Mimic of cellulitis: Primary cutaneous B cell lymphoma – Leg type
Sathish Pai1, Kanthilatha Pai2, Shrutakeerthi Shenoi2, Shastry BA3
1Department of Dermatology, Kasturba Medical College, Manipal University, Manipal, India 2Department of Pathology, Kasturba Medical College, Manipal University, Manipal, India 3Department of Medicine, Kasturba Medical College, Manipal University, Manipal, India
ABSTRACT
Primary cutaneous B-cell lymphoma, leg type, is an uncommon and aggressive subtype of Primary cutaneous B cell lymphoma that is recently updated by the World Health Organization–European Organization for Research and Treatment of Cancer classification of cutaneous lymphomas. We present a case of an 80-year-old woman who presented with redness and swelling mimicking cellulitis of her right leg, along with few skin colored nodules. Skin biopsy revealed pathology consistent with this entity. The patient was treated with systemic chemotherapy, but expired while on treatment secondary to sepsis.
Key words: Primary cutaneous B cell lymphoma; leg type; cellulitis
INTRODUCTION
Primary cutaneous B-cell lymphoma-LT (PCBCL-LT) belongs to a distinct group of B-cell lymphoproliferative disorders defined by its presentation in the skin, without evidence of extra cutaneous spread at the time of diagnosis [1]. It is a rare form of Primary cutaneous B cell lymphoma (PCBCL) that has an inferior prognosis when compared to other subtypes of PCBCL and requires treatment with aggressive chemotherapy.
CASE REPORT
An 80 year old female presented with complaints of pain and swelling of her right leg along with mild fever since 5 days. On clinical examination, the skin over her left leg appeared red and inflamed and was tender on palpation with local rise of temperature. Doppler study revealed no evidence of deep vein thrombosis. She gave history of similar complaints in the past that responded to antibiotics. Patient was treated with antibiotics, with partial response. The pain and swelling subsided but the redness persisted with thickening of skin, along with the presence of pea sized nodules (Figs 1 and 2). Hence a biopsy was taken with a clinical differential diagnosis of Pseudo Kaposi’s sarcoma, Pretibial myxedema and Cutaneous lymphoma.
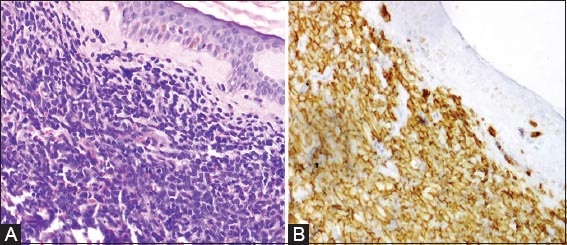
Histopathological examination revealed diffuse infiltration of the dermis by medium to large sized atypical monotonous appearing non cleaved lymphoid cells, that stained positive with CD20, CD 79a, Bcl2 and negative with CD 10 on immunohistochemistry (Fig. 3) suggesting a diagnosis of Primary cutaneous large cell lymphoma (PBLBCL) – leg type. Patient was started with systemic chemotherapy with rituximab, but developed sepsis secondary to severe neutropenia during the first cycle of chemotherapy and expired.
The patient’s informed consent was obtained.
Prior to the study, patient gave written consent to the examination and biopsy after having been informed about the procedure
DISCUSSION
The incidence of Cutaneous lymphoma is reported to be 0.5 to 1 per 100,000 [1]. While Most of the nodal lymphomas are B cell type, PBCBL account for only 20-25% of Cutaneous lymphomas. The new 2008 World Health Organization – European Organization for Research and Treatment of Cancer classification for cutaneous lymphomas classifies PCBCLs into three types: primary cutaneous marginal zone lymphoma (PCMZL), primary cutaneous follicular center lymphoma (PCFCL) and PCLBCL, LT [2].
PCLBCL, LT represents approximately 20% of all PCBCLs and 4% of all cutaneous lymphomas. This condition preferentially affects elderly women who usually present with rapidly growing red or bluish-red cutaneous nodules or tumors on one or both lower legs [3]. About 10% to 15% of these patients are noted to present with lesions outside of the lower extremities. Cutaneous lymphoma presenting as cellulitis has rarely been described in literature [4].
PCLBCL, LT is more aggressive and has a worse outcome when compared with other subtypes of PCBCLs (PCMZL and PCFCL). They frequently disseminate to lymph nodes and visceral organs [5].
A diagnosis of PCLBCL, LT is made based on Clinical, histologic, immunohistochemical and molecular studies [3]. Pathology reveals diffuse non-epidermotropic infiltrates made up of a monotonous population of large non-cleaved B cells that is seen extending into the subcutaneous tissue. There is absence of reactive or inflammatory cells in the background. The neoplastic cells express B-cell markers (CD12, CD20, CD22, CD79a) and also often express surface immunoglobulin. They are strongly positive for bcl-2, but the translocation t (14:18) characteristic of PCFCL is not a feature of PCLBL-LT [6]. Bcl-6, MUM-1 and FOXP1 are usually positively expressed, while CD10 and CD138 are negative. Fluorescent in situ hybridization studies reveal breakpoints in at least one loci involving IGH, MYC, BCL6 or MALT1 genes in majority of cases similar to its systemic counterpart.
While watch-and-wait strategies are often employed with the other subtypes PCBCL, aggressive systemic therapy with combination chemotherapy with or radiation therapy remains the recommended approach for PCLBCL, LT. Alternative therapy with systemic single-agent rituximab may be appropriate in elderly patients unable to tolerate multi agent chemotherapy; however, long-term data are lacking [7].
CONSENT
The examination of the patient was conducted according to the Declaration of Helsinki principles. Written informed consent was obtained from the patient for publication of this article.
REFERENCES
1. Pandolfino TL, Siegel RS, Kuzel TM, Rosen ST, Guitart J, Primary cutaneous B-cell lymphoma: review and current conceptsJ Clin Oncol 2000; 18: 2152-68.
2. Goodlad JR, Krajewski AS, Batstone PJ, McKay P, White JM, Benton EC, Primary cutaneous diffuse large B-cell lymphoma: prognostic significance of clinicopathological subtypesAm J Surg Pathol 2003; 27: 1538-45.
3. Grange F, Beylot-Barry M, Courville P, Maubec E, Bagot M, Vergier B, Primary cutaneous diffuse large B-cell lymphoma, leg type: clinicopathologic features and prognostic analysis in 60 casesArch Dermatol 2007; 143: 1144-50.
4. Falagas ME, Bliziotis IA, Rafailidis PI, Peppas G, Peripheral T-cell lymphoma masquerading as infectious cellulitisEur J Dermatol 2007; 17: 166-7.
5. Senff NJ, Noordijk EM, Kim YH, Bagot M, Berti E, Cerroni L, European Organization for Research and Treatment of Cancer and International Society for Cutaneous Lymphoma consensus recommendations for the management of cutaneous B-cell lymphomasBlood 2008; 112: 1600-9.
6. Geelen FA, Vermeer MH, Meijer CJ, Van der Putte SC, Kerkhof E, Kluin PM, bcl-2 protein expression in primary cutaneous large B-cell lymphoma is site-relatedJ Clin Oncol 1998; 16: 2080-5.
7. Fink-Puches R, Wolf IH, Zalaudek I, Kerl H, Cerroni L, Treatment of primary cutaneous B-cell lymphoma with rituximabJ Am Acad Dermatol 2005; 52: 847-53.
Notes
Source of Support: Nil
Conflict of Interest: None declared.


Comments are closed.