Cutaneous tuberculosis in Niger: a 9-year retrospective study
Laouali Salissou1, Eric Adehossi2, Sani Maman Laouali1, Saidou Mamadou3, Hassan Nouhou4
1Department of Dermatology and Venereology, National Hospital of Niamey, Niamey, Niger, 2Department of Internal Medicine, National Hospital of Niamey, Niamey, Niger, 3Laboratory of Biology, National Hospital of Lamordé, Niamey, Niger, 4Laboratory of Histopathology, Faculty of Health Sciences, ABDOU Moumouni University, Niamey, Niger
ABSTRACT
Introduction: Cutaneous tuberculosis is a skin infection due to the Mycobacterium tuberculosis and rarely due to Mycobacterium bovis or Mycobacterium africanum. The disease is difficult to diagnose, given the fact that the skin is seldom a location for tuberculosis. The aim of this study is to determine the epidemiological, clinical and therapeutic profile of the disease in Niger.
Materials and Methods: This is a retrospective study over a period of 9 years in the Department of Dermatology and Venereology at the National Hospital of Niamey. The study included all cases of cutaneous tuberculosis that were clinically diagnosed and confirmed or not by some conventional complementary examinations.
Results: Over a period of nine years, 49 cases of cutaneous tuberculosis were diagnosed, which represents 0.34% of the total 14376 dermatological consultations in the dermatological unit. Patients of both sexes were affected, but the majority were male with 69% or a sex ratio M/F of 2.26. The patients ranged in age from 6 to over 60 years. The mean age was 34.67 years. Patients between 31 and 40 years were the most affected at 34.69%. A personal or family history of tuberculosis was noted in 8.16% of the cases. Scrofuloderma is the most frequent form of the disease (93.87% of the cases). The average course of the disease before consultation was 30.28 months. The tuberculin skin test was positive in 83.67% of the cases. The TB smear test was positive in only 6% of the cases. The hyperleukocytosis, which was mostly lymphocytic, was noted in 21.62% of the cases. Radiological evaluation was normal in 91.83% of the cases. All patients responded well in 100% of the cases with a treatment period ranging from 6 to 9 months. No clinical and/or biological treatment-related side effects were observed.
Conclusion: Cutaneous tuberculosis is still a common infection in third world countries where it affects both sexes. The scrofuloderma is the most observed form in our study. A TB test-based treatment is often a good solution in the face of an array of clinical and epidemiological evidence. Systematic vaccination after birth would drastically reduce all forms of tuberculosis.
Key words: Cutaneous tuberculosis; therapeutic response; Niger
INTRODUCTION
Cutaneous tuberculosis, like any non-pulmonary form of the disease, is most often due to the Mycobacterium tuberculosis and rarely due to Mycobacterium bovis or Mycobacterium africanum [1]. The disease is difficult to diagnose because of its rarity and clinical polymorphism. The diagnosis relies on a body of epidemiological, clinical, para-clinical evidence or just on test evaluation. Its treatment is based on TB antibiotics, which in most cases gives excellent results [2–6]. The aim of this study is to determine the epidemiological, clinical and therapeutic profile of the disease in Niger.
MATERIALS AND METHODS
This is a retrospective study carried over a period of 9 years in the Dermatology and Venereology Unit at the National Hospital of Niamey. The study included cases of cutaneous tuberculosis and their handling for the period between January 2004 and December 2012. Data collection was carried out using a survey form that specified epidemiological, clinical, para-clinical and therapeutic information.
Consultation records at Dermatology and Venereology Unit from 2004 to 2012 were used as source of information. For this study, we considered all cases of cutaneous tuberculosis that were treated with standard therapy regimes involving 2 months of quadruple therapy (isoniazid, rifampicin, pyrazinamide, and ethambutol) following by futher 4 months of izoniazid associated to rifampicin. All data were entered in and processed with EXCEL 2007.
Ethics
This study was performed on human subjects; thus, all patients were aware of the presence of the study and they were fully informed about the drug and its side-effects.
RESULTS
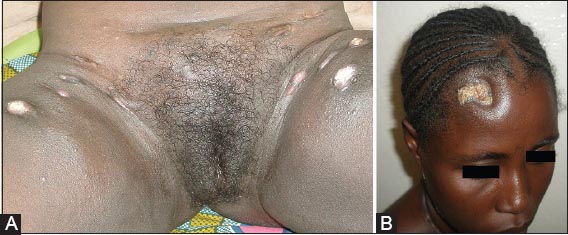
Cutaneous tuberculosis occurred in 49 cases, out of a total of 14376 dermatological consultations over 9 years (or 0.34% of the cases). The average annual cases was 5.44. The patients were 34 men (69%) and 15 women (31%) or a sex ratio M/F of 2.26. The subjects ranged in age from 6 to over 60 years. The mean age was 34.67 years. The age group between 31 and 40 years was most represented (34.69% of the cases). Four patients (8.16% of the cases) showed a personal or family history of tuberculosis. Weight loss was the most frequent clinical sign (32.65% of the cases), followed by fever (26.53%) and anorexia (22.44%). Scrofuloderma (Fig. 1) was the most common manifestation of the disease (93.87% of the cases), followed by tuberculosis verrucosa cutis (4.08%) and tuberculous gumma (2.04%).
The average course of the disease before consultation was 30.28 months and ranged from 2 to 156 months. The major folds (inguinal and axillary) were the most common sites (30.61% of the cases). There were other important affected areas such as the neck, the trunk and the pelvic limbs (Figs 2A and 2B) (each at 12.24% of the cases). In 55.10% of the cases, the disease was restricted to one area only, and to two areas in 24.48% of the cases. Attacks in more than three area represented 20.42% of the cases. The tuberculin skin test was performed on all patients and was positive in 83.67% of the cases. A diameter of induration measuring 16 to 24 mm was observed in 41.46% of the cases, with a mean value of 15.41 mm. The smear test was positive in 6% of the cases. Lymphocytic hyperleukocytosis was noted in only 21.62% of the cases followed untyped anemia in 13.51% of the cases. The accelerated rate of sedimentation was significant only in 10.81% of the cases. Chest radiographs were performed on 37 patients and were normal in 33 of the them (91.83%). However, 4 patients (8.16%) showed pathological radiographs (such as geodes, osteoporosis and shrinking of the space between vertebral bones). Most of histopathology results showed granulomatous dermatitis. So, the diagnosis of CTB was based on classic combination of clinical, epidemiologic laboratory features and responses to anti-tuberculosis therapy.
Among the 39 patients, 37 underwent a regular TB treatment, first during 2 months in a daily quadruple therapy (isoniazid 3 to 5 mg/Kg/day, rifampicin 10 mg/Kg/day, pyrazinamid 20 to 30 mg/Kg/day; and ethambutol 15 to 20 mg/Kg/day) and then during 4 months in a daily bitherapy (isoniazid 3 to 5mg/Kg/day, rifampicin 10 mg/Kg/day). For the whole patients, we adjusted the doses. All 37 patients were cured at the end of the treatment like in those images (Figs 3, 4A, 4B and 5).
DISCUSSION
In our study, cutaneous tuberculosis accounted for 0.34% of all consultations in dermatology with an annual incidence of 5.44 cases. The annual number of cases reported in other studies varies from less than 1 to 8.6 cases [4,6]. Our study showed that the disease affected young subjects with a male predominance, as is noticed in other studies [7–10]; although other studies found a feminine predominance [5,6,11].
In our study, the scrofuloderma was the most common cutaneous form accounting for 93.87% of the cases. Some publications have also reported the prevalence of this form [6,8,10]. In our study, tuberculosis verrucosa cutis and the tuberculosis of the gum were less important, at 4.08% and 2.04% of the cases, respectively. This is not congruent with other studies, where tuberculosis verrucosa has a frequency of 19.59% [12] and the tuberculous gumma frequency of 46.6% [13]. The average course of the disease before the consultation was 30.28 months in our study. In some studies [10,11], this period ranged from 16 to 38.4 months, confirming the chronic aspect of the disease. Location in the large folds (30.61% of the cases) was predominant in our study; while in other studies the most frequent the cervical area and the lower limbs [5,11] were most affected. Overall, we founded that the disease affects many more skin areas than what is usually reported in other studies [6,11]. In our study the tuberculin skin test was positive in 83.67% of the cases, the smear test was positive in 6% of the cases. The chest radiograph was normal in 91.83% of the cases and most of histopathology results showed granulomatous dermatitis. This points to the heterogeneous nature of the para-clinical aspects. The same heterogeneity is reported in other studies [13,14]. All of the 37 patients in our study were totally cured. This result is also reported in other studies [5,9,11,15]. This confirms the effectiveness of conventional TB therapy protocols. We noted no clinical or laboratory side effects related to the TB treatment.
CONCLUSION
Cutaneous tuberculosis, although relatively rare, is still a concern in third world countries. Scrofuloderma and other cutaneous forms can be handled with a standard TB therapy. While a test-based TB treatment is often a good solution in the face of an array of clinical and epidemiological evidence, systematic vaccination at birth is the best way to combat all forms of tuberculosis.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
Written informed consent was obtained from the patient for publication of this article and any accompanying images.
REFERENCES
1. Dias MFRG, Bernardes Filho F, Quaresma MV, Nascimento LV, Nery JAC, Azulay DR, Update on cutaneous tuberculosisAn Bras Dermatol 2014; 89: 925-38.
2. Morand JJ, Lighburn E, Tuberculose cutanéeDermatol 2007; 98: Paris: EMC (Elsevier Masson SAS); 360.
3. Morand JJ, Garnotel E, Simon F, Lighburn E, Panorama de la tuberculose cutanéeMed Trop 2006; 66: 229-36.
4. Marcela Concha R, Félix Fich S, Ricardo Rabagliati B, Cristian Pinto S, Rocio Rubio L, Oscar Navea D, Tuberculosis cutanea: reporte de dos casos y revision de la literaturaRev Chil Infect 2011; 28: 262-8.
5. Abdelmalek R, Mebazaa A, Berriche A, Kilani B, Osman Ben B, Mokni M, Cutaneous tuberculosis in TunisiaMed Mal Infect 2013; 43: 374-8.
6. Garcia-Rodriguez JF, Monteagudo-Sanchez B, Marino-Callejo A, Cutaneous tuberculosis: a 15-year descriptive studyEnferm Infecc Microbiol Clin 2008; 26: 205-11.
7. Puri N, A clinical and histipathological profil of tuberculosis of patients with cutaneous tuberculosisIndian J Dermatol 2011; 56: 550-2.
8. Thakur BK, Verma S, Hazarika D, A clinicopathological study of cutaneous tuberculosis at Dibrugarh district, AssamIndian J Dermatol 2012; 57: 63-5.
9. Wang H, Wu Q, Lin L, Cui P, Cutaneous tuberculosis: A diagnostic and therapeutic study of 20 casesJ Dermatol Treatment 2011; 22: 310-4.
10. Kane A, Niang SO, Cissé M, Sy TN, Diallo M, Dieng MT, Tuberculose cutanée à Dakar: A propos de 151 casMali Méd 2010; 25: 4.
11. Eddaoui A, Chiheb S, Khadir K, Azzouzi S, Benchikhi H, Erythéme induré de bazin: 14 observations au Maroc, efficacité des antituberculeuxMéd Trop 2008; 68: 549.
12. Buhutto AM, Solangi A, Khaskhely NM, Arakaki H, Nonaka S, Clinical and epidemiological observations of cutaneous tuberculosis in Lanarka, PakistanInt J Dermatol 2002; 41: 159-65.
13. Akhdari N, Zouhair K, Habibedine S, Lakhdar H, Tuberculose cutanée de l’enfant au Maroc: Etude de 30 casArch Pédiatr 2006; 13: 1098-101.
14. Gallouj S, Amara B, Mikou O, Benjelloun MC, Mernissi FZ, Scrofuloderme révélant une tuberculose sternale primitiveMed Trop 2010; 70: 333-34.
15. Akdeniz S, Yildiz T, Ates G, Ataman A, Özekinci T, Harman M, Cutaneous tubercolosis In a Region of Southeast of TurkeyJ Turk Acad Dermatol 2011; 5: 2.
Notes
Source of Support: Nil
Conflict of Interest: None declared.




Comments are closed.