Our Dermatol Online. 2014; 5(3): 312-326
DOI:. 10.7241/ourd.20143.83
Date of submission: 30.04.2014 / acceptance: 16.06.2014
Conflicts of interest: None
DERMATOLOGY EPONYMS – SIGN – LEXICON – (M)
Piotr Brzeziński1, Patrice Bourée2, Anca Chiriac3,4, Jerry E. Bouquot5, Carmelo Schepis6, Thomas Hofer7, Susheera Chatproedprai8, Hitoshi Mizutani9
1Department of Dermatology, 6th Military Support Unit, Ustka, Poland
2Unité des maladies parasitaires, hôpital de Bicêtre, 94275 Kremlin-Bicêtre, France
3Department of Dermatology, Nicolina Medical Center, Iasi, Romania
4Department of Dermato-Physiology, Apollonia University Iasi, Strada Muzicii nr 2, Iasi-700399, Romania
5Department of Diagnostic & Biomedical Sciences, University of Texas School of Dentistry at Houston, Houston, Texas, USA
6Unit of Dermatology, Oasi Institute (IRCCS), Troina, Italy
7Dermatologie und Venerologie FMH, Private Practice, Wettingen, Switzerland
8Division of Ambulatory Pediatrics, Department of Pediatrics, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
9Department of Dermatology,Mie University, Graduate School of Medicine,Tsu, Japan
Corresponding author: Piotr Brzezinski, MD PhD e-mail: brzezoo77@yahoo.com
How to cite this article: Brzezinski P, Bourée P, Chiriac A, Bouquot JE, Schepis C, Hofer T, Chatproedprai S, Mizutani H. Dermatology Eponyms – Sign – Lexicon – (M). Our Dermatol Online. 2014; 5(3): 312-326.
Abstract
Eponyms are used almost daily in the clinical practice of dermatology. And yet, information about the person behind the eponyms is difficult to find. Indeed, who is? What is this person’s nationality? Is this person alive or dead? How can one find the paper in which this person first described the disease? Eponyms are used to describe not only disease, but also clinical signs, surgical procedures, staining techniques, pharmacological formulations, and even pieces of equipment. In this article we present the symptoms starting with (M) and other. The symptoms and their synonyms, and those who have described this symptom or phenomenon..
Key words: eponyms; skin diseases; sign; phenomenon
MACHUPO SIGN, [South America]
Fever and bleeding caused by the zoonotic Bolivian hemorrhagic fever Arenavirdae virus. Machupo virus is spread from its primary hosts, rodents, to humans via aerosol and vector-borne (infected ticks and mosquitoes) transmissions. Aerosol transmission occurs when an infected rodent secretes any bodily fluids, such as urine or saliva, on an area where it’s highly used by humans. Upon contact, a human becomes infected with the virus through inhalation of just a few organisms. From there, the machupo virus is able to produce a disease within the site of infection particularly in the lungs. The virus uses hilar lymph nodes and parenchymal organs for viral growth purposes. Machupo virus outbreak has been reported mostly in the country of Bolivia – agriculture remote area – and Bolivia’s surrounding countries. The reservoir hosts of this virus are rodents particularly in the family of Calomys callosus – the vesper mice. The recent major outbreak in Bolivia occurred during the 1962-1964 because of an increase population of the vesper rodents which resulted in over 1000 human cases of machupo virus infection [1,2].
MACLEAD’S SIGN
Rheumatoid arthritis with joint effusion [3,4].
RODERICK MACLEOD
Scotch physician, 1795-1852.
MADAGASCAR SIGN
Eosinophilia and seizures from the ingestion of infected arthropods containing eggs from the zoonotic Inermicapsifer cestoda [5].
MADURA FOOT SIGN
Chronic fungi caused disease, most common form in the foot, pus contains red, black and yellow granules [6-8].
MAGNAN’S SIGN
A frightening illusory sensation of a foreign body under the skin. A sign seen in cases of cocaine addiction [9].
VALENTIN JACQUES JOSEPH MAGNAN
French psychiatrist, 1835-1916 (Fig. 1). A pivotal figure in the historical classification of mental diseases. He studied medicine in Lyon and Paris. From 1867 to the end of his career he was associated with the Hôpital Sainte-Anne in Paris. Magnan was an influential figure in French psychiatry in the latter half of the 19th century. He is remembered for expanding the concept of degeneration that was first introduced into psychiatry by Bénédict Augustin Morel (1809-1873). Magnan’s theory of degeneration was a form of „evolutionary biology” that was based on an hereditary precept. He used terms such as bouffée délirante (transitory delusional psychosis) and délire chronique évolution systématique (chronic systemized delusional disorder) as descriptive categories of mental illness. [2] In 1892 with psychiatrist Paul Sérieux (1864-1947), he published a monograph on the latter mental state titled Le délire chronique a évolution systématique. Magnan believed that the prodiguous use of alcohol, particularly absinthe, was a major factor in what he perceived was a decline of French culture. In his investigations of absinthe he tried to establish a particular „absinthe effect” that wasn’t present in other forms of alcohol, and suggested that the delirium of absinthe was different from delirium tremens experienced in alcoholism. In his research with laboratory animals, Magnan used essence of absinthe (wormwood), rather than the beverage itself, which contains only a small percentage of wormwood. From his experiments he observed that animals experienced epileptiform convulsions when exposed to concentrated levels of wormwood [10].
 Figure 1. Valentin Jacques Joseph Magnan.
|
MAJOCCHI’S SIGN
Purpura annularis telangieciodes [11].
DOMENICO MAJOCCHI
Italian dermatologist, (1849–1929) (Fig. 2). He characterized Majocchi’s disease and Fungal folliculitis (also known as „Majocchi granuloma”). Born in Rome Roccalvecce, he completed his studies in Rome, where he graduated on 11, August, 1873. He entered the competition for the Hospital of St. Galligano and began his career as a dermatologist. In fact while passing other hospitals and doing extensive practice in operative surgery it had always been an object of his to study particularly the various branches of dermatology. His sifilografia of Venereology, lying today in the hospital of St. James, is an extensive treatise on syphilis of the nose and palate which remains vital and valuable still, along with other minor but noteworthy contributions. He became, in 1880, the first Chair of the University Clinic Dermosifilopatica Parma, a position which he help until 1892. During this period he made nu- Merosi disciples, he published valuable studies among which stand out in particular that of the granuloma tricofitico, a hitherto undescribed form that brought him great fame. In 1892 he was unanimously called to the chair of dermosifilopatia of Bologna, held it up to his retirement, that is, 1924, and in this golden age of his career, he published many works among which the most famous is the one on purpura annnlaris teleangectodes, dermatosis new linked perpetually to his name. He continued to bring new contributions to the study of granuloma tricofitico, published highly valuable memoirs on the rupee foliacea, various forms of ringworm, on ‚acariosis from wheat, etc.., also dealing with skin abnormalities (duplicatio supercilii, supernumerary frenulum, etc..) and more still of the History of Medicine (Syphilis in Bologna at the descent of Charles VIII, Jerome Mercuriale Marcello Malpighi, etc..). He retained to the last his activity as evidenced by its latest publication, left incomplete, that he was dictating to his niece a few hours before his death, on the teaching of dermatology in Bologna. A gentle and good person devoted to his clinic, his disciples, to his patients; complex shape of humanist, scientist, dermatologist, of sifilografo, a historian of medicine; appassionatissimo of music and the arts, lover of conversation with scholars and scholars (and in his time in Bologna and learned scholars did not defect) whose friendship kept in a special way, in his tireless activity found time to devote to all his favorite activities. Admirer and follower of the work of Ferdinand Hebra [12].
 Figure 2. Domenico Majocchi.
|
MALIGNANT MILITARY SIGN
A term referring to the fact that many more British soldiers died from dysentery during the Crimean War (1854-56) and the Boer War (1899-1902) than from enemy action. History reveals disease has proven to be more lethal than the enemy weapons in most military campaigns [13].
MAO’S SIGN (China)
Green teeth and the most extremely foul breath associated with the practice of cleaning the mouth by only rinsing with green tea.
“…..Eccentric, at any rate. In matters of personal care, for instance, Mao was strictly a minimalist. When Li first started treating him, he was startled to discover that the chairman had apparently never brushed his teeth. Instead, as with many Chinese peasants, he rinsed his mouth with tea, then chewed the leaves. The result was that Mao’s teeth were green and his gums oozed pus from infections. Li encouraged the Great Helmsman to brush, without much success. „Does a tiger brush his teeth?” Mao demanded…..” [14].
MAP SIGN
Zoonotic Mycobacterium avium subspecies paratubetrculosis. Causes chronic diarrhea, sometimes fatal. The bacterium is found in cattle, sheep, giraifes, wildebeest, antelope, and other ruminants [15].
HEINRICH ALBERT JOHNE (pronounced YOH-ne)
German pathologist (1839-1910) (Fig. 3). He contributed to the literature of actinomycosis and trichinosis and discovered a method of staining bacterial capsules. He was instrumental in the introduction of meat inspection. Johne’s disease, a paratuberculosis disease of cattle he described in 1895, is named for him [16].
 Figure 3. Heinrich Albert Johne.
|
MARBURG SIGN (Africa)
Rapid fever, muscle pain, vomiting, maculopapular rash with desquamation, liver involvement and bleeding. Moriality can be 30 percent, caused by the zoonotic Marburg hemorrhagic fever Filoviridae virus [17].
MARFAN’S SIGN
A red triangle on the tip of a furred or coated tongue. A sign of typhoid fever [18].
ANTOINE BERNARD-JEAN MARFAN
French paediatrician, 1858-1942 (Fig. 4). Marfan entered the medical school in Toulouse. After two years he went to Paris in 1879, became externe in 1880 and started an internship in 1882. After taking time out to do his military service, he graduated with a silver medal in 1886 and received his doctorate in 1887. He was Chef de clinique medicale 1889-1891, agrégé of paediatrics to the Faculté de Médecine de l’Université de Paris in 1892 and until 1901 deputised for Grancher in the Hôpital des Enfants Malades during the winter terms. It was here he became interested in pediatrics. In 1892 he was appointed assistant professor of paediatrics in the Paris faculty. Marfan was made head of the diphteria service at the Hospital for Sick Children and in 1910 professor of therapy. In 1914, at the age of 56 years, he was appointed as the first professor of infantile hygiene at the newly established pediatric clinic at the University of Paris. His career was spent at the Hôpital des Enfants Malades in the Rue des Sèvres, where he remained until his retirement in 1928. He was a member of the Académie de Médecine from 1914. In 1920 his chair was moved to the Hospice des Enfants-Assistés. The writing of his doctoral thesis, „Troubles and gastric lesions in pulmonary tuberculosis”, prompted Marfan’s interest in pulmonary tuberculosis. This paper gave rise to the concept known as the Marfan law, which noted the rarity of pulmonary tuberculosis following the healing of local tuberculous lesions because of the development of immunity. Marfan wrote: „One rarely records pulmonary tuberculosis in people who, during their childhood, had been attacked by the disease and in whom lesions had healed before the age of 15 years”. Research such as this led to the development of the BCG vaccine. Marfan was one of the first to recognise the importance of skin reactions and when von Pirquet developed his technique for skin testing for tuberculosis he immediately employed this in his clinical studies which became classics. Marfan published extensively on pediatric themes and in 1897 was co-author of Treatise of Children’s Diseases which was awarded the prize of the French Academy of Sciences. He investigated the harmful effects of feeding infants goat’s milk and made extensive researches on rachitis. He was undoubtedly the pioneer in paediratrics in France and one of the most outstanding figures in his time. He stated: «In medicine it is always necessary to start with the observation of the sick and to always return to this as this is the paramount means of verification. Observe methodically and vigorously without neglecting any exploratory procedure using all that can be provided by physical examination, chemical studies, bacteriological findings and experiment, one must compare the facts observed during life and the lesions revealed by autopsy.» [19]. In 1896 Marfan, presented the case of a 5-year-old girl, Gabrielle P, to the Société Médicale des Hôpitaux de Paris. Marfan pointed out Gabrielle’s disproportionately long limbs. and asthenic physique. Her mother had noticed the abnormalities already at birth. The fingers and toes were exceptionally long and slender, making a spider-like impression. Marfan used the term „pattes d’araignée”, spider’s legs, and called the condition dolicostenomely (Greek: stenos = narrow, slender; melos = limb). Gabrielle P’s striking abnormalities of the skeletal system progressed to the time of her death in early adolescence, probably from tuberculosis [Marfan, 1938]. The first to use the term Marfan’s syndrome was Henricus Jacobus Marie Weve (1888-1962) of Utrecht in 1931.
 Figure 4. Antoine Bernard-Jean Marfan.
|
MARIE’S DISEASE SIGN
Akromegaly [20].
PIERRE MARIE
French neurologist, 1853-1940 (Fig. 5). After finishing medical school, he served as an interne (1878), working as an assistant to neurologist Jean-Martin Charcot (1825–1893) at the Salpêtrière and Bicêtre Hospitals in Paris. In 1883 he received his medical doctorate with a graduate thesis on Basedow’s disease, being promoted to médecin des hôpitaux several years later (1888). In 1907 he attained the chair of pathological anatomy at the Faculty of Medicine, and in 1917 was appointed to the chair of neurology, a position he held until 1925. In 1911 Marie became a member of the Académie de Médecine. One of Marie’s earlier contributions was a description of a disorder of the pituitary gland known as acromegaly. His analysis of the disease was an important contribution in the emerging field of endocrinology. Marie is also credited as the first to describe pulmonary hypertrophic osteoarthropathy, cleidocranial dysostosis and rhizomelic spondylosis. In his extensive research of aphasia, his views concerning language disorders sharply contrasted the generally accepted views of Paul Broca (1824–1880). In 1907, he was the first person to describe the speech production disorder of foreign accent syndrome. Marie was the first general secretary of the Société Française de Neurologie, and with Édouard Brissaud (1852–1909), he was co-founder of the journal Revue neurologique. His name is associated with the eponymous Charcot–Marie–Tooth disease, being named along with Jean-Martin Charcot and Howard Henry Tooth (1856–1925) [21]. Associated eponyms: „Marie’s ataxia”: an hereditary disease of the nervous system, with cerebellar ataxia. „Marie-Foix-Alajouanine syndrome”: cerebellar ataxia of the cerebellum in the elderly; usually due to alcohol abuse. „Marie’s anarthria”: inability to articulate words due to cerebral lesions. „Marie–Strümpel Disease”: also known as Ankylosing spondylitis; a severe arthritic spinal deformity. „Marie-Léri syndrome”: hand deformity caused by osteolysis of the articular surfaces of the fingers. „Bamberger-Marie disease”: also known as Hypertrophic pulmonary osteoarthropathy.
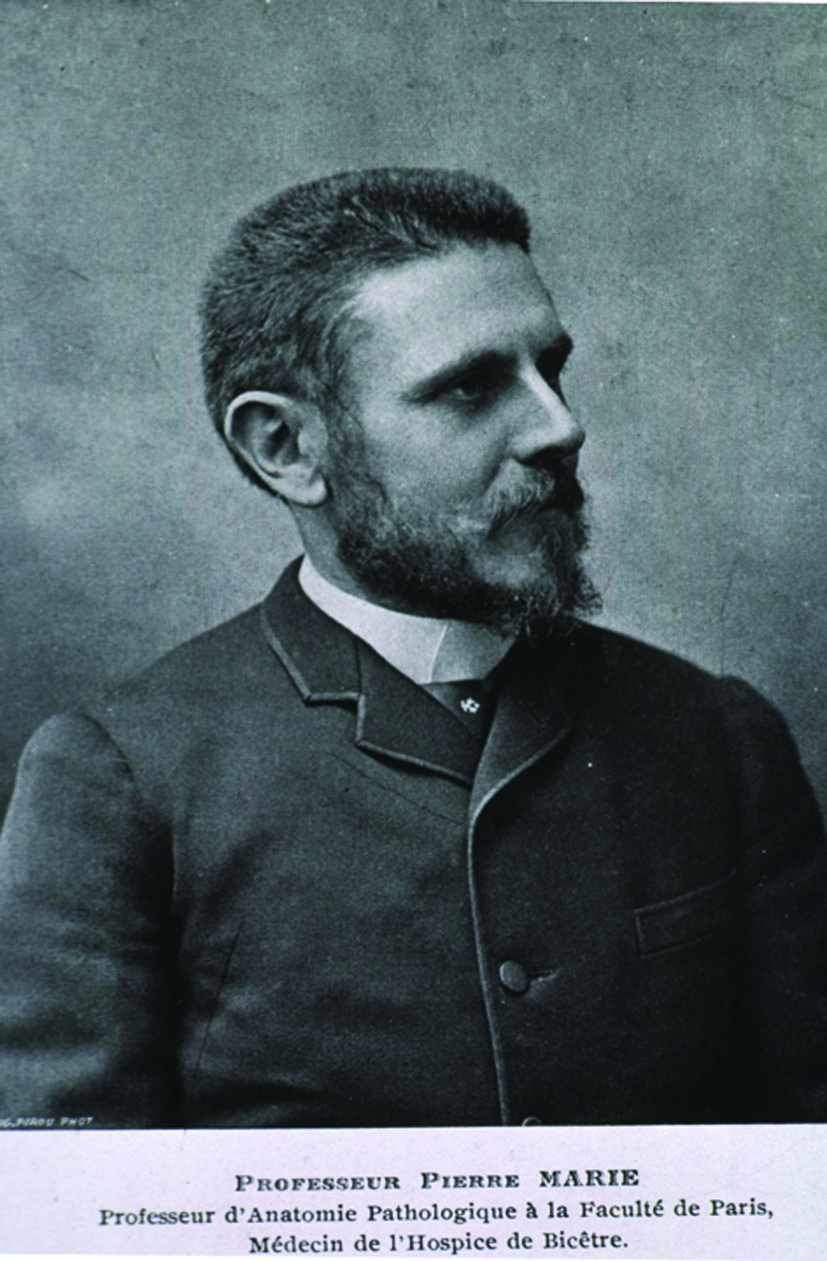 Figure 5. Pierre Marie.
|
MARINER’S SIGN
A sign of religious mutilation in which Tonga natives cut off a portion of the little finger. “……amongst an earlier generation of Tongans it was comparatively rare to find anyone who lived a long life with both little fingers intact…..” [22].
MARSHALL’S SIGN
Bagginess of the eyelids and bloated facies that give the patient an appearance of a wax doll. A sign of myxoedema. Also known as wax doll sign [23].
GEOFFREY MARSHALL
British physician.
MARTIN’S SIGN
Martin described a remarkable variety of ichthyosis in which the skin was covered with strong hairs like the bristles of a boar. When numerous and thick the scales sometimes assumed a greenish-black hue. An example of this condition was the individual who exhibited under the name of the „alligator-boy.” The skin affected in this case resembled in color and consistency that of a young alligator (Fig. 6). Also called Alligator’s sign (Martin and Taylor) [24].
 Figure 6. Martin’s sign.
|
MATCHBOX SIGN
Patient having delusions of parasitosis (acarophobia, entomophobia) collects skin debris with mistaken belief that such collected material contains alleged parasite in a matchbox, tissue paper, or small container (Fig. 7). This whole exercise executed by the patient is referred to as „matchbox sign.” [25,26].
 Figure 7. Different containers in which patients bring „Evidence of parasites”.
|
MATHIEU’S SIGN
Severe leptospirosis [27,28].
ALBERT MATHIEU
French physician, 1855-1917 (Fig. 8). He studied in Paris and became an interne in 1878. He was particularly influenced by Ernest-Charles Lasègue (1816-1883) and Charles Lailler (1822- 1893), and in 1883 received his doctorate with a remarkable thesis on purpura haemorrhagica. He first mainly concerned himself with dermatology, but after having been chef de clinique with Germain Sée (1818-1896) in 1883, he turned to the study of digestive diseases, in which field he made important contributions. He worked at the Hôpital St.-Andral 1896, and then worked in the Hôpital St.-Antoine [29].
 Figure 8. Albert Mathieu.
|
MCDOUGALL’S POWDER SIGN
The presence of a white stain around the mouth and brown stains, known as eschars on the skin of the face. Indicating suicide from the intake of McDougall powder, a sewage deodorant and parasitc insecticide made from carbolic acid [30]. Sign described by Alexander Mcdougall and Robert Angus Smith.
ROBERT ANGUS SMITH
British chemist, (1817–1884) [30].
MEAL TAG SIGN
Tattoos containing clear names and registration numbers on military personnel to be used if needed for post mortem identification. Often located on the ribs.
MECCA SIGN (c. 1831)
Epidemic marking cholera’s first devastating invasion of Mecca, site of Islam’s holiest shrine. Cholera epidemics appeared more than 40 times between 1831 and 1912 during the Muslim pilgrimage. The disease was then widely dispersed as the followers of Muhammad returned home and the term Mecca of disease came into use, meaning: The place where diseases come from. Today in the 21st century, pilgrims to Saudi Arabia are especially at risk of contracting a meningococcal infection which causes fatal meningitis and fatal septicaemia blood poisoning. Vaccination requirements are now in place for the multiple sub groups of the meningococcus bacterium. The modern Mecca sign would now be defined as infections relating to the meningococeus bacterium instead the cholera bacillus [31].
MEFFERT’S SIGN
It is described in Fordyce’s disease, characterized by presence of ectopically located sebaceous glands on the lips, oral mucosa and less commonly on gums. Prominent lip involvement can result in a lipstick like mark left on the rim of a glass mug after consuming a hot beverage (Meffert’s sign) [32].
MEIGE’S SIGN
A form of hereditary edema of the legs. Also called Milroy’s sign [33].
HENRI MEIGE
French physician, 1866-1940 (Fig. 9). He studied medicine in Paris under Jean Charcot (1825–1893), earning his doctorate in 1893. Afterwards he worked at the Salpêtrière and the École des Beaux-Arts, where in the 1920s he was appointed professor. With Édouard Brissaud he researched skeletal changes in acromegaly, concluding that gigantism in adolescents is fundamentally the same disease as acromegaly in adults. During World War I he conducted studies of neuropathy with Pierre Marie. Meige is best known for his work with extrapyramidal lesions. In 1902, with Eugene Feindel, he published an important work on motor disturbances, blepharospasms and tics. In contrast to Charcot, Meige asserted that disturbances of the extrapyramidal system were manifestations of pathological changes outside the pyramidal system. He was editor of the journals Nouvelle iconographie de la Salpêtrière and Schriftleiter of the Revue Neurologique [34]. Related eponyms: Meige’s syndrome I; Meige’s syndrome II; Nonne-Milroy-Meige disease.
 Figure 9. Henri Meige.
|
MEIROWSKY SIGN
Darkening of existing melanin, perhaps by oxidation, beginning within seconds and complete within minutes to a few hours after exposure to ultraviolet radiation [35].
EMIL MEIROWSKY
German-American dermatologist, 1876-1960. Meirowsky studied at the universities of Berlin and Königsberg, where he received his doctorate in 1901. He spent his hospital service and time as an assistant at the Berlin Polyclinic at Oscar Werl, in Wroclaw in Albert Neisser, Paul Gerson Unna and in Paris. In 1919 he received the title of professor. In 1920 he was habilitated at the University of Cologne, a year later he was appointed extraordinary professor. He was chairman of the Cologne Chamber of Physicians and a member of the German Democratic Party. In 1939 he emigrated to England. In 1947 he emigrated to the United States. Meirowsky conducted research on the origins of melanin. In 1906 he proved (in Unna’s laboratory) that the epidermis can produce melanin. According to him, the Meirowsky phenomenon (1909), the tanning of the skin, is produced by high temperatures. His daughter Lisa Maria Meirowsky was also a doctor and was murdered in the concentration camp Auschwitz-Birkenau. His brother was the entrepreneur and art collector Max Meirowsky [36].
MELTING SIGN
The gingival tissues turn from normal pink to purple-black and appear to melt away. Awash in a flow of haemorrhage and the eyes may weep tears of blood. An indication of envenomation by the Dispholidus typus—Boomslang viper (Fig. 10). Also referred to as the Sahara plague [37].
 Figure 10. Dispholidus typus—Boomslang viper.
|
E. A. WHILE
American historian-archaeologist
MENANGLE SIGN (New South Wales, Australia)
Fever from exposure to infected fruit bats or pigs carrying the zoonotic Menangle virus [38].
MENDEL’S SIGN
The patient experiences anesthesia of the popliteal space. A sign of tabes dorsalis. Also known as Mendel-Bekhterev sign [39].
VLADIMIR MIKHAILOVICH VON BEKHTEREV
Russian neurologist and psychiatrist, 1857-1927 (Fig. 11). To the lay public Vladimir Bekhterev is known for Bekhterev’s disease, pelvospondylitis. Bekhterev’s most important work, however, was in the study of reflexes and the morphology of the brain. He is the founder of psycho reflexology, transmitting to humans the same pattern of thinking that Pavlov had developed in his work on conditioned reflexes in dogs, and he used similar experiments. He enrolled at the Military Medical and Surgical Academy in St. Petersburg in 1873, at 16 years of age. After graduating in 1878 he held a position at the psychiatric clinic in St. Petersburg. It was here that he turned to the field that would make him famous: the anatomy and the physiology of the brain. In 1881 Bekhterev defended his dissertation for the medical doctorate that dealt with the possible relation between body temperature and some forms of mental illness. He was habilitated for Privatdozent of neurology and psychiatry in 1881 and was appointed associate professor – Dozent – that year. In 1895 he returned to Russia to become professor of psychiatric diseases at the University of Kazan. In 1913 he founded the State Institute for the Study of the Brain, which today bears his name. Independently of Pavlov Bekhterev developed a theory of conditioned reflexes, studying both inherited an acquired reflexes in the laboratory. He also accumulated a considerable volume of data on skeletal reflexes that was later applied in neurology. Bekhterev’s most lasting work was his research on brain morphology and his original description of several nervous symptoms and illnesses. He discovered the superior vestibular nucleus (Bekhterev nucleus) as well as several previously unknown brain formations. He also described numbness of the spine (Bekhterev’s disease) and new forms of syphilitic-sclerosis, motor ataxia and spondylitis. [40].
 Figure 11. Valdimir Mikhailovich von Bekhterev.
|
KURT MENDEL
German neurologist, 1874-1946 (Fig. 12). In 1897 he received his doctorate from Kiel, and in 1899 went to work at the policlinic of Emanuel Mendel in Berlin. Kurt Mendel was an editor of Neurologisches Zentralblatt. With Russian neurophysiologist Vladimir Bekhterev (1857-1927), the eponymous Mendel- Bekhterev reflex is named, which is flexion of the toes caused by percussion of the upper surface of the foot, a sign of lesions of the pyramidal tract [41].
 Figure 12. Kurt Mendel.
|
MENDEL-BEKHTEREV SIGN
See Mendel’s sign.
METAL LINE SIGN
A line on the gums nearly identical to the lead line, but is caused by mercury. A sign of treatment for venereal disease [42].
METCHNIKOFF’S SIGN
In Pfeiffer’s phenomenon, if the animals are given an intraperitoneal injection of bouiIlon or other material. Twelve hours before the test, lytic phenomena are replaced by phagocytosis [43].
ELIE METCHNIKOFF
Nobel laureate, Russian zoologist, 1845-1916 (Fig. 13). Best known for his pioneering research into the immune system. Mechnikov received the Nobel Prize in Medicine in 1908, shared with Paul Ehrlich, for his work on phagocytosis. He is also credited by some sources with coining the term gerontology in 1903, for the emerging study of aging and longevity. He attended Kharkiv University where he studied natural sciences, completing his four-year degree in two years. He then went to Germany to study marine fauna on the small North Sea island of Heligoland and then at the University of Giessen, University of Göttingen and then at Munich Academy. While he was at Giessen, he discovered, in 1865, intracellular digestion in one of the flatworms, an observation which was to influence his later discoveries. Travelling on to Naples he prepared a thesis for his Doctorate on the embryonic development of the cuttle-fish Sepiola and the Crustacean Nelalia. In 1867 he returned to Russia to the appointment of docent at the newly established Imperial Novorossiya University (now Odessa University), followed by an appointment at the University of St. Petersburg. In 1870 he returned to Odessa to take up the appointment of Titular Professor of Zoology and Comparative Anatomy. Mechnikov became interested in the study of microbes, and especially the immune system. In 1882 he resigned his position at Odessa University and set up a private laboratory at Messina to study comparative embryology, where he discovered phagocytosis after experimenting on the larvae of starfish. He realized that the process of digestion in micro-organisms was essentially the same as that carried out by white blood cells. His theory, that certain white blood cells could engulf and destroy harmful bodies such as bacteria, met with scepticism from leading specialists including Louis Pasteur, Behring and others. At the time most bacteriologists believed that white blood cells ingested pathogens and then spread them further through the body. He worked with Émile Roux on calomel, an ointment to prevent people from contracting syphilis, a sexually transmitted disease. Mechnikov also developed a theory that aging is caused by toxic bacteria in the gut and that lactic acid could prolong life. Based on this theory, he drank sour milk every day. He wrote three books: Immunity in Infectious Diseases, The Nature of Man, and The Prolongation of Life: Optimistic Studies, the last of which, along with Metchnikoff’s studies into the potential life-lengthening properties of lactic acid bacteria (Lactobacillus delbrueckii subsp. bulgaricus), inspired Japanese scientist Minoru Shirota to begin investigating a causal relationship between bacteria and good intestinal health, which eventually led to the worldwide marketing of kefir and other fermented milk drinks, or probiotics. In honor of this great and illustrious researcher, The Russian Empire created the prestigious Mechnikov Medical Academy in St. Petersburg. One of the most prestigious institutions in the training of physicians and senior professionals in Russia [43].
 Figure 13. Elie Metchnikoff.
|
METH MOUTH SIGN
The front teeth are often missing or black and broken down, due to the heat and dry mouth associated with smoking methamphetamine. Also known as Crack Teeth sign [44].
MEYERSON PHENOMENON
Meyerson phenomenon is an uncommon clinical condition that is characterized by an eczematous halo surrounding a preexisting melanocytic nevus and numerous other lesions (Fig. 14a, b) [45]. In 1971, Meyerson described two patients that presented erythema, desquamation and pruritus concerning exclusively nevi, localized on the trunk and close extremities and that improved after therapeutics with topical corticosteroids. Since then, this phenomenon has been described in various pigmented lesions including junctional nevi , Sutton nevi, atypical nevi and congenital ones. It was even documented in non-melanocytic lesions such as basal cells carcinomas, spinocellular carcinomas, seborrheic keratosis, keloids, histiocytofibromas and insect bites [46].
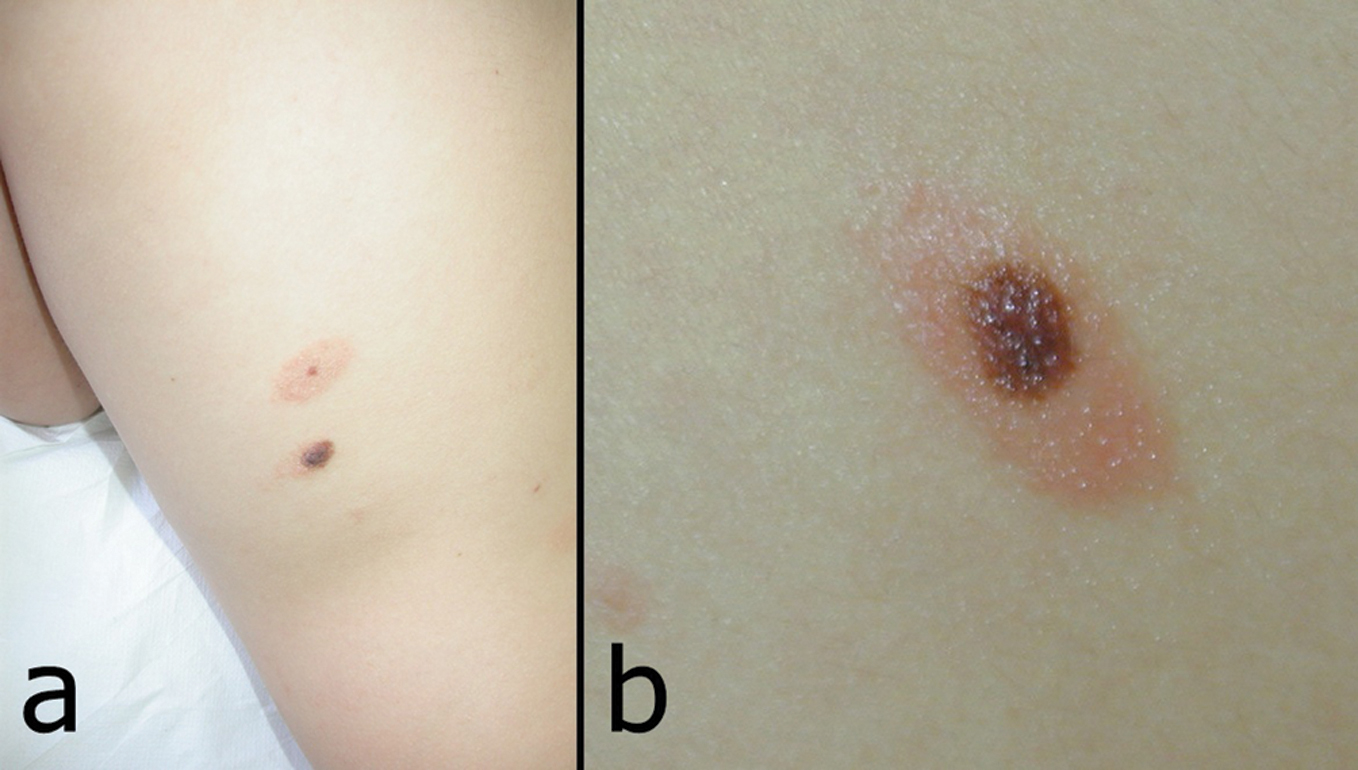 Figure 14a and b. Meyerson phenomenon.
|
ÉMILE MEYERSON
Polish-born French epistemologist, chemist, and philosopher of science, 1859-1933 (Fig. 15). Meyerson was educated in Germany and studied chemistry under Robert Wilhelm Bunsen. In 1882 Meyerson settled in Paris. He served as foreign editor of the Havas news agency, and later as the director of the Jewish Colonization Association for Europe and Asia Minor. He became a naturalized French citizen after World War I [47].
 Figure 15. Émile Meyerson.
|
MIASMATIC SIGN
One due to malaria poisoning [48].
MIBELLI’S SIGN
Porokeratosis with yellow brown patches and red and white dike like borders (Fig. 16). Also called keratodermia [49-51].
 Figure 16. Mibelli’s sign.
|
VITTORIO MIBELLI
Italian dermatologist, 1860-1910 (Fig. 17). He studied in Siena and, following further education in Florence, became prosector in the anatomical institute in Siena, and subsequently assistant in the dermatological clinic in that town. He was habilitated in 1888, from 1889 worked with Paul Gerson Unna in Hamburg and 1890 came to the University of Cagliary as extraordinary professor and director of the skin clinic. In 1892 he was called to Parma, where he was appointed ordinarius in 1900 and was active until his death in 1910 [52].
 Figure 17. Vittorio Mibelli.
|
MICKEY SIGN
Giddiness, blueness of the face, coldness of extremities and unconsciousness. A sign of chloral hydrate or chloralamide poisoning [53].
MIKULICZ’S SIGN
Chronic enlargement of the lacrimal and salivary glands, due to replacement of the glandular tissue by lymph-cells: called also achroacytosis [54].
JOHANN VON MIKULICZ-RADECKI
Polish-Austrian surgeon, 1850-1905 (Fig. 18). He was professor in Kraków, Wrocław, and Królewiec (Königsberg). Inventor of new operating techniques and tools, one of the pioneers of antiseptics and aseptic techniques. In Poland he is regarded as one of the founders of the Kraków school of surgery. After finishing studies at the University of Vienna under Theodor Billroth he was a director of surgery at the Jagiellonian University in Kraków, the University of Königsberg (Królewiec, Kaliningrad) and from 1890 at the University of Wrocław. Mikulicz-Radecki’s innovations in operative technique for a wide variety of diseases helped develop modern surgery. He contributed prodigiously to cancer surgery, especially on organs of the digestive system. He was first to suture a perforated gastric ulcer (1885), surgically restore part of the oesophagus (1886), remove a malignant part of the colon (1903), and describe what is now known as Mikulicz’ disease. In 1881 he developed improved models of the esophagoscope and gastroscope. As an ardent advocate of antiseptics he did much to popularize Joseph Lister’s antiseptic methods. He created a surgical mask and was the first to use medical goves during surgery [55].
|
Figure 18. Johann Von Mikulicz-Radecki.
|
MILIAN’S SIGN
In subcutaneous inflammation of the head and face, the ears are not involved but in skin diseases they are. Erysipelas and cellulitis have traditionally been defined as acute inflammatory processes of infectious origin that primarily affect the dermis (in the case of erysipelas) or deeper dermis and subcutaneous tissue in cellulitis. It is a sign used to distinguish between erysipelas and cellulitis of the facial region, where there is involvement of ear in erysipelas and sparing in cellulitis, as there is no deeper dermal tissue and subcutaneous fat [56]. Also known as Milian’s Ear sign.
GASTON AUGUSTE MILIAN
French dermatologist, 1871-1945 [56].
MILIAN’S EAR SIGN
see Milian’s sign.
MILITARY SWEATS SIGN (after c. 1775, France)
Unknown lethal infection killing significant numbers of peasants [57].
MILK MAID SIGN
Vesicles on the hands that become pustular often with lymph node swelling. Exposure to cattle, lions, and tigers that are infected with the zoonotic cowpox virus [58].
MILROY’S SIGN
A form of hereditary edema of the legs. Also called Meige’s sign [59].
WILLIAM FORSYTH MILROY
American physician, 1855-1942 (Fig. 19). William Forsyth Milroy studied medicine at the University of Rochester and the Johns Hopkins Hospital. He graduated from the College of Physicians and Surgeons, University of Columbia, in 1882 and had his internship in New York. He commenced practice in Omaha, Nebraska, and in 1885 he was appointed professor of histological pathology at the New University medical college. In 1894 he became professor of clinical medicine at the University of Nebraska. He retired in 1933 [60].
 Figure 19. William Forsyth Milroy.
|
MIRCHAMP’S SIGN
When a sapid substance, such as vinegar, is applied to the mucous membranę of the tongue, a painful reflex secretion of saliva in the gland about to be affected is indicative of sialadenitis, e.g., mumps [61].
MITCHELL’S SIGN
Erythromelalgia (Fig. 20) [62]. The term erythromelalgia, specific to the myeloproliferative disorders, refers to the occlusion of the microcirculation by platelets and is characterized by redness, congestion, and painful burning sensations of the extremities. Symptoms are characteristically relieved by cold or elevation of the extremity.
 Figure 20. Erythromelalgia.
|
SILAS WEIR MITCHELL
American neurologist and writer known for his discovery of causalgia, 1829-1914 (Fig. 21). He studied at the University of Pennsylvania in that city, and received the degree of M.D. at Jefferson Medical College in 1850. During the Civil War he had charge of nervous injuries and maladies at Turners Lane Hospital, Philadelphia, and at the close of the war became a specialist in neurology. In this field Mitchell’s name became prominently associated with his introduction of the rest cure, subsequently taken up by the medical world, for nervous diseases, particularly neurasthenia and hysteria. His medical texts include Injuries of Nerves and Their Consequences (1872) and Fat and Blood (1877). Mitchell’s disease (erythromelalgia) is named after him. He also coined the term phantom limb during his study of an amputee. Silas Weir Mitchell discovered and treated causalgia (today known as CRPS/RSD), a condition most often encountered by hand surgeons. He is considered the father of neurology as well as an early pioneer in scientific medicine. He was also a psychiatrist, toxicologist, author, poet, and a celebrity in America and Europe. His many skills and interests led his contemporaries to consider him a genius on par with Benjamin Franklin. His contributions to medicine and particularly hand surgery continue to resonate today [63].
 Figure 21. Silas Weir Mitchell.
|
MIZUTANI’S SIGN (Round finger pad sign)
It is seen in Raynaud’s phenomenon associated with systemic sclerosis. This sign refers to the disappearance of the peaked contour on fingerpads and replacement with a hemisphere-like fingertip contour especially on ring fingers (Figs. 22a, b) [64]. Sign was described by Hitoshi Mizutani and Tomoko Mizutani.
 Figure 22a. Finger tip of a patient with systemic scleroderma with positive for round finger pad sign.
|
 Figure 22b. Finer tip of a healthy control subject with the peaked contour.
|
MOELIER-BARLOW’S SIGN
Subperiosteal hematoma in rickets [65].
“Under this name, and under the name of MÖLLER-BARLOW’S disease, a condition has been described in which a hemorrhagic effusion takes place under the periosteum, which is quite rare, but nevertheless interesting. Six cases of this rare disease have recently been recorded by BRUN andRENAULT, of Paris, in La Presse Médicale, Jan. 12, 1898.
MOELIER-BARLOW’S SIGN
Subperiosteal hematoma in rickets [65].
“Under this name, and under the name of MÖLLER-BARLOW’S disease, a condition has been described in which a hemorrhagic effusion takes place under the periosteum, which is quite rare, but nevertheless interesting. Six cases of this rare disease have recently been recorded by BRUN andRENAULT, of Paris, in La Presse Médicale, Jan. 12, 1898. These six cases were observed in the Hospital for Children’s Diseases during the past two years. The first case was that of a girl of three months. The father and mother were healthy, but a younger brother had died in convulsions. The child was born at term after a normal labor and had been nursed for six months. It was brought to the Hospital because of the swelling of the right thigh. The general appearance of the child was good…”
JULIUS OTTO LUDWIG MÖLLER
German surgeon, 1819-1887. He studied in Königsberg, Halle and Vienna, receiving his doctorate in 1840. He was physician in Königsberg from 1841, until 1863 extraordinary professor of practical medicine, director of the medical policlinic and Medcinalrath. In 1863 he was «politisch gemassregelt» and laid down the named positions. From 1845 to 1863 he wrote a number of treatises in various journals [66].
SIR THOMAS BARLOW
English physician, 1845-1945 (Fig. 23); known for his research on infantile scurvy. He studied as an undergraduate at Manchester and London. University College London (UCL) Bachelor of Medicine (BM) in 1873 and Doctor of Medicine (MD) 1874. He became a registrar at Great Ormond Street Hospital, and later a physician and in 1899 a consultant. He was professor at the UCL from 1895 to 1907, initially of paediatrics and later of clinical medicine. Barlow’s disease – infantile scurvy – is named after him. He was Royal Physician to Queen Victoria and attended her on her death, and to King Edward VII and King George V. He was knighted as a Knight Commander of the Royal Victorian Order in March 1901, and in February 1902 he was created a Baronet, of Wimpole Street in St Marylebone in the County of London. [4] He was President of the Royal College of Physicians from 1910–1914 and delivered their Harveian Oration in 1916 on the subject of Harvey, The Man and the Physician. He was elected a Foreign Honorary Member of the American Academy of Arts and Sciences in 1918 [67].
 Figure 23. Thomas Barlow.
|
MOELLER’S TONGUE SIGN
Generalized loss of filiform papillae of the tongue in pernicious and other anemias. Early cases present as enlargement and tenderness of the papillae, a form of chronic lingual papillitis (CLP) (Figs. 24a – c) [68]. CLP is an innocuous entity represented by focal or diffuse enlargement of numerous lingual papillae, primarily the filiform papillae. It appears to usually have an adult onset and most likely represents papillary reaction to very low-grade, chronic irritation or desiccation. Some cases with childhood onset, however, seem to be variations of normal anatomy. No treatment or biopsy is required, but a number of systemic disorders and syndromes must be ruled out before applying the CLP diagnosis. Also called Moeller’s glossitis.
 Figure 24a – c. a) Moeller’s glossitis in Vitamin B12 deficiency (pernicious anemia) presenting as a diffuse loss of filiform papillae on the tongue, with remaining nodules representing unaffected fungiform papillae; b and c) early Moeller’s glossitis in Vitamin B12 affecting only the tip of the tongue, with an area of enlarged, tender papillae, sometimes referred to as chronic lingual papulosis.
|
MÖLLER
German surgeon, 1829-1862
MOKOLA FEVER SIGN (Africa)
Fatal encephalitis caused by a zoonotic rabies lyssavirus. The disease course does not have the classic rabies signs [69].
MONGOL SPOT SIGN
A birthmark on the lower back of Peruvian children with Asian lineage which later disappears (Fig. 25). Also known as „Mongolian blue spot” [70].
 Figure 25. Mongol Spot sign.
|
MONGOLISM SIGN
Down syndrome [71].
JOHN LANGDON HAYDON DOWN
English physician, 1828-1896 (Fig. 26). At the age of 18 he was supporting himself as an assistant to a surgeon in private practice on White Chapel Road, where he had the opportunity to concern himself with blood-letting, tooth extraction etc. A few months later, in 1847, he was allowed to commence work at the laboratory of The Pharmaceutical Society in Bloomsbury Square, London, where he made great progress and concentrated his efforts in organic chemistry. In 1849 he became assistant to professor Redwood and subsequently became research assistant to Michael Faraday. Down was predicted a brilliant career at the university hospital, but surprised his teacher when he, in 1858, became resident physician and subsequently medical superintendent at the Earlswood Asylum for Idiots in Surrey. He was elected assistant physician to the London Hospital in 1859 shortly after Mr. Jonathan Hutchison had been elected assistant surgeon. He was conferred doctor of medicine in London in 1859. Down wanted to work for the then hitherto gravely neglected mentally retarded children, and for a period of ten years (1858- 1868) he shared his time between the Earlswood institution for the mentally retarded and his London practice. Down became a lecturer on materia medica and therapeutics at the London Hospital Medical College and afterwards lecturer in the principles and practice of medicine. For the first 9 years following this appointment he continued to live at the Earlswood Asylum and to work there and superintend the asylum’s organisation and development. This resulted in a model for the care of the mentally ill in the UK. Down described mongolism in his Letsom lectures entitled «On some of the mental afflictions of childhood an youth» delivered in 1887. He published relatively little, but was awarded several medals for his publications on psychiatry. Down’s monograph Mental Affections of Childhood and Youth, published in 1887, contained the classic description of the condition which now bears his name. He also mentioned adrenogenital dystrophy, which gained recognition more than 40 years later as Fröhlich’s syndrome (adiposogenital syndrome, entered as Babinski-Fröhlich syndrome or disease, under Joseph François Félix Babinski, French Neurologist,) [71].
 Figure 26. John Langdon Haydon Down.
|
MONKEY BITE SIGN
Vesicular blisters and encephalitis, including seizures and coma. Very high mortality caused by the bites or scratches of Old World monkeys infected with the zoonotic ceropithecine herpesvirus-simiae type B [72].
MONKEY PANCREATITIS SIGN
Acute panereatitis caused by a tapeworm infection in the biliary tract. The zoonotic infection is usually associated with consumption of raw pork viscera, but can also be found in monkeys. Also called Asian taeniasis disease [73].
MONKSHOOD SIGN
Prickling and tingling sensations with giddiness and possible numbness in the mouth. The prickling feeling spreads on to the face and then to the whole body. A sign of aconite or aconitine poisoning [74]. Also known as Aconite sign.
MONTEVERDE’S SIGN
Failure of any response to the subcutaneous injection of ammonia. A sign of death [75].
N. N. MONTEVERDE
1885-1952 [75].
MOON’S SIGN
Domed-topped first molars seen in congenital syphilis [76].
HENRY MOON
English dental surgeon, 1845-1892 (Fig. 27) [77]. Henry Moon qualified in London in medicine and dentistry, emigrated to New Zealand, eventually returning to London. He is known for his observations of the malformation of tooth cusps in children with congenital syphilis.
 Figure 27. Henry Moon.
|
MORPHEA SIGN
Circumscribed scleroderma presenting in patches and bands (Fig. 28) [78].
 Figure 28. Morphea sign.
|
MORQUIO SIGN
Mucopolysaccharidosis IV or Morquio’s [79].
LUIS MORQUIO
Uruguayan physician and professor, (1867–1935) (Fig. 29). He graduated in 1890 and obtained his doctorate two years later for a thesis on the treatment of typhoid fever. In 1893 Morquio paid his first visit to Europe, spending a year as intern broadening his experience, especially in Paris, where he pursued his chosen field of paediatrics at Jacques- Joseph Grancher’s clinic for sick children. He worked with Antoine Bernard-Jean Marfan and was present at the clinics of Jean Martin Charcot, Pierre Charles Édouard Potain and Paul Georges Dieulafoy as well as Georges Hayem (1841-1933) and Étienne Lanceraux. He returned to Uruguay in 1894 and opened practice as a paediatrician. During his absence, his faculty had created a chair of paediatrics and on his return Morquio was appointed second in command, succeeding to the professorship in 1900. He was professor of internal pathology 1895-1900. In 1915 he was a founder of the Sociedad uruguaya de pediatría. Morquio maintained links with his colleagues in France, where he was elected to membership of several academic societies. The French government conferred upon him the rank of officer of the Légion d’Honneur and in 1930, in Geneva, he was elected president of the international Save the Children Society. In 1930 he was appointed director of Clínica Pediátrica y Puericultura – the Institute of Clinical Pediatrics in Montevideo. Morquio’s academic activities extended to many aspects of congenital and acquired disorders of childhood and he was the author of numerous publications in the field of pathology and hygiene of paediatrics, and two paediatric textbooks. Morquio was an amicable man who was esteemed by his colleagues throughout the world. He died suddenly in 1935 at the age of 68 years, and after his death a bust was erected in his honour at the institute of paediatrics, Montevideo [80].
 Figure 29. Luis Morquio.
|
Acknowledgement
PP Favier Anne Laure – IRBA-Unité de Virologie, Laboratoire d’accueil : IBS, 6 rue Jules Horowitz, 38000 Grenoble, France
Prof. Toshiyuki Yamamoto – Department of Dermatology, Fukushima Medical University, Fukushima 960-1295, Japan
Dr ZhengYong Yuan – Department of Urology and Dermatology, Dujiangyan Medical Center, Dujiangyan, Sichuan Province, China
Dr Salvador Labrador, MD – Clinica Trasmiera, Cantabria, Spain
Dr Heinz Feldmann – Laboratory for Zoonotic Diseases and Special Pathogens, National Microbiology Laboratory, Public Health Agency of Canada, Winnipeg, Manitoba, Canada
From Figures:
Figure 6. – Dr. Vinzenz Oji – Department of Dermatology, University of Münster, Münster, Germany and Interdisciplinary Center of Clinical Research, University of Münster, Münster, Germany
Figure 16. – Prof. Beatriz Di Martino Ortiz – Cátedra de Dermatología. Hospital de Clínicas. Facultad de Ciencias Médicas. Universidad Nacional de Asunción. Paraguay
Figure 17. – Dr Khalid Al Aboud – Department of Public Health, King Faisal Hospital, Makkah, Saudi Arabia
REFERENCES
1. Meyer AG, Sawyer SL, Ellington AD, Wilke CO. Analyzing machupo virus-receptor binding by molecular dynamics simulations. Peer J. 2014;2:e266.
2. Markin VA, Pantiukhov VB, Markov VI, Bondarev VP. [Bolivian hemorrhagic fever]. Zh Mikrobiol Epidemiol Immunobiol. 2013;3:118- 26.
3. Schaumburger J, Trum S, Anders S, Beckmann J, Winkler S, Springorum HR, et al. Chemical synovectomy with sodium morrhuate in the treatment of symptomatic recurrent knee joint effusion. Rheumatol Int. 2012;32:3113-7.
4. Macleod R. Dr. Macleod on the Statistics of Rheumatism. Prov Med J Retrosp Med Sci. 1842;4:19-21.
5. González Núñez I, Díaz Jidy M, Núñez Fernández F. [Infection by Inermicapsifer madagascariensis (Davaine, 1870); Baer, 1956. A report of 2 cases]. Rev Cubana Med Trop. 1996;48:224-6.
6. Yogeesh HR, Chankramath S, Srinivasa S, Sravana Rajendran RP, Shenoy PK. A case of nocardia mycetoma occurring at the site of skin grafting. Our Dermatol Online. 2011;2:219-23.
7. Iffat H, Abid K. Mycetoma revisited. N Dermatol Online. 2011;2:147- 50.
8. Nazimuddin M, Chowdhury A, Parvin R, Uddin R, Razzak A, Hoque M. The madura foot – a case report. N Dermatol Online. 2011;2:70-3.
9. Dowbiggin I. Back to the future: Valentin Magnan, French psychiatry, and the classification of mental diseases, 1885-1925. Soc Hist Med. 1996;9:383-408.
10. Medea E. [Profiles of great physicians: how, when, where i have known them. Jacques Joseph Valentin Magnan (1835-1916)]. Minerva Med. 1965 Mar 10;56:361-3.
11. Kaplan R, Meehan SA, Leger M. A case of isotretinoin-induced purpura annularis telangiectodes of Majocchi and review of substance-induced pigmented purpuric dermatosis. JAMA Dermatol. 2014;150:182-4.
12. Caffaratto TM. [Giovanni Domenico Majocchi, pioneer of social obstetrics]. Minerva Ginecol. 1959;11:40-5.
13. Linton DS. „War dysentery” and the limitations of German military hygiene during World War I. Bull Hist Med. 2010;84:607-39.
14. Bill Hewitt B. The Tyrant’s Physician. People. 1994;42:e (http:// www.people.com/people/archive/article/0,,20104202,00.html)
15. Hashemi M, Madani R, Razmi N. Evaluation of immunodominant proteins of mycobacterium avium paratuberculosis cell wall by Western blot analysis. Monoclon Antib Immunodiagn Immunother. 2014;33:101- 8.
16. Mathijsen A, Oldenkamp EP. [Predecessors: veterinarians from earlier times (48). Heinrich Albert Johne (1839-1910)]. Tijdschr Diergeneeskd. 2002;127:460-1.
17. Mbonye A, Wamala J, Winyi-Kaboyo, Tugumizemo V, Aceng J, Makumbi I. Repeated outbreaks of viral hemorrhagic fevers in Uganda. Afr Health Sci. 2012;12:579-83.
18. Bal SK, Czarnowski C. A man with fever, cough, diarrhea and a coated tongue. CMAJ. 2004;170:1095.
19. Gott VL. Antoine Marfan and his syndrome: one hundred years later. Md Med J. 1998;47:247-52.
20. Ellsworth CA, Neelon FA. Marie’s disease. N C Med J. 1988;49:662.
21. Pearce JM. A note on Pierre Marie (1853-1940). J Neurol Neurosurg Psychiatry. 2004;75:1583.
22. Collocott EEV. Notes on Tongan religion. J Polynesian Soc. 1921;30:152-163.
23. Lohiya S, Lohiya V, Stahl EJ. Pretibial myxedema without ophthalmopathy: an initial presentation of Graves’ disease. Am J Med Sci. 2013;346:73-5.
24. Brzeziński P, Wass J, White K, Daboul MW, Arlt W, van den Hombergh P, et al. Dermatology eponyms – phenomen / sign – Dictionary (A) – continued. N Dermatol Online. 2011;2:27-34
25. Bourée P, Benattar B, Périvier S. [Ekbom syndrome or delusional parasitosis]. Rev Prat. 2007;57:585-9.
26. Lee WR. Matchbox sign. Lancet. 1983;2:457-8.
27. Mamuchishvili N, Kuchuloria T, McHedlishvili I, Imnadze P. [Leptospirosis in georgia]. Georgian Med News. 2014;:63-6.
28. Brzeziński P, Chiriac A, Arenas R, Dori GU, Monteiro R, Cairncross S, et al. Dermatology Eponyms – sign –Lexicon (L). Our Dermatol Online. 2014;5:217-30.
29. http://www.whonamedit.com/doctor.cfm/944.html
30. Hamlin C. Smith, (Robert) Angus (1817–1884). Oxford Dictionary of National Biography, Oxford University Press, 2004 [http://www.oxforddnb.com/view/article/25893/2004-09]
31. Chiffoleau S. [Pilgrims to Mecca, germs and the international community]. Med Sci (Paris). 2011;27:1121-5.
32. Landenberger H, Siepmann K, Rohrbach JM. [Hyperplasia of sebaceous glands (Fordyce’s disease) in an oral mucocutaneous graft: 45-year follow-up]. Klin Monbl Augenheilkd. 1999;214:185-7.
33. Tammer ME, Plogmeier K, Schneider W. [Surgical therapy of scrotal edema in elephantiasis congenita hereditaria (Meige type)]. Urologe A. 2002;41:493-5.
34. Tolosa ES, Klawans HL. Meiges disease: a clinical form of facial convulsion, bilateral and medial. Arch Neurol. 1979;36:635-7.
35. Findlay GH, Van der Merwe LW. The Meirowsky phenomenon. Colour changes in melanin according to temperature and redox potential. Br J Dermatol. 1966;78:572-6.
36. Hollander A. Emil Meirowsky. Arch Dermatol. 1960;82:644.
37. Mass spectrophotometric evidence for P-III/P-IV metalloproteinases in the venom of the Kamiguti AS, Theakston RD, Sherman N, Fox JW. Boomslang (Dispholidus typus). Toxicon. 2000;38:1613-20.
38. Barr JA, Smith C, Marsh GA, Field H, Wang LF. Evidence of bat origin for Menangle virus, a zoonotic paramyxovirus first isolated from diseased pigs. J Gen Virol. 2012;93:2590-4.
39. Bowsher D, Lahuerta J. A case of tabes dorsalis with tonic pupils and lightning pains relieved by sodium valproate. J Neurol Neurosurg Psychiatry. 1987;50:239-41.
40. Kesselring J. VladimirMikhailovic Bekhterev (1857-1927): strange circumstances surrounding the death of the great Russian neurologist. Eur Neurol. 2011;66:14-7.
41. Hofer HG. [Men in a critical age: Kurt Mendel and the controversy over the male climacterium]. Urologe A. 2011;50:839-45.
42. Forrai J. [Dental aspects of general symptoms in the 18th century]. Orv Hetil. 2009;150:979-83.
43. Tan SY, Dee MK. Elie Metchnikoff (1845-1916): discoverer of phagocytosis. Singapore Med J. 2009;50:456-7.
44. Brown C, Krishnan S, Hursh K, Yu M, Johnson P, Page K, et al. Dental disease prevalence among methamphetamine and heroin users in an urban setting: a pilot study. J Am Dent Assoc. 2012;143:992-1001.
45. Hassan I, Sajad P. Mayerson’s phenomenon in a cutaneous neurofibroma. Our Dermatol Online. 2012;3:227.
46. Al Aboud K. Eponyms linked to melanocytic nevi. Our Dermatol Online. 2012;3:374-6.
47. Émile Meyerson : portrait [http://fondation.laposte.fr/article.php3?id_article=1101]
48. Gregurić Gracner G1, Vucevac Bajt V. History of eradication of malaria in Croatia. Orvostort Kozl. 2002;47:145-55.
49. Valiente Rebull C, Rodríguez L, Martinez Braga G, Di Martino Ortiz B, Rodriguez Masi M, Knopfelmacher O, et al. [Porokeratosis. Report of three cases]. Our Dermatol Online. 2014;5:163-8.
50. Raghunath N, Vijayashankar M. Solitary Porokeratosis of Mibelli at an unusual site. Our Dermatol Online. 2012;3:330-2.
51. Kolanuvada P, Sujatha C, Ambika H. Disseminated superficial porokeratosis and anetoderma developing after acute pancreatitis. Our Dermatol Online. 2012;3:228-30.
52. Al Aboud K, Al Aboud D. Eponyms in the dermatology literature linked to Italy. Our Dermatol Online. 2013;4(Suppl.2):437-9.
53. Slatt KA. Crazy with chloral hydrate: a parent witnesses a paradoxical reaction. Gastroenterol Nurs. 2009;32:296-7.
54. Coloma-González I, Ruíz-García L, Flores-Preciado J, Encampira-Luna EO, Ceriotto A, Salcedo-Casillas G. Mikulicz’s disease. A case report. Arch Soc Esp Oftalmol. 2013;pii: S0365-6691:00229-3.
55. Al Aboud K, Al Aboud A. Eponyms in the dermatology literature linked to Poland. Our Dermatol Online. 2013;4(Suppl.2):424-5.
56. Mouquin M. [Queyrat and Milian]. Prophyl Sanit Morale. 1952;24:43-4.
57. Manring MM, Hawk A, Calhoun JH, Andersen RC. Treatment of war wounds: a historical review. Clin Orthop Relat Res. 2009;467:2168-91.
58. Steinborn A, Essbauer S, Marsch WCh. [Human cowpox/catpox infection. A potentially unrecognized disease]. Dtsch Med Wochenschr. 2003;128:607-10.
59. Raffa V, Campra D, Guarino R, Angellotti P, Ballardini G, Boscardini L, et al. [Congenital Milroy Oedema: a case report of a family]. Pediatr Med Chir. 2012;34(2):100-3.
60. [No authors listed]. William Forsyth Milroy (1855-1942): hereditary edema of the lower legs. JAMA. 1968;204:166.
61. Peters JW, Koot HM, de Boer JB, Passchier J, Bueno-de-Mesquita JM, de Jong FH, et al. Major surgery within the first 3 months of life and subsequent biobehavioral pain responses to immunization at later age: a case comparison study. Pediatrics. 2003;111:129-35.
62. Ajili F, Mansour HB, Ghedira H, Zriba S, Metoui L, Gharsallah I, et al. Digital ischemia due to Systemic Sclerosis associated to Essential Thrombocythemia: A case report. Our Dermatol Online 2013;4:508-10.
63. Bourke J. Silas Weir Mitchell’s The Case of George Dedlow. Lancet. 2009;373:1332-3
64. Mizutani H, Mizutani T, Okada H, Kupper TS, Shimizu M. Round fingerpad sign: an early sign of scleroderma. J Am Acad Dermatol. 1991;24:67-9.
65. [No authors listed]. Subperiosteal hematoma in rickets. JAMA. 1898;XXX:618-9.
66. http://www.whonamedit.com/doctor.cfm/559.html
67. http://hharp.org/library/gosh/doctors/thomas-barlow.html
68. Bouquot JE, Adibi SS, Sanchez M. Chronic lingual papulosis: new, independent entity or „mature” form of transient lingual papillitis? Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:111-7.
69. Francis JR, Nourse C, Vaska VL, Calvert S, Northill JA, McCall B, et al. Australian Bat Lyssavirus in a child: the first reported case. Pediatrics. 2014;133:e1063-7.
70. Abilkassem R, Agadr A. [Extensive mongolian spot: a clinical sign that deserves attention]. Pan Afr Med J. 2013;16:41.
71. Ellis H. John Langdon Down: Down’s syndrome. J Perioper Pract. 2013;23:296-7.
72. Zhu L, Han JB, Zhang XH, Ma JP, Lv LB, Zhang GH, [Epidemiological survey of a captive Chinese rhesus macaque breeding colony in Yunnan for SRV, STLV and BV]. Dongwuxue Yanjiu. 2012;33:49-54.
73. Wandra T, Sudewi AA, Swastika IK, Sutisna P, Dharmawan NS, Yulfi H, et al. Taeniasis/cysticercosis in Bali, Indonesia. Southeast Asian J Trop Med Public Health. 2011;42:793-802.
74. Brzeziński P, Sinjab AT, Campbell CM, Kentorp N, Sand C, Karwan K. Dermatology Eponyms – phenomen / sign –Lexicon (supplement). Our Dermatol Online. 2012;3:147-55.
75. [No authors listed] [In memory of N. N. Monteverde, 1885-1952]. Aptechn Delo. 1953;2:79.
76. Jacobi KP, Cook DC, Corruccini RS, Handler JS. Congenital syphilis in the past: slaves at Newton Plantation, Barbados, West Indies. Am J Phys Anthropol. 1992;89:145-58.
77. Waldron T. Henry Moon and his molars. Dent Hist. 2014;59:17-24.
78. Raveendra L, Raju BP, Nagaraju U, Vivekananda, Sundar PK, Keshavalu L. Atrophic type of morphea profundus – an Indian experience. Our Dermatol Online 2013;4:172-5.
79. Unger S, Lausch E, Stanzial F, Gillessen-Kaesbach G, Stefanova I, Di Stefano CM, et al. Fetal akinesia in metatropic dysplasia: The combined phenotype of chondrodysplasia and neuropathy? Am J Med Genet A. 2011;155A:2860-4.
80. Haas LF. Luis Morquio (1867-1935). J Neurol Neurosurg Psychiatry. 2002;72:787.
Comments are closed.