Our Dermatol Online. 2014; 5(3): 273-275
DOI:. 10.7241/ourd.20143.68
Date of submission: 16.05.2014 / acceptance: 03.06.2014
Conflicts of interest: None
SUBCUTANEOUS PHAEOMYCOTIC CYST: A CASE REPORT
Archana Shivamurthy1, Shaila Talengala Bhat1, Padmapriya Jaiprakash2
1Department of Pathology, Melaka Manipal Medical College, Manipal University, Manipal, India
2Department of Pathology, Kasturba Medical College, Manipal University, Manipal, India
Corresponding author: Ass. Prof. Archana Shivamurthy e-mail: archana_018@yahoo.co.in
How to cite this article: Shivamurthy A, Bhat ST, Jaiprakash P. Subcutaneous phaeomycotic cyst: a case report. Our Dermatol Online. 2014; 5(3): 273-275.
Abstract
Phaeohyphomycosis refers to infection of tissues by dematiaceous fungi which occur most commonly due to traumatic inoculation of fungi. A host reaction to these fungi can ultimately lead to the formation of a cystic cavity or abscess. Here we present a 71 year old woman who presented with a nodular swelling over the left elbow. A surgical excision was performed. On histopathological examination she was found to have a subcutaneous phaeomycotic cyst..
Key words: phaeohyphomycosis; fungi; cyst; elbow
Introduction
Phaeohyphomycosis refers to a heterogeneous group of mycotic infections that are caused by dematacious fungi [1]. These fungi occur either as soil saprophytes, plant pathogens or contaminants living in the environment, with more than 100 different species [2]. Exophiala and Phialophora species usually cause subcutaneous infection. In tissues they form yeast like cells, pseudohyphae-like elements or hyphae [3]. Phaeohyphomycosis is rare. Subcutaneous infection can manifest as phaeomycotic cyst which commonly occurs in the extremities [3,4]. A male predominance has been noted with majority of patients being more than 30 years of age [4]. Infection usually occurs through traumatic implantation of the fungi into the skin with contaminated vegetable matter, slivers of wood or thorn prick [3,4]. We present a subcutaneous phaeomycotic cyst occurring in a 71 year old woman.
Case Report
A 71 year old woman presented with a slowly progressive swelling over the posterior aspect of the left elbow joint since 6 months. It initially started as a small nodule which then progressed to the present size. It was not associated with pain. There was no obvious history of trauma. On local examination the swelling was about 5×3 cm. A clinical diagnosis of bursitis was rendered, excision biopsy performed and sent for histopathological examination.
Pathological Findings
The biopsy specimen consisted of a skin covered cystic tissue mass which weighed about 44grams and measured 6.5×4.5×3 cm. On cut section a uniloculated cyst was identified, filled with pultaceous material (Fig. 1). On microscopy, the cyst wall was fibrocollagonous and lined by foamy macrophages, necro-inflammatory debris, histiocytes, numerous multinucleate giant cells and chronic inflammatory infiltrate (Fig. 2). Septated pigmented fungal hyphae were identified in the giant cells and extracellularly in H and E stained sections (Fig. 3) and with the help of PAS and GMS stains (Figs. 4 – 6). Constrictions were also noted at few of the septations. The overlying epidermis showed no hyperplasia or ulceration. A diagnosis of subcutaneous phaeomycotic cyst was made based on the above findings. A fungal culture to identify the species could not be performed as the specimen was already preserved in formalin.
 Figure 1. Skin covered cystic tissue mass, inset shows uniloculated cyst on cut section,
|
.jpg) Figure 2. Cyst wall lined by granulation tissue overlying fibrocollagenous wall. [H&E x40]
|
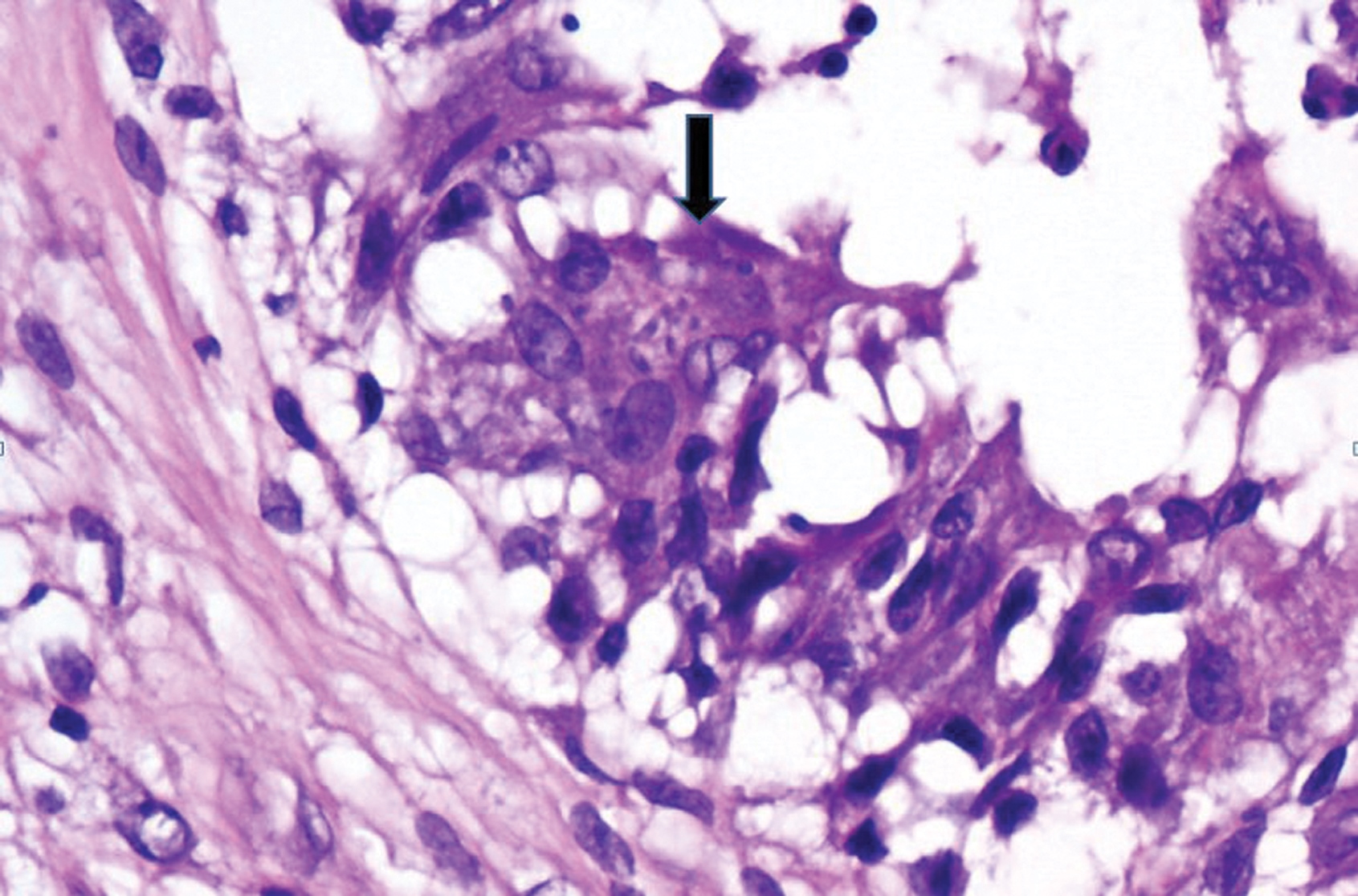 Figure 3. Arrow shows hyphae seen within the multinucleate giant cell. [H&E x400]
|
 Figure 4. PAS stain shows pigmented septate hyphae extracellularly and intracellualrly respectively. [PAS x200]
|
 Figure 5. PAS stain shows pigmented septate hyphae extracellularly and intracellualrly respectively. [PAS x400]
|
 Figure 6. GMS stain shows septate hyphae. [GMS x200]
|
Discussion
Phaeohyphomycosis is a fungal infection caused by dark-walled, pigmented hyphae in tissue and culture. The term ”phaeo” is derived from the greek word phaios which means black or grey [5,6]. Clinical manifestations vary from local skin lesions to invasive and disseminated infections. McGinnis has classified the disease broadly into superficial, subcutaneous and systemic forms. Subcutaneous infections usually occur as solitary lesions; however multifocal lesions have also been described. Common sites include the hand, arm, face, or neck. These infections are being increasingly being detected in immunocompromised patients [1,2,4]. Histopathologically, the lesions are seen as uniloculated pus filled cavities with a fibrous wall. On microscopy granulomas with epitheloid cells, giant cells, lymphocytes and plasma cells are seen. Fungi are septate and seen both intra and extra cellularly [1,5,6]. Often the brown colour of the hypha may not be visible on routine H and E stains. Hence PAS and Fontana-Masson stains can aid in diagnosis. Constriction at the septations can sometimes be observed with Gomori methenamine silver stain [3,6,7]. The overlying epidermis does not show ulceration or hyperplasia as observed in cases of chromomycosis and sporotrichosis which should be considered in the differential diagnosis, nor do phaeomycotic cysts form sinus tracts or contain grains, both of which are typical features of mycetoma [1,3]. Excision of the localized lesion is usually curative. However different antifungal agents have been administered of which itraconazole and amphotericin B appear to be the preferable agents [3,4]. No recurrence has been noted in our patient with a 6 month follow up.
Conclusion
Phaeohyphomycosis should always be considered as one of the differential diagnosis while evaluating cystic lesions in the extremities, especially the exposed areas vulnerable to external trauma. Hyphae may appear hyaline on H and E stains with very light brown pigmentation or no pigment at all. However special stains would always be helpful. Some authors suggest that lowering the condenser of the microscope makes these fungi refractile and visible.
Acknowlegement
We wish to thank all the technical staff of pathology department for their support.
REFERENCES
1. McGinnis MR. Chromoblastomycosis and phaeohyphomycosis: new concepts, diagnosis, and mycology. J Am Acad Dermatol. 1983;8:1-16.
2. Halaby T, Boots H, Vermeulen A, van der Ven A, Beguin H, van Hooff H, et al. Phaeohyphomycosis Caused by Alternaria infectoria in a Renal Transplant Recipient. J Clin Microbiol. 2001;39:1952–5.
3. Manoharan M, Shanmugam N, Veeriyan S. A Rare Case of a Subcutaneous Phaeomycotic Cyst with a Brief Review of Literature. Malays J Med Sci. 2011;18:78–81.
4. Kimura M, Goto A, Furuta T, Satou T, Hashimoto S, Nishimura K. Multifocal Subcutaneous Phaeohyphomycosis Caused by Phialophora verrucosa. Arch Pathol Lab Med. 2003;127:91–3.
5. Ramos AM, de Sales AO, de Andrade MC, Bittencourt JF, Ramos CC. A simple method for detecting subcutaneous phaeohyphomycosis with light-colored fungi. A study of eight cases. Am J Surg Pathol.1995:109–14.
6. Ziefer A, Connor DH. Phaeomycotic cyst. A clinicopathologic study of twenty-five patients. Am J Trop Med Hyg. 1980;29:901-11.
7. Saha R, Rudra S. Phaeomycotic cyst-A case report. J Indian Med Assoc. 2005;103:555–6.
Comments are closed.