Our Dermatol Online. 2011; 5(2): 172-175
DOI:. 10.7241/ourd.20142.42
Date of submission: 22.11.2013 / acceptance: 20.01.2014
Conflicts of interest: None
PLASMOACANTHOMA OF ORAL CAVITY AND PLASMA CELL CHEILITIS: TWO SIDES OF SAME DISORDER “ORAL PLASMA CELL MUCOSITIS” ?
Gayatri Khatri1, Vikram K Mahajan1, Pushpinder S. Chauhan1, Karaninder S. Mehta1, Bal Chander2, Mrinal Gupta1
1Departments of Dermatology, Venereology & Leprosy, Dr. R. P. Govt. Medical College, Kangra (Tanda) -176001 (Himachal Pradesh), India
2Departments of Pathology, Dr. R. P. Govt. Medical College, Kangra (Tanda) -176001 (Himachal Pradesh), India
Corresponding author: Dr. Vikram K. Mahajan e-mail: vkm1@rediffmail.com
How to cite an article: Khatri G, Mahajan VK, Chauhan PS, Mehta KS, Chander B, Gupta M. Plasmoacanthoma of oral cavity and plasma cell cheilitis: two sides of same disorder “oral plasma cell mucositis”? Our Dermatol Online. 2014; 5(2): 172-175.
Abstract
Plasmoacanthoma and plasma cell cheilitis are rare disorders of obscure etiology characterized by a plasma cell infiltrate an 80-year-old woman presented with a verrucous, fleshy, skin colored plaque over lips, gingiva, and the palate and painful swallowing for over a period of 6 months. Histopathology of the lesion showed dense infiltrate of plasma cells. The lesions resolved completely after intralesional triamcinolone acetonide. Another 52-year-old male had progressively enlarging, erosive lesion over vermilion border of lower lip for 6months resembling actinic cheilitis. Histology was diagnostic of plasma cell cheilitis. Treatment with topical clobetasol propionate was effective. Plasma cell cheilitis and plasmoacanthoma perhaps represent a spectrum of oral ”plasma cell mucositis” with plasmoacanthoma being an advanced version of the former.
Key words: Atypical gingivostomatitis; Paraneoplastic acanthosis nigricans; Plasmoacanthoma; Plasma cell cheilitis; Plasma cell mucositis
Introduction
Reactive plasma cell proliferation represents a heterogeneous spectrum of mucocutaneous disorders manifesting clinically with intensive hyperemia, erosions or lobulated warty lesions affecting mostly mucosal/orificial areas [1]. These have been considered to be benign immunologic inflammatory reaction to known (subclinical infection, friction, poor hygiene, trauma, etc.) or unknown stimuli. However, its etiology largely remains speculative. Plasmoacanthoma is a rare benign tumor with plasma cell infiltrate involving the oral mucosa, particularly oral commissures, and perianal areas. Plasma cell cheilitis and plasma cell balanitis of Zoon too have similar dense plasma cell infiltrate. Zoon’s balanitis occurs almost exclusively in uncircumcised men and is speculated to be due to poor hygiene, heat, chronic irritation or Mycobacterium smegmatis infection [2]. Although White et al [3] tried to clarify some of the confusion by grouping together these similar disorders involving different body sites (vulva, buccal mucosa, tongue, palate, epiglottis, and larynx) under the nomenclature of ”plasma cell mucositis”, its exact clinical status remained under studied. Recent reports on co-occurrence of plasma cell mucositis and plasmoacnathoma or intertriginous plasmacytosis of skin, plasma cell orificial mucosistis together with plasmoacanthoma of oral commissures and peri-anum [4,5] has evoked considerable interest for pathogenesis of this rare entity. Cases of plasma cell infiltrate of gums, tongue, oral and labial mucosa have been described mostly under atypical gingivostomatitis, plasma cell gingivostomatitis, plasma cell gingivitis or plasmacytosis mucosae in dental literature but this unusual entity remains under reported in dermatology literature. We feel that both are two sides of one disorder‚ oral plasma cell mucositis’ and should be evaluated as such.
Case Report
Case 1
This 80-year-old woman presented with fleshy, verrucous, skin colored plaque involving the lips and oral cavity. She had feeling of sore mouth and chewing was associated with pain. She was not known to have allergy to any food, beverages, toothpaste, or dentifrices. She was non-smoker, had never consumed alcohol or used nasal snuff/mouth wash, and received no treatment. It had started with a painful ulcer and papules on the lower lip that over a period of 6months had increased in size and number and coalesced to form a verrucous plaque involving the lips, gingiva, palate and buccal mucosa (Fig. 1 A, B). A small ulcer was visible on the right buccal mucosa with shaggy necrotic base, undermined edges and yellowish necrotic slough. She also had swelling, fissuring and crusting of the lips, more so of the lower lip. Cervical and right submandibular lymph nodes were enlarged, firm and mobile. Systemic examination including for ear, nose and throat (ENT) was normal. She was investigated with the provisional diagnosis of paraneoplastic (malignant) acanthosis nigricans. Laboratory work up including complete hemogram, peripheral blood film for abnormal cells, erythrocyte sedimentation rate, serum biochemistry, thyroid and hepato-renal function tests, VDRL, urinalysis were normal. Fine needle aspiration cytology from an enlarged cervical lymph node showed reactive hyperplasia. Chest and skull x-rays, barium meal and follow-through, ultrasonography for abdomen and pelvic organs, and computed tomography scan for thorax showed no abnormality. No organisms were identified in KOH mounts, Giemsa or Gram’s stained tissue smears or on culture of biopsy specimen. Histologic features of ulcerated epidermis with focal neutrophilic exocytosis and dense plasma cell infiltrate in the dermis were suggestive of plasma cell cytoma or multiple myeloma (Fig. 2 A – D). Serum electrophoresis for ‚M’ proteins spike and urine for Bence-Jones proteins were negative. With the final diagnosis of plasmoacanthoma the whole lesion (labial, buccal, palatal) was infiltrated with triamcinolone acetonide (40mg/ml). On follow up after 3weeks there was marked improvement in the lesions (Fig. 1 C, D) and a second dose of intralesional triamcinolone acetonide 40 mg was infiltrated as earlier. No recurrence has occurred during 2-year follow up.
 Figure 1A and B. Fleshy, verrucous plaque over lips and angle of mouth, gingiva, and oral mucosa. Both lips show fissuring and cracking, lower lip is more involved. Note edentulous lower jaw and cobblestone like verrucous surface of gingiva. Upper gingiva and palate had similar lesions. C and D. Three weeks after the first intralesional triamcinolone acetonide injection).
|
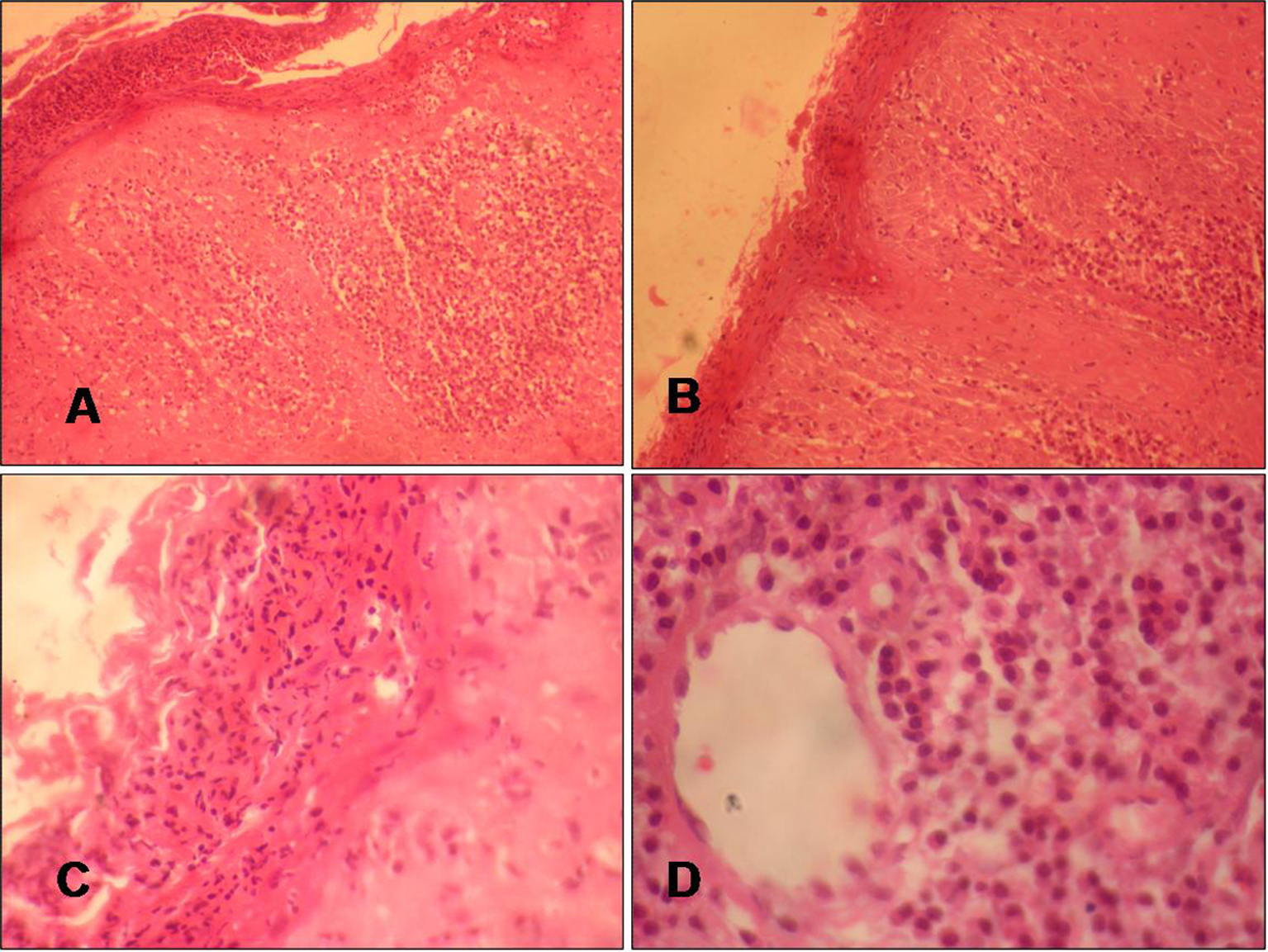 Figure 2A and B. Histology of skin lesion shows focally ulcerated epidermis, prominent rete rigdes, neutrophilic infiltrate in the epidermis and dense plasma cell infiltrate in the dermis (H & E, x10). C and D. Focally ulcerated epidermis with focal neutrophilic exocytosis, dense plasma cell infiltrate in dermis (H & E, x40).
|
Case 2
This 52-year-old male developed a small erosive lesion over lower lip which had progressed to involve the whole lip in 6months. Irritation, burning and occasional bleeding following minor trauma were common symptoms. The erosion was mainly confined to vermilion border of lower lip, showed ill defined to well demarcated and irregular borders, and bright erythematous floor having white slough, crusting and small bleeding at places (Fig. 3A). Regional lymph nodes were not enlarged. He was a smoker for many years but did not consume alcohol or used nasal snuff. He had no allergy to any food, beverages, toothpaste, or dentifrices. He had poor orodental hygiene, gingivitis and few missing teeth. Systemic examination, complete blood counts, serum biochemistry, VDRL, urinalysis and x-ray chest were normal. Lesional biopsy with a clinical diagnosis of actinic cheilitis showed ulcerated epithelial lining, dermal inflammatory infiltrate comprising dense aggregates of plasma cells, few lymphocytes, occasional neutrophils and few macrophages especially in the peri-appendagial and peri-vascular areas suggestive of benign plasma cell cheilitis (Fig. 3B, C). The smooth muscle cells in deeper tissue showed no inflammation. He did not follow up after initial improvement with topical clobetasol propionate 0.05% ointment applied twice daily.
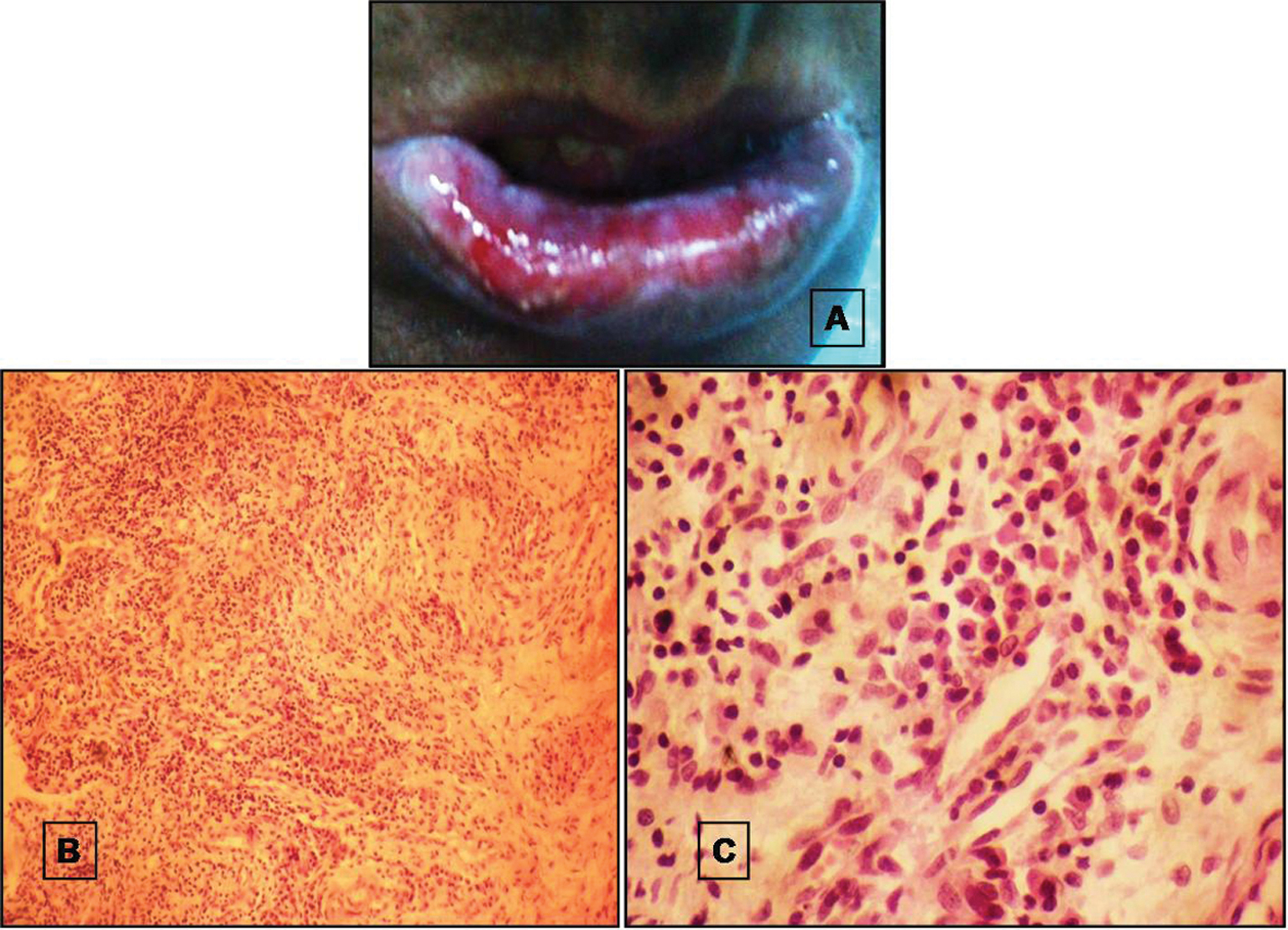 Figure 3A. Superficial, brightly erythematous, poorly demarcated, irregular shaped erosion over vermilion
lower lip having white slough at places. B. Histology of skin lesion shows dense inflammation in the dermis (H&E, x4). C. Chronic inflammatory infiltrate comprises mainly plasma cells along with few lymphocytes (H&E, x40). |
Discussion
Plasmoacanthoma is a verrucous tumour with plasma cell infiltrate involving the oral mucosa, particularly oral commissures. Perianal, periumbilical, or inguinal areas and toe web involvement has been reported [4]. Plasma cell cheilitis is another idiopathic benign inflammatory condition of lips having similar dense plasma cell infiltrate histologically. The usual presenting feature is an asymptomatic patch or plaque of erythema and induration of the lower lip in an elderly person akin to Zoon’s plasma cell balanitis. The significance of trauma/chronic irritation in the pathogenesis of plasma cell cheilitis too has been emphasized from its enhanced incidence in persons habitually chewing tobacco and certain gums, using dentifrices, mint and artificial dentures or snuff intranasally [6]. Similarly, plasmoacanthoma too has been reported following trauma from beak of a bird or insect bites [6]. Candida albicans has been implicated in some cases [4]. However, its association with low levels of serum and secretary IgA remains unsubstantiated [4]. Poor orodental hygiene and associated inflammation seems likely cause in our patients as we could not elicit history of any other preceding trauma/irritation, allergies, tobacco/gum chewing, or use of other dentifrices and causal relationship with smoking will be speculative in case-2. Both plasmoacanthoma and plasma cell cheiltis are entirely benign conditions. Resolution after treatment with intralesional/topical and systemic steroids, griseofulvin, anti-candidial drugs, surgical excision or destructive procedures (Co2 laser ablation, electro-coagulation, cryotherapy) has been observed [1]. Response to intralesional triamcinolone acetonide or topical clobetasol propionate in our patients was notable. Papillomatous plaques of plasmoacanthoma in the oral cavity clinically mimic paraneoplastic acanthosis nigricans (P-AN) on mucous membranes. P-AN is a cutaneous manifestation of underlying malignancy especially adenocarcinoma of the gastrointestinal tract (gastric, gall bladder, pancreas, liver or colorectal adenocarcinoma), lungs, breast, prostate and ovaries [1,6]. P-AN often involves nasolarynx and esophageal mucosa, eyelids and conjunctiva accompanying with extensive cutaneous involvement. Similarly, lower lip plasma cell cheilitis needs be differentiated from actinic cheilitis that may have similar clinical presentation but contrarily therapeutic response to oral antimalarial is usually dramatic. The benign nature of the lesions in our cases was apparent from clinicopathologic features and therapeutic response to intralesional/topical corticosteroids. Moreover, we did not find any laboratory evidence (serum electrophoresis, Bence-Jones proteins in urine) of plasma cell cytoma or multiple myeloma in case-1. Similarly, the histopathology showed no features of erosive lichen planus in case-2. Although seems speculative, we opine that plasma cell cheilitis and plasmoacanthoma perhaps represent a spectrum of the same disease ”the oral plasma cell mucositis”. This appears plausible in view of the reports of co-occurrence of plasma cell mucositis and plasmoacnathoma or intertriginous plasmacytosis of skin, plasma cell orificial mucosistis together with plasmoacanthoma of oral commissures and peri-anum [4,5]; plasmoacanthoma perhaps representing its papillomatous version. However, due to lack of significant number of cases there is paucity of literature on the subject.
REFERENCES
1. James WD, Berger TG, Elston DM. Disorders of the mucous membranes: Plasma cell cheilitis, plasmoacanthoma. In: James WD, Berger TG, Elston DM, editors. Andrews’ Diseases of the Skin, 11th ed. Elsevier Saunders: Philadelphia; 2011. p. 785.
2. Kumar B, Sharma R, Rajagopalan M, Radotra BD. Plasma cell balanitis: Clinical and histopathological features – response to circumcision. Genitourin Med. 1995;71:32-4.
3. White JW Jr, Oslen KD, Banks PM. Plasma cell orificial mucositis. Report of a case and review of the literature. Arch Dermatol. 1986;122:1321-4.
4. Senol M, Ozcan A, Aydin E, Hazneci E, Turan N. Intertriginous plasmacytosis with plasmoacanthoma: Report of a typical case and review of literature. Int J Dermatol. 2008;47:265-8.
5. van de Kerkhof PC, van Baar HM. Co-occurrence of plasma cell orificial mucositis and plasmoacanthoma. Report of a case and review of the literature. Dermatology. 1995;191:53-5.
6. Thami GP, Kanwar AJ, Mohan H. Plasma cell cheilitis. Indian J Dermatol. 1999;44:135-7.
Comments are closed.