Our Dermatol Online. 2013; 4(1): 75-77
DOI: 10.7241/ourd.20131.14
Date of submission: 05.09.2012 / acceptance: 16.10.2012
Conflicts of interest: None
CARCINOMA IN CUTANEOUS LICHEN PLANUS
Rahul Shetty1, Shashank Lamba1, Archana Gulur2, Sapna Patel3, Ashish Kumar Gupta1
1Department of Plastic and Reconstructive Surgery, Christian Medical College, Vellore, India
2Consultant,DHI, Asian Roots, ex consultant Kaya skin care clinic and ESI Hospital, India
3Department of Pathology, Christian Medical College, Vellore, India
Corresponding author: Dr. Rahul Shetty e-mail: rahulplastic@hotmail.com
How to cite an article: Shetty R, Lamba S, Gulur A, Patel S, Gupta AK. Carcinoma in cutaneousLichen Planus. Our Dermatol Online. 2013; 4(1):75-77.
Abstract
Carcinoma occurring in the cutaneous lesions of Lichen Planus though rarely mentioned in literature does occur and should be kept in mind while treating such lesions. We report a 16 year female who developed a squamous cell carcinoma in a long standing verrucous lichen planus in the lower leg. This case is being presented to indicate the possibility of malignant transformation of cutaneous lichen planus to carcinoma, especially in the hypertrophic forms and the need to have an early diagnosis so that it can be treated in the initial stages. A high degree of suspicion should be present whenever we come across a non healing lesion in a patient with lichen planus. A few markers, which may give us a clue for increased chances of malignant transformation in these cases is presented.
Key words: hypertrophic lichen planus; squamous cell carcinoma; reverse sural artery flap
Introduction
Lichen planus is a common papulo-squamous disorder affecting about 1-2% of the population. Lichen planus several forms. It can affect the oral mucosa, skin, nails and genatalia. Cutaneous lichen planus may affect any area but it is often seen on the front of the wrists, lower back, and ankles. Usually the lesions near the ankle are scaly and itchy and form the hypertrophic variant. New lesions occur when the old lesions are clearing. When the lesions cleared they are often replaced by greyish brown discolouration especially in dark skinned individuals. Usually these lesions heal with the conventional treatment. Neoplastic transformation in lichen planus has been described, especially in the oral form of the disease where an estimated 0.3-3% of patients may develop squamous cell carcinoma. Malignancy though uncommon with cutaneous lichen planus has been described in chronic hypertrophic lesions of lichen planus on the legs [3-5].
Case Report
We described a 16-year-old female, who presented to our Department in may 2011 with a non healing ulcer on her left ankle which had been present for approximately one year. She had been treated elsewhere but with no signs of healing. She had been diagnosed as having hypertrophic variant of lichen planus 7 years back. On examination multiple raised pigmented verrucous plaques on dorsum, shins and ankles of both her legs were found. In some lesions there were areas of depigmentation (Fig. 1). A biopsy of one of the hypertrophic plaques showed classic features of a lichen planus. An ulcero proliferative globular growth measuring 6cms x 6cms x 2cms was present on her left heel (Fig. 1). This was restricted in mobility and soft to firm in consistency, tender and there no bleeding on manipulation. The edges of the wound has plaques which suggested it had arised from a lichen planus lesion (Fig. 2). This was being treated by regular dressings. Earlier topical betamathesone and salicylic acid had been tried with only partial response. Both the legs had post inflammatory changes at sites of earlier lesions. The left inguinal lymph were enlarged with a firm consistency. Results of the histological examination of the ulcer biopsy, removed under local anesthesia on 28.05.2011, referred to a diagnosis of squamous cell carcinoma. FNAC of the inguinal lymph nodes suggested metastatic squamous cell carcinoma. A wide local excision (2cms margin) with a reverse sural artery flap cover was done (Fig. 3). Results of the histological examination confirmed malignancy (squamous cell carcinoma) (Fig. 4).
 Figure 1. Lesion on the left heel
|
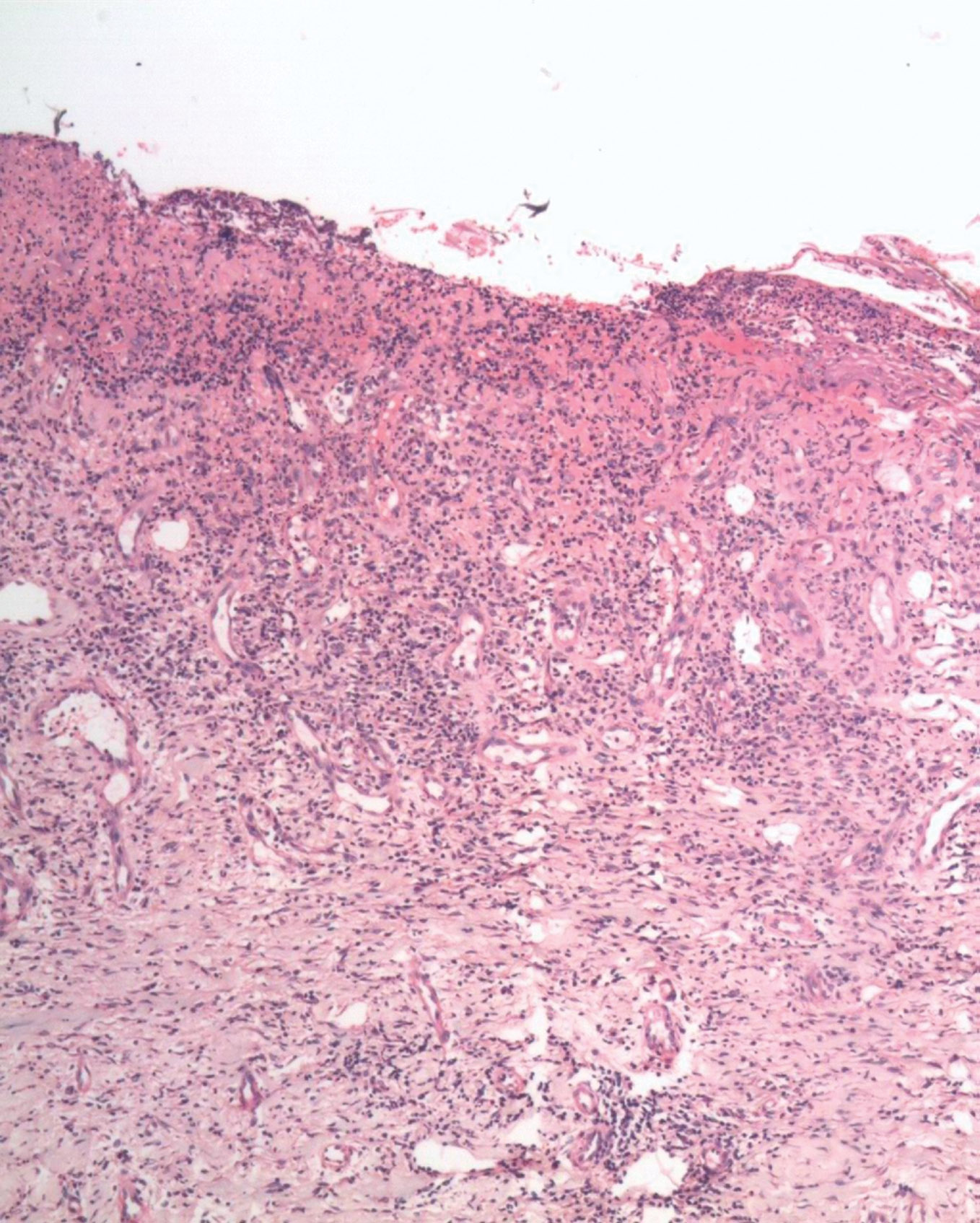 Figure 2. Skin biopsy of plaque over right foot with ulceration, crusting, non specific chronic inflammation
|
 Figure 3. Post operative picture after excision and flap cover
|
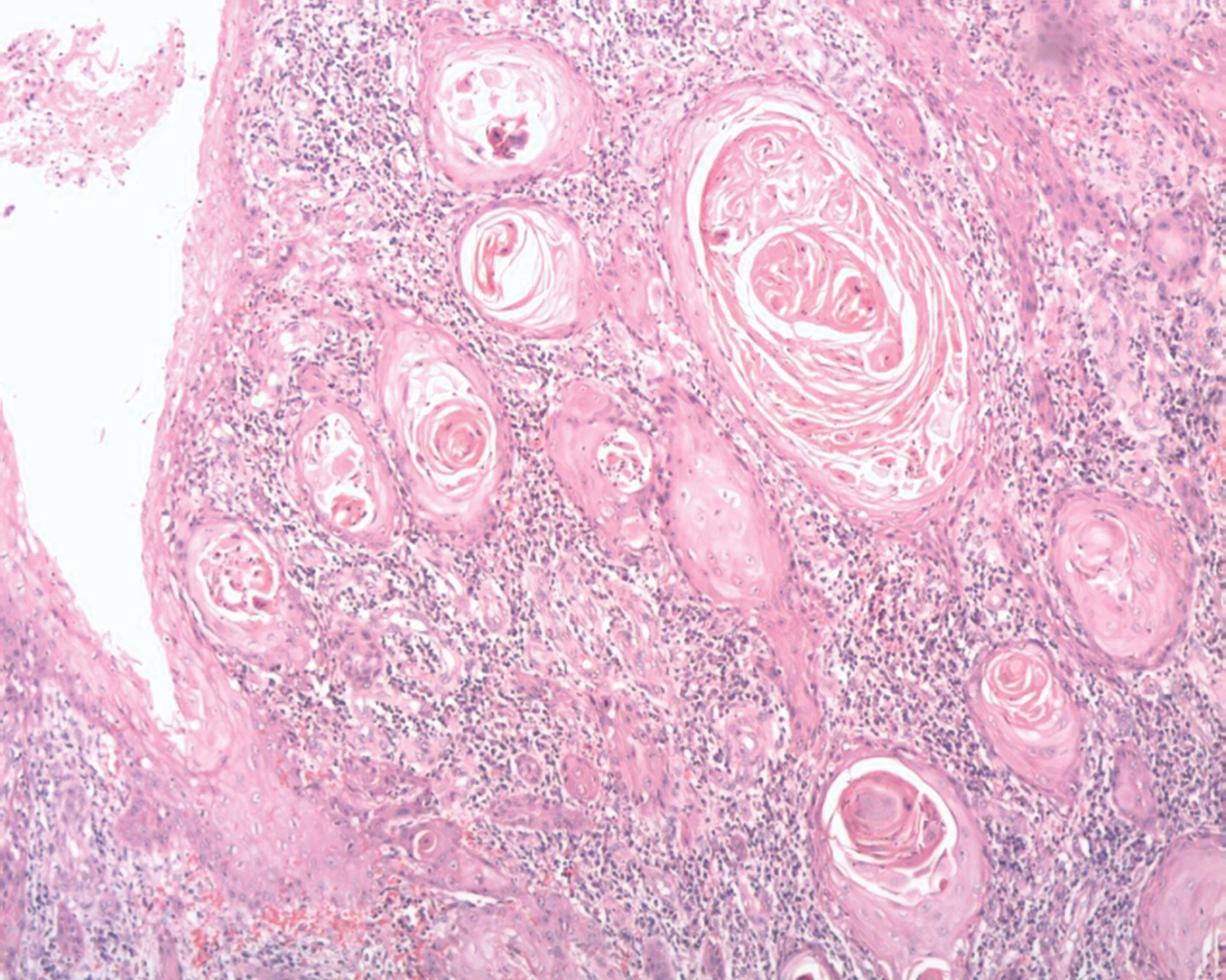 Figure 4. Squamous cell carcinoma
|
Discussion
Most squamous cell carcinoma (scc) is induced by ultraviolet light, while carcinogenic chemicals and human papilloma viruses are also implicated. While an increased risk of the development of carcinoma in oral LP is generally accepted, it is still unclear if there exists a true association between cutaneous lichen planus and Squamous cell carcinoma. Squamous cell carcinoma complicating cutaneous Lichen Planus (LP) has an incidence of 0.4% and most of the reported cases are hypertrophic type [4]. It is essential that one identifies lesions which are likely to transform into carcinoma and a diagnosis is made early. One such marker could be the presence of areas of depigmentation in the lesions. Such lesions have increased probability to turn malignant [5]. Depigmentation was present on our case too. Another common feature of all cases reported so far in literature is the presence of the lesions in the legs (specially the ankles). Hence such cases must be viewed with increased suspicion [6-9]. \
Conclusion
Hypertrophic lichen planus on the legs tend to persist and has a propensity for malignant transformation even in young patients. Therefore non healing ulcers overlying such lesions should be viewed with great suspicion and biopsy performed to rule out squamous cell carcinoma.
REFERENCES
1. Castaño E, López-Ríos F, Alvarez-Fernández JG, Rodríguez-Peralto JL, Iglesias L: Verrucous carcinoma in association with hypertrophic lichen planus. Clin Exp Dermatol. 1997;22:23-5. 2. Hodzic-Avdagic N, Kuhn A, Megahed M, Neumann NJ: Verrucous squamous cell carcinoma developing in hypertrophic lichen planus. Hautarzt. 2004;55:385-7. 3. Singh SK, Saikia UN, Ajith C, Kumar B: Squamous cell carcinoma arising from hypertrophic lichen planus. J Eur Acad Dermatol Venereol. 2006;20:745-6. 4. Sigurgeirsson B, Lindelo¨FB: Lichen planus and malignancy. An epidemiologic study of 2071 patients and a review of the literature. Arch Dermatol. 1991;127:1684-6. 5. Jayaraman M, Janaki VR, Yesudian P: Squamous cell carcinoma arising from hypertrophic lichen planus. Int J Dermatol. 1995;34:70-1. 6. Gawkrodger DJ, Stephenson TJ: Squamous cell carcinoma complicating lichen planus a clinico–pathological study of three cases. Dermatology. 1994;188:36-9. 7. Kaulich M, Jurecka W, Steiner A: Development of squamous epithelial carcinoma on the lower leg in long term verrucous lichen planus.Wien Klin Wochenscr. 2003;115:267-70. 8. Potter B, Fretzin D:Well differentiated epidermoid carcinoma arising in hypertrophic lichedn planus. Arch dermatology. 1996;94:805-6. 9.Manz B, Paasch U, Stierherling M: Squamous cell carcinoma as a complication of long standing hypertrophic lichen planus. Int J Dermatology. 2005;44:773-4.
Comments are closed.