Acrodermatitis Enteropathica in an adult: a case report
Kanthilatha Pai1, Poornima Baliga1, Sathish Pai2, Swati Sharma1
1Department of Pathology, Kasturba Medical College, Manipal, Manipal University, Karnataka, India, 2Department of Dermatology, Kasturba Medical College, Manipal, Manipal University, Karnataka, India
ABSTRACT
Acrodermatitis enteropathica (ADE) is an uncommon, inherited disorder occurring due to defective Zinc absorption. It can occur as an acquired condition secondary to impaired intestinal absorption in a wide variety of clinical conditions or due to nutritional deficiency. It is clinically characterized by triad of acral dermatitis, alopecia and diarrhoea. The preferential involvement of acral and peri-orificial skin is a feature that is pathognomonic for zinc deficiency. We report a case of ADE in a 22 year old female with no underlying comorbid conditions.
Key words: acrodermatitis enteropathica; zinc deficiency; adult
INTRODUCTION
Acrodermatitis enteropathica (ADE) is an uncommon, inherited disorder occurring due to defective Zinc absorption. It can occur as an acquired condition secondary to impaired intestinal absorption in wide variety of clinical conditions or due to nutritional deficiency. It is clinically characterized by triad of acral dermatitis, alopecia and diarrhoea. The preferential involvement of acral and peri-orificial skin is feature that is pathognomonic for zinc deficiency [1].
It can be hereditary or acquired secondary to gastrointestinal disorders or in patients with prolonged total parenteral nutrition or due to nutritional deficiency [2]. Classical clinical manifestation consists of triad of peri-orificial dermatitis, diffuse thinning of hair and diarrhea. Recognition of this condition is important as it can be fatal in severe cases. It occurs due to impaired Zinc absorption and patients respond dramatically when treated with Zinc [3].
We report a case of ADE in a 22 year old female with no underlying comorbid conditions.
CASE REPORT
A 22 year old patient presented with itchy lesions over face, neck, cubital fossa, hands and feet since 4 months. There was no history of oozing or bleeding. Patient gave history of fissuring with pain and burning. She also gave history of burning sensation and excessive lacrimation and inability to close her eyes. There was no blurring of vision. She complained of increased hair loss since 6 months. There was no history of diarrhea/oral ulcers/Raynauds phenomena and photosensitivity. She gave no history suggestive of any systemic illness. No contributory family history was present. She was not on any medications. She is a strict vegetarian and consumes mostly cereals. On clinical examination, well defined erythematous scaly and shiny plaques with crusting over the periorbital, perioral and perianal region and all around the neck were seen (Fig. 1). Erythematous fissured plaques were seen over bilateral cubital fossa, tips of fingers, toes and soles of feet (Fig. 2). Scalp showed diffuse thinning of hair. There was ectropion of both lower eyelids. Patient gave history of necrotizing fasciitis of the left foot for which debridement and amputation was done a year ago (Fig. 3).
Her laboratory investigations revealed mild anemia (10.3 gm/dl) and raised erythrocyte sedimentation rate (45 mm/1hr). All other biochemical parameters including renal and liver function tests, blood sugar were within normal limits. Her HIV, HBsAg, HCV were non-reactive. ANA global was negative. Ultrasound abdomen, Chest X-Ray was normal. Serum zinc level was marginally low.
Patient has been treated with Zinc sulphate 200mg twice daily along with evening primrose oil 1 gm once a day, which contains essential fatty acid. Topically she was given white petroleum jelly twice a day along with diluted topical fluticasone propionate once at night. A diet containing leafy vegetables, nuts and legumes was advised. Patient is due for follow-up.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure
DISCUSSION
Acrodermatitis enteropathica (ADE) is an autosomal recessive disorder resulting in impaired zinc absorption or acquired, usually occuring in alcoholics. Zinc plays an essential role in catalytic, structural and regulatory functions in the human body. Deficiency of zinc manifests with multi-systemic manifestations, which can be fatal if not diagnosed and treated early.
ADE was first recognized by a Swedish dermatologist Thore Brandt in 1936 presenting with acral rash and diarrhoea. Later in the year 1973 Moynahan and Barnes associated the clinical finding with low plasma zinc level that responded dramatically when the patient was treated with zinc supplements [3].
Classical ADE is an autosomal recessive disorder and the defective gene is linked to a zinc transporting protein encoded on chromosome 8q24.3.5 by the gene SLC39A4. Since patients with hereditary acrodermatitis enteropathica may have minimal or no diarrhea and the correct diagnosis may be long delayed, the condition should not be considered strictly a disease of children.
Acquired zinc deficiency is widespread and is more common in populations who eat predominantly cereal proteins. It has been reported in a wide variety of clinical conditions including alcoholism, Crohn’s disease and intestinal malabsorption syndromes, total parenteral nutrition, nutritional deficiency, defect of mammary zinc secretion (lactogenic ADE), pancreatic disorders, burns, malignancies and renal disorders [4]. Our patient had no underlying comorbid conditions, and we attribute the Zinc deficiency to deficient dietary intake.
The classical dermatological features of zinc deficiency include dry, scaly, sharply demarcated, erythematous patches in the peri-orifial areas that can become vesicular, pustular or desquamative. Psoriasiform plaques are typically seen in the acral region. Nails show paronychia and transverse ridging. Scalp can show diffuse alopecia with severe deficiency or dry, brittle hair in milder cases.
The associated systemic features of zinc deficiency are diarrhea, anorexia, growth retardation in children, photophobia, corneal opacities, hyposmia, hypogonadism, amenorrhea, anemia, impaired wound healing, neuropsychiatric problems, and perinatal morbidity in pregnancy. requirement in pregnancy. Our patient did not have any underlying systemic manifestations except mild anemia.
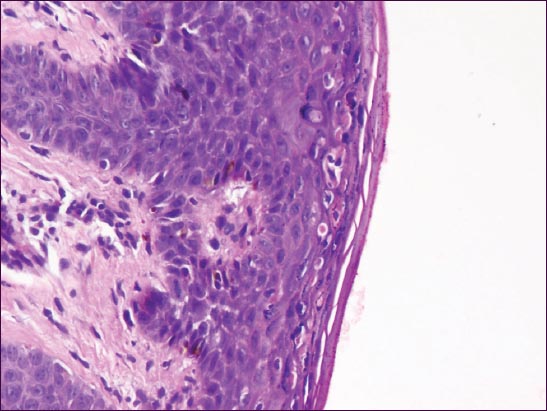
In the histopathology, necrolysis, characterized by cytoplasmic pallor, vacuolization, and ballooning degeneration of keratinocytes within the superficial epidermis of the epidermis which may subsequently lead to confluent necrosis of keratinocytes [5]. Other features are confluent parakeratosis, dimunition in the granular layer, dyskeratosis and psoriasiform hyperplasia. These findings need to be differentiated from necrolytic migratory erythema, seen in glucaganoma.
The most serious complication of ADE increased susceptibility to develop secondary infections, usually with Candida albicans, Staphylococcus aureus and Pseudomonas aeruginosa. Our patient had necrotizing fasciitis 1 year back for which she underwent debridement and amputation of great toe of left foot.
Establishing the diagnosis is by measuring plasma or serum zinc levels, although ADE with normal zinc levels has been reported. Treatment includes supplementation of elemental zinc at a dose of 2 mg/kg/day, at least two or three times the recommended dietary allowance of 15 mg/day.
CONCLUSION
This case highlights a case of ADE occurring in an adult, with no underlying comorbid conditions, presenting with peri-orificial erythematous rashes and diffuse alopecia.
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles.
REFERENCES
1. Mankaney GN, Vipperla K, Images in clinical medicine. Acquired acrodermatitis enteropathicaN Engl J Med 2014; 371: 67.
2. Wessells KR, King JC, Brown KH, Development of a plasma zinc concentration cutoff to identify individuals with severe zinc deficiency based on results from adults undergoing experimental severe dietary zinc restriction and individuals with acrodermatitis enteropathicaJ Nutr 2014; 144: 1204-10.
3. Puri N, A study on efficacy of oral Zinc therapy for treatment of Acrodermatitis EnteropathicaOur Dermatol Online 2013; 4: 162-6.
4. Perafán-Riveros C, França LF, Alves AC, Sanches JA, JrAcrodermatitis enteropathica: Case report and review of the literaturePediatr Dermatol 2002; 19: 426-31.
5. Maverakis E, Fung MA, Lynch PJ, Draznin M, Michael DJ, Ruben B, Acrodermatitis enteropathica and an overview of zinc metabolismJ Am Acad Dermatol 2007; 56: 116-24.
6. van Voorhees AS, Riba M, Acquired zinc deficiency in association with anorexia nervosa: Case report and review of the literaturePediatr Dermatol 1992; 9: 268-71.
Notes
Source of Support: Nil
Conflict of Interest: None declared.



Comments are closed.