruritus.
Conclusions: This first cross-sectional study describes key features UP in Republic of Srpska (Bosnia and Herzegovina) and results that the UP is significantly more common in men. This study demonstrates that the serum level of PTH and phosphate isn’t associated with the incidence of pruritus in HD patients.
Key words: Uremic pruritus; End-stage renal disease; Hemodialysis
INTRODUCTION
Pruritus, defined as an unrestricted and uncomfortable sensation that elicits the desire to scratch, has been well recognized as a common complication in patients with chronic Renal failure [2–6]. It has been found that 15%-49% of patients with predialysis chronic renal failure and 50%-90% of those on hemodialysis or CAPD have pruritus [7].
In 2012, over 2500 patients received hemodialysis (HD) in the Bosnia and Herzegowina [17], in USA about 384,000 [7], and in Germany about 63,300 patients per year depend on HD [8]. It is estimated that worldwide more than 2 million people suffer from end-stage renal disease (ESRD) that requires HD.
Pruritus may be localized or disseminated and is the most common symptom of ESRD. It occurs in about 53% of these patients, causing great harm to their quality of life [2,10,11]. It is not associated with other primary or systemic skin diseases, psychological disorders or acute renal failure. The pathogenesis is not fully known, but there is a relation with hyperparathyroidism, xerosis, hypervitaminosis A, iron deficiency anemia, and elevated serum levels of magnesium, calcium, phosphate, aluminum and histamine, though the latter may be associated with allergic sensitization to components in dialysis membranes. Pruritus contributes to the appearance of perforating injuries by the Koebner phenomenon [12–16].
Moreover, there is no relationship between the plasma level of PTH and dermal Cell proliferation, nor is there a difference in the number of mast cells or the levels of PTH between patients with or without pruritus.
The pathophysiology of pruritus is multifactorial. Until now, studies reported significant association between serum parathyroid hormone (PTH) and the itching; some other studies have found no specific relationship between pruritus and hyperparathyroidism, hypercalcemia, hyperphosphatemia, and level of PTH [5,9,14,23].
PATIENTS AND METHODS
This cross-sectional study was conducted on sixty and two patients with ESRD (age ranging from 31 to 87 years) free from systemic, skin or psychiatric disorders and other secondary causes attributable to pruritis, undergoing maintenance HD at Fresenius dialysis center, Banja Luka, Bosnia and Herzegovina were evaluated for pruritus and included in a study during period from December, 2013 to May, 2014. Duration of each session was 4 hours.
Those with history of dermatologic disease or chemical exposure were excluded. Patients were asked to report the severity of their pruritus.
Blood samples were taken from all patients for assessment of serum levels of phosphate, PTH, KT/V (index of dialysis dose), parameters at the beginning of the study and six months after.
Ethics
This study was performed on human subjects; thus, all patients were aware of the presence of the study and they were fully informed about the drug and its side-effects.
Statistical Analyses
Descriptive data were compared as a mean±standard deviation (range). Mann-Whitney U test and T-test was used to compare means between patients with and without pruritus.
Wilcoxon Signed Rank Test and Chi-square test with Yates correction factor were used for relationship of quantitative data and comparison of qualitative variables respectively. The level of significance was p<0.05.
RESULTS
The overall prevalence of pruritus in the present study is 45,2%.
Pruritus has been discovered in 21 out of 34 males (54,8%) and 6 out of 28 females (22,2%).
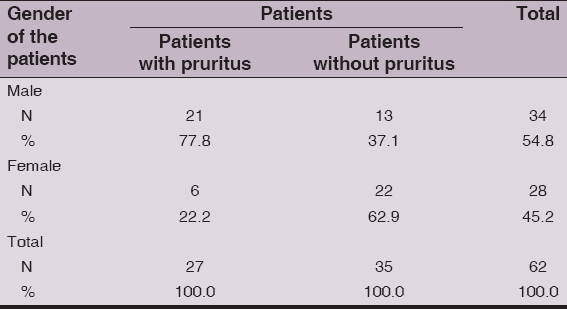
Applying χ2 test with Yates correction was highly statistically significant (χ2 = 8.003, p = 0.005) by gender. Analysis of the gender revealed that pruritus was significantly more detected in men, as shown in Table 1.
Table 1: Pruritus in relation to patients’ gender
According to patients’ age no significant differences were found (applying T-Test (Independent Samples), t = – 0.443, p = 0.659).
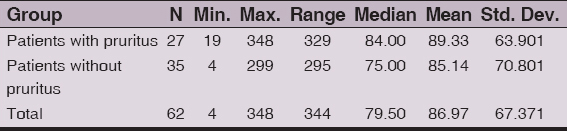
Applying the Mann-Whitney-U test, there was no statistically significant difference in the duration HD/months/by groups of patients with pruritus (n = 27, Md = 84.00) and those without pruritus (n = 35, Md = 75.00), U = 421.00 z = -0731, p = 0.465, r = 0.092 (Table 2).
Table 2: HD duration (months)
Using the Mann-Whitney-U test, there was no statistically significant difference in KTV1 by groups of patients with pruritus (n = 27, Md = 1.56) and patients without pruritus (n = 35, Md = 1.65), U = 339.50, z = -1889, p = 0.059, r = 0.239), the laboratory determined the start of the study as shown in Table. 3.
Table 3: Comparison of values KT/V 1 (index of dialysis dose)
Using the T-test for independent samples there was no statistically significant difference (t = – 1.166, p = 0.248) in KT/V2 examined groups of subjects, measured at the end of the study.
Using the Mann-Whitney-U test, there was no statistically significant difference of level Phosphate 1 in serum by groups of patients with pruritus (N = 27, Md = 1.42) and patients without pruritus (N = 35, Md = 1.33), U = 371.50, z = -1.434, p = 0.151, r = 0.182. The laboratory determined the start of the study as shown in Table 4.
Table 4: Comparison of Phosphate 1 level in serum
Using the Mann-Whitney-U, test there was no statistically significant difference of level Phosphate 1 in serum by groups of patients with pruritus (N = 27, Md = 1.26) and patients without pruritus (N = 35, Md = 1.30), U = 456.50, z = -0.227, p = 0.820, r = 0.029, measured at the end of the study.
Using the Mann-Whitney-U test, there was no statistically significant difference in PTH 1 by groups of patients with pruritus (N = 27, Md = 194.50) and patients without pruritus (N = 35, Md = 245.80), U = 453.00, z = -0.277, p = 0.782, r = 0.035 as shown in Table 5.
Table 5: Comparison of PTH 1 level in serum
Using the Mann-Whitney-U test, there was no statistically significant difference in PTH 2 by groups of patients with pruritus (N = 27, Md = 218.20) and patients without pruritus (N = 35, Md = 214.70), U = 455.00, z = -0.248, p = 0.804, r = 0.031.
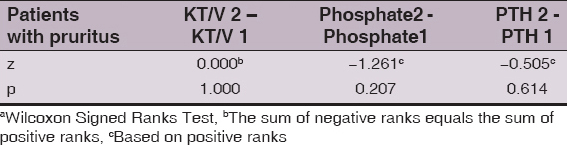
By applying the Wilcoxon test of paired couples there was no statistically significant difference in patients with pruritus neither in the change of KT/V2 and KT/V1 (z = 0.000, p = 1.000), nor in the change of Phosphates2 and Phosphates (z = -1.261, p = 0.207) nor in the change of PTH2 and PTH2 (z = -0,505, p = 0.614)., that is the measured laboratory value at the beginning of the study as shown in Table 6.
Table 6: Comparisons within groups
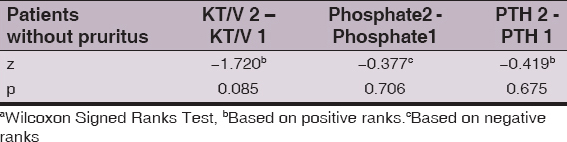
By applying the Wilcoxon test of paired couples there was no statistically significant difference in patients without pruritus neither in the change of KT/V2 and KT/V1 (z = -1.720, p = 0.085), nor in the change of Phosphates2 and Phosphates ((z = -0.377, p = 0.706), nor in the change of PTH2 and PTH2 (z = -0.419, p = 0.675). measured at the end of the study as shown in Table 7.
Table 7: Comparisons within groups
DISCUSSION
We conducted the first study of uremic pruritus in Republic of Srpska (Bosnia and Herzegovina).
Our study as many others showed that pruritus is very common (45.2%) in HD patients.
The overall prevalence of pruritus among our study population is 45,2 % and it is comparable with the published reports [1,3–5,14,17–19,20–22,24].
Pruritus has been detected in 21 out of 34 males (54,8%) and 6 out of 28 females (22,2%).
Analysis of the gender revealed that pruritus was significantly more shown in men, and previous studies have shown no difference in gender [24].
Men in the DOPPS I and I Studies had UP more often than women. In contrast, Snit M. et al. report that UP occurred statistically significantly more often in women, independent of method of renal replacement therapy [1,14].
In our study, we did not find any relationship between pruritus and duration of dialysis as seen in some previous studies [14,21,23,24].
Like most of other studies, we could not find any relationship between serum levels of phosphorus and UP in the patients’ [24].
Hyperparathyroidism has been proposed by some authors as a cause of uremic pruritus [24]. Hyperparathyroidism can stimulate mast cells to release histamine and can promote microprecipitation of calcium and magnesium salts in the skin. On the other hand, all of the patients with severe hyperparathyroidism do not have pruritus. Moreover, there is no relationship between the plasma level of PTH and proliferation of dermal cell, and there is no difference in the number of mast cells and the levels of PTH between patients with or without pruritus. On the other hand, a direct role for parathyroid hormone as a cause of uremic pruritus has been questioned because of the failure of intradermal injections of PTH analogs to produce pruritus, and because of negative immunohistochemical studies for PTH in the skin biopsy specimens [24].
Furthermore, no correlation between PTH levels and itching intensity was found in most studies [14,21,23].
In our study, we did not find any relationship between pruritus and the plasma level of PTH.
CONCLUSIONS
This first cross-sectional study describes key features UP in Republic of Srpska and results that the UP is significantly more common in men.
This study demonstrates that the serum level of PTH and phosphate isn’t associated with the incidence of pruritus in HD patients.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
REFERENCES
1. Pisoni RL, Wikstrom B, Elder SJ, Akizawa T, Asano Y, Keen ML, Pruritus in haemodialysis patients. International results from the Dialysis Outcomes and Practice Patterns Study (DOPPS)Nephrol Dial Transplant 2006; 21: 3495-05.
2. Lupi O, Rezende L, Zangrando M, Sessim M, Silveira CB, Sepulcri MAS, Cutaneous manifestations in end-stage renal diseaseAn Bras Dermatol 2011; 86: 319-26.
3. Suseł J., Batycka-Baran A, Reich A, Szepietowski JC, Uraemic Pruritus Markedly Affects the Quality of Life and Depressive, Symptoms in Haemodialysis Patients with End-stage Renal DiseaseActa Derm Venereol 2014; 94: 276-81.
4. Falodun O, Ogunbiyi A, Salako B, George AK, Skin Changes in Patients with Chronic Renal FailureSaudi J Kidney Dis Transpl 2011; 22: 268-72.
5. Mathur VS, Lindberg J, Germain M, Block G, Tumlin J, Smith J, Longitudinal Study of Uremic Pruritus in Hemodialysis PatientsClin J Am Soc Nephrol 2010; 5: 1410-19.
6. Weiss M, Weisshaar E, Qualitative Interviews on Chronic Pruritus in Haemodialysis PatientsActa Derm Venereol 2014; 94: 713-4.
7. U.S. Renal Data System, USRDS 2011 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage RenalDisease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD2013; Available from: URL: http://www.usrds.org/atlas11.aspx.
8. Frei U, Schober-Halstenberg H, Nierenersatztherapie in Deutschland. Bericht über Dialysebehandlung und Nierentransplantation in DeutschlandAnnual report QuaSi-Niereg GmbH 2004/2005; 17:
9. Sprague SM, Moe SM, The Case for Routine Parathyroid Hormone MonitoringClin J Am Soc Nephrol 2013; 8: 313-8.
10. Kuypers DR, Skin problems in chronic kidney diseaseNat Clin Pract Nephrol 2009; 5: 157-70.
11. Pisoni RL, Wilkström B, Elder SJ, Akizawa T, Asano Y, Keen ML, Pruritus in haemodialysis patients: International results from the Dialysis Outcome and Practice Patterns Study (DOPPS)Nephrol Dial Transplant 2006; 21: 3495-505.
12. Udayakumar P, Balasubramanian S, Ramalingam KS, Lakshmi C, Srinivas CR, Mathew AC, Cutaneous manifestations in patients with chronic renal failure on hemodialysisIndian J Dermatol Venereol Leprol 2006; 72: 119-25.
13. Welter EQ, Bonfá R, Petry V, Moreira LL, Weber MB, Relação entre grau de prurido e qualidade de vida de pacientes em hemodiáliseAn Bras Dermatol 2008; 83: 137-40.
14. Śnit M, Gawlik R, Łącka-Gaździk B, Kuźniewicz R, Dwornicki M, Owczarek A, Substance P and pruritus in dialyzed patientsMed Sci Monit 2013; 19: 723-32.
15. Chen HY, Chiu YL, Hsu SP, Pai MF, Lai CF, Yang JY, Elevated C-reactive protein level in hemodialysis patients with moderate/severe uremic pruritus: a potential mediator of high overall mortalityQJM 2010; 103: 837-46.
16. Laudański K, Nowak Z, Niemczyk S, Age-related differences in the quality of life in end-stage renal disease in patients enrolled in haemodialysis or continuous peritoneal dialysisMed Sci Monit 2013; 19: 378-85.
17. Resić H, Prnjavorac B, Nadomještanje bubrežne funkcije u Bosni i Hercegovini u 2013. godini. Udruženje ljekara za nefrologiju, dijalizu i transplantaciju bubrega u Bosni i HercegoviniAvailable from: URL: http://www.undt.ba/download/Godisnji%20izvjestaji/2013.pdf.
18. Furue M, Ebata T, Ikoma A, Takeuchi S, Kataoka Y, Takamori K, Verbalizing extremes of the visual analoguescale for pruritus: a consensus statementActa Derm Venereol 2013; 93: 214-15.
19. Fallahzadeh MK, Roozbeh J, Geramizadeh B, Namazi MR, Interleukin-2 serum levels are elevated in patients with uremic pruritus: a novel finding with practical implicationsNephrol Dial Transplant 2011; 26: 3338-44.
20. Mourad B, Heqab D, Okasha K, Rizk S, Prospective study on prevalence of dermatological changes in patients under hemodialysis in hemodialysis units in Tanta University hospitals, EgyptClin Cosmet Investig Dermatol 2014; 7: 313-39.
21. Ramakrishnan K, Bond TC, Claxton A, Sood VC, Kootsikas M, Agnese W, Clinical characteristics and outcomes of end-stage renal disease patients with self-reported pruritus symptomsInt J Nephrol Renovasc Dis 2014; 7: 1-12.
22. Ko MJ, Wu HY, Chen HY, Chiu YL, Hsu SP, Pai MF, Uremic Pruritus, Dialysis Adequacy, and Metabolic Profiles in Hemodialysis Patients: A Prospective 5-Year Cohort StudyPLoS One 2013; 8: e71404
23. Narita I, Iquchi S, Omori K, Gejyo F, Uremic pruritusJ Nephrol 2008; 21: 161-5.
24. Makhlough A, Emadi N, Sedighi O, Khademloo M, Bicmohamadi AR, Relationship Between Serum Intact Parathyroid Hormone and Pruritus in Hemodialysis PatientsIran J Kidney Dis 2013; 7: 42-6.
Notes
Source of Support: Nil,
Conflict of Interest: None declared.



Comments are closed.