Our Dermatol Online. 2014; 5(4): 362-365
DOI:. 10.7241/ourd.20144.90
Date of submission: 12.08.2014 / acceptance: 20.09.2014
Conflicts of interest: None
AN EPIDEMIOLOGICAL ANALYSIS OF CHILDREN AND ADOLESCENTS PSORIASIS IN A TERTIARY REFERRAL DERMATOLOGY INSTITUTE IN THE DOMINICAN REPUBLIC
Manuel Valdebran, Martha Miniño
Instituto Dermatológico y Cirugía de Piel “Dr. Huberto Bogaert Díaz”, C/Federico Velásquez, esq. Albert Thomas, Santo Domingo, República Dominica
Corresponding author: Dr Manuel Valdebran e-mail: investigacion@valdebran.com
How to cite this article: Valdebran M, Miniño M. An epidemiological analysis of children and adolescents psoriasis in a tertiary referral dermatology institute in the Dominican Republic.
Our Dermatol Online. 2014; 5(4): 362-365.
Abstract
Introduction: Psoriasis is one of the most common chronic inflammatory diseases, affecting about 3.5% of the population. Despite psoriasis carries a high risk of morbidity, few epidemiological studies provide estimates on the prevalence of psoriasis in children.
Aim: The objective of this study is to report the frequency of children and adolescents diagnosed with psoriasis at Instituto Dermatologico y Cirugía de Piel “Dr. Huberto Bogaert Díaz” (IDCP-DHBD) between March 2007 and March 2012.
Material and Methods: Examination were done on 76 children and adolescents with psoriasis confirmed by histopathological examinations at the IDCP DHBD in the Dominican Republic between March 2007 and March 2012. The data was retrospectively reviewed to assess age, gender, clinical localization, treatment modalities and delay in diagnosis.
Results: The frequency of children and adolescents with psoriasis among dermatological patients was 0.96 cases for every 10,000 patients seen in the Institute. There were 43 (56.6%) girls and 37 (43.4%) boys. The mean age of onset was 14 years. Children from 0-2 years, were the least affected with 3% of the cases. The most frequent site of onset were the trunk (28.8%) and the scalp (27.4%). 67% of the patients had 2 or more sites involved. The mean delay in diagnosis was 6 months. Topical therapy was the treatment of choice in all the patients except one.
Conclusions: Even though psoriasis may cause a profound impact on the quality of life of children and adolescents the epidemiological data in the countries of Central America and the Caribbean is scarce.
Key words: psoriasis; children; Dominican Republic
Introduction
Psoriasis is one of the most frequent chronic inflammatory diseases in the world, affecting around 3.5% of the population [1]. It presents in the first two decades of life [2-5] in more than 33% of the cases; 10% of which will develop psoriasis before the age of 10 [6]. Besides being affected physically a child can potentially be affected socially and emotionally [7]. In fact, it has been reported that the quality of life of the children suffering psoriasis is worse than those suffering from other chronic diseases such as diabetes mellitus or epilepsy [8].
Epidemiology
Despite being a matter of concern, there are a few epidemiological studies that provide estimates of the prevalence of psoriasis in children worldwide, most of the available data we have at the present time comes from European countries where the prevalence is relatively high as opposed to what is seen in southern countries [9-13] as described in Figure 1.
.jpg) Figure 1. Frequency of children and adolescents psoriasis around of the world.
|
Etiology
Psoriasis is a chronic inflammatory condition probably mediated by T lymphocytes, endothelial cells, dendritic cells, monocytes, neutrophils, keratinocytes and cytokines and chemokines characterized by hyperproliferation of keratinocytes, endothelial vascular proliferation and an infiltrate of inflammatory cells. The IL-23/Th17 seems to be crucial in the pathogenesis of psoriasis, mediating the host’s inflammatory response [14].It has been demonstrated that the PSORS1 gene is determinant in the early onset of non-pustular type 1 psoriasis [5,15]. The HLA-Cw6 is the most important allele in the PSORS1 locus which confers susceptibility for the early onset of the disease [2,5,16,17]. Contrary to what has been described in adults, infections such as pharyngitis or skin trauma may trigger the disease [5,18]. Additionally, the onset of new lesions in periods of emotional stress is seen more frequently in children [18].
Aim
To report the number of diagnosed cases of psoriasis in children and adolescents at Instituto Dermatológico y Cirugía de Piel “Dr. Huberto Bogaert Díaz” (IDCP-DHBD) between March 2007 and March 2012
Material and Methods
This is a retrospective epidemiologic study from 76 children and adolescents with psoriasis confirmed by histopathological examinations at the IDCP DHBD in the Dominican Republic between March 2007 and March 2012. Information data was obtained from the clinical and histopathology records of the patients seen at the Institute. The data was retrospectively reviewed to assess age, gender, clinical localization, treatment modalities and delay in diagnosis.
Results
In total 76 children and adolescents with psoriasis were included in the study. The center registered a total of 789,558 patients seen in the clinical dermatology division in the period of time of the study. The frequency of children and adolescents with psoriasis among dermatological patients was 0.96 cases for every 10,000 patients seen in the Institute (Fig. 2). There were 43 (56.6%) girls and 37 (43.4%) boys, with a female to male ratio of 1.3:1 (Fig. 3). The mean age of onset was 14 years, with a peak age of onset seen in the group of adolescents from 12-18 years with 40.2% of the cases. Children from 0-2 years, were the least affected with 3% of the cases (Fig. 4). The most frequent site of onset were the trunk (28.8%) and the scalp (27.4%) (Fig. 5). It was found that 67% of the patients had 2 or more sites involved, while 32% of patients were affected in one body site. The period between the onset of the first skin lesions and the final diagnosis was designated as the delay in diagnosis. The mean delay in diagnosis was 6 months. Topical therapy was the treatment of choice in all the patients except one. Antralin was prescribed for 42% of the patients followed by betamethasone combined with calcipotriol, cade emulsion, topical corticosterioids and salicylic acid ointments. Systemic therapy with methotrexate was used in only one patient.
.jpg) Figure 2. Frecuency of juvenile psoriasis at IDCP in the Dominican Republic.
|
.jpg) Figure 3. Gender distribution of patients.
|
.jpg) Figure 4. Age distribution of patients.
|
.jpg) Figure 5. Most frequent site of onset.
|
Discussion
In terms of age of onset our data shows that 3.4% of patients were infants of 0-2 years, 12.6% less than 5 years and 54% less than 15 years. This results differs to the data of other regions of the world, for example in Australia, where 27% of the cases of psoriasis in children were reported in the group of patients of 0 – 2 years. But they are similar to areas like California which reports 2% of affected patients less than 2 years, 7% in 5 years or less, and 45% in the group of 12 years or less [12]. There have been reported racial differences on the groups affected by psoriasis; White and Asians seem to be the most affected while Hispanics and blacks are the least affected [12]. Our data reflects a low frequency of children and adolescents psoriasis. There is a mixture of races in the Caribbean area where there is a significant African American population. In the present series, girls were slightly more affected than boys in a 1.3:1 ratio. It was interesting to see that 67% of the patients presented with 2 or more body segments involved, which could correlate with a delay in the diagnosis found of 6 months. There is a need to educate the population about what is psoriasis, how the symptoms may be found in children and adolescents and how they may differ from the typical presentation of the adults.
Treatment
It is important to consider certain facts that in children could alter the course of the disease, for instance, infections may trigger the onset of psoriasis or may perpetuate it. [19] In this young age it is essential to verify the weight and height of the children and adolescents, especially to detect metabolic syndrome risk factors [20,21], and also search for sign and symptoms of psoriatic arthritis. The objective of the treatment is to improve the physical symptoms minimizing the effect of the disease in the psychosocial development of the child. When choosing a therapy it is imperative to think in the future health of the child as well as in his growth and development [7]. Based on the European consensus on the management of juvenile psoriasis [22] we propose that the first line of treatment for induction to remission on mild psoriasis defined as PASI ≤ 10, or BSA ≤ 10 or DLQI ≤ 10 should be topical steroids class II- IV; for transitional therapy topical steroids class IV-VI or calcipotriol plus steroids; and for maintenance therapy it should be considered the use of mild potency steroids, calcipotriol, tacrolimus and finally tar, antraline and salicylic acid compounds. In cases of moderate-to-severe psoriasis, defined as PASI ≥ 10 or BSA ≥ 10 or DLQI ≥ 10, it is indicative of the use of systemic therapy such as methotrexate, cyclosporine, oral retinoids or biologic agents. Alternatively narrow band ultraviolet B phototherapy could be considered for older children and adolescents. It is important to take into consideration the rotation, combination and sequential strategies when using these agents in order to improve the effectiveness of the treatment, its tolerance and to minimize the long term side effects of these agents (Fig. 6).
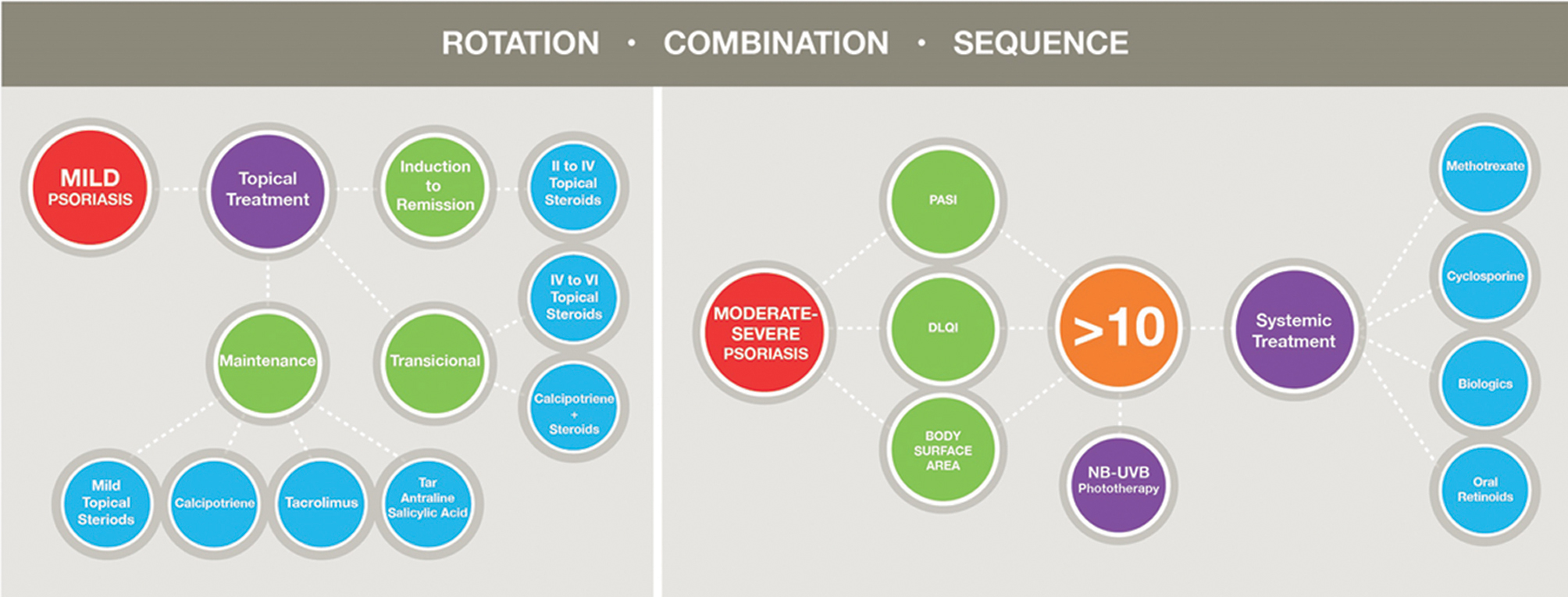 Figure 6. Therapeutic algorithm.
|
Conclusion
Even though psoriasis may cause a profound impact in the quality of life of children and adolescents the epidemiological data in the countries of Central America and the Caribbean is scarce. Psoriasis may impact the quality of life of children and adolescents and their parents in different ways than in adults, thus requiring separate studies. Many times the initial clinical presentation, the different trigger factors, and the different associations may be unrecognized by the parents and thus contribute to the delay in the diagnosis therefore more education should be given to the general population regarding this entity and specific therapeutic guidelines should be proposed.
REFERENCES
1. Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60:218-24.
2. Benoit S, Hamm H. Childhood psoriasis. Clin Dermatol. 2007;25:555-62.
3. Romiti R, Maragno L, Arnone M, Takahashi MD. Psoriasis in childhood and adolescence. An Bras Dermatol. 2009;84:9-20.
4. Rogers M. Childhood psoriasis. Curr Opin Pediatr. 2002;14:404-9.
5. Cordoro KM. Management of childhood psoriasis. Adv Dermatol. 2008; 24:125-69.
6. Farber EM, Jacobs AH. Infantile psoriasis. Am J Dis Child. 1977;131:1266-9.
7. Dogra S, Kaur I. Childhood psoriasis. Indian J Dermatol Venereol Leprol. 2010;76:357-65.
8. Beattie PE, Lewis-Jones MS. A comparative study of impairment of quality of life in children with skin disease and children with other chronic childhood diseases. Br J Dermatol. 2006;155:145-51.
9. Agustin M, Glaske G, Radtke MA, Christophers E, Reich K, Schafer I. Epidemiology and comorbidity of psoriasis in children. Br J Dermatol. 2010;162:633-6.
10. Gelfand JM, Weinstein R, Porter SB, Neimann AL, Berlin JA, Margolis DJ. Prevalence and treatment of psoriasis in the United Kindom: a population-based study. Arch Dermatol. 2005;141:1537-41.
11. De Jager ME, Van de Kerhof PC, De Jong EM, Seyger MM. Epidemiology and prescribed treatments in childhood psoriasis: a survey among medical professionals. J Dermatolog Treat. 2009;20:254-8.
12. Wu J, Helen-Black M, Smith N, Porter A, Jacobsen S, Koebnick C. Low prevalence of psoriasis among children and adolescents in a large multiethnic cohort in southern California. J Am Acad Dermatol. 2011;65:957-64.
13. Dogra S, Kumar B. Epidemiology of skin diseases in school children: A study from Northen India. Pediatr Dermatol. 2003;20:470-3.
14. Coimbra S, Figueiredo A, Castro E, Rocha-Pereira P, Santos-Silva A. The roles of cells and cytokines in the pathogenesis of psoriasis. Int J Dermatol. 2012.51:389-398.
15. Sticherling M, Augustin M, BoehnckeW, Christophers E, Domm S, GollnickH, et al. Therapy of psoriasis in childhood and adolescence – a German expert consensus. J Dtsch Dermatol Ges. 2011;9:815-23.
16. Sticherling M. Children and adolescents with psoriasis. What therapy is recommended? Hautarzt. 2012;63:192-201.
17. Silverberg NB. Pediatric psoriasis: an update. TherClin Risk Manag. 2009;5:849-56.
18. Leman J, Burden D. Psoriasis in children: a guide to its diagnosis and management. Paediatr Drugs. 2001 3:673-80.
19. Raychaudhuri SP, Gross J. A comparative study of pediatric onset psoriasis with adult onset psoriasis. Pediatric Dermatol. 2000;17:174-78.
20. Zindanc? I, Albayrak O, Kavala M, Kocaturk E, Can B, Sudogan S, et al. Prevalence of Metabolic Syndrome in Patients with Psoriasis. Scientific World J. 2012;2012:312463.
21. Langan SM, Seminara NM, Shin DB, Troxel AB, Kimmel SE, Mehta NN, et al. Prevalence of Metabolic Syndrome in Patients with Psoriasis: A Population-Based Study in the United Kingdom. J Invest Dermatol. 2012;132:556-62.
22. Ståhle M, Atakan N, Boehncke WH, Chimenti S, Daudén E, Giannetti A, et al. Juvenile psoriasis and its clinical management: a European expert group consensus. J Dtsch Dermatol Ges. 2010;8:812-8.
Comments are closed.