|
|
Porcelain plaques: what is your diagnosis
Aicha Nassiri , Niema Aqil, Hanane Baybay, Fatima Zahra Mernissi
, Niema Aqil, Hanane Baybay, Fatima Zahra Mernissi
Dermatology Departement, Hassan II hospital, Fez, Morocco
Corresponding author: Dr. Aicha Nassiri, E-mail: aichanassiri6@gmail.com
Submission: 07.01.2019; Acceptance: 01.02.2019
DOI:10.7241/ourd.2019e.4
Cite this article: Nassiri A, Aqil N, Baybay H, Mernissi FZ. Porcelain plaques: what is your diagnosis. Our Dermatol Online. 2019;10(e):e4.1-e4.3.
Copyright information
© Our Dermatology Online 2019. No commercial re-use. See rights and permissions. Published by Our Dermatology Online.
Case Report
History
A 12-years-old teenager with no significant pathological antecedants who has moderately itchy whitish lesions in the abdomen and back that have been evolving for one year.
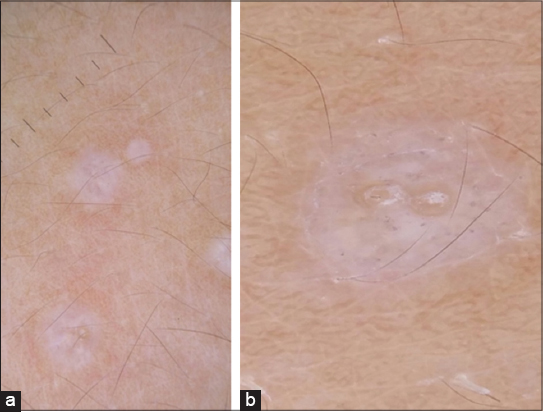
The clinical examination showed whitish and atrophic guttae patches, confluent in shiny plaques in the abdomen and back (Fig 1).
Dermoscopy found bright white patches (Figs. 2a and 2b).
The rest of the clinical examination didn’t show any other anomalies.
Histopathology
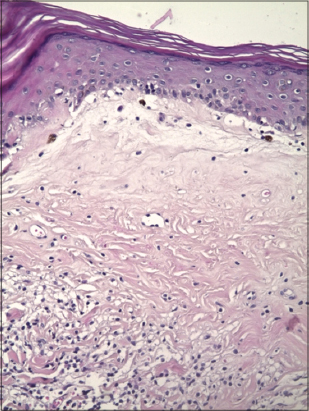
A squamous, atrophic epidermal lining surmounted by a thick hyperkeratosis orthokeratotic compact. The basal membrane is sometimes horizontal, sometimes cut into an arch between irregular epidermal crests (Fig. 3).
It undergoes a continuous basal vacuolization focalising in several places a bullous sub-epidermal detachment of mechanical appearance (Fig. 4). The epidermis without notable cytoarchitectural disorder, rests on a thick edematous fibrohyaline dermal band per places sheltering numerous vascular telangiectasies with hyaline PAS positive wall.
At its level, the coloring of orcein shows that the superficial elastic network is absent and that this band repels the persistent elastic fibers of the middle and deep dermis which are compacted at depth.
This fibrohyaline band also deeply repels discontinuous inflammatory infiltrates mainly lymphohistiocytic mononucleate mixed with some melanophages.
Note the presence at the dermoepidermal junction of a discrete lichenoid focal interface reaction.
The rest of the dermis is fibrous as a whole.
PAS staining does not show mycelium.
What’s your diagnosis?
Answer
Extragenital lichen sclerosus
Skin biopsy whose histopathological examination favored a sclero-atrophic lichen.
First described by Hallopeau in 1887, lichen sclerosus is a rare chronic inflammatory dermatosis that has a predilection for the ano genital area, although extra genital localisation can occur [1]. The majority of reported cases occurred in Caucasian women, however, the disease has been described in other ethnic groups [2]. Both sexes can be affected with a sex ratio of 10/1 for the genitals and 1/1 for the extra genital Lichen sclerosus [3]. Sclerosing lichen can occur at any age, but has a bimodal peak during infancy and after menopause [2]. In our case it happened in a teenager girl.
The pathogenesis of LS is unclear. However, a combination of environmental factors, genetic predisposition, and an autoimmune mechanism have been reported [2].
The genetic theory includes an association with human leukocyte antigen (HLA) class II (HLA-DQ7). Autoimmunity is approved by the increased incidence of autoimmune diseases and autoantibodies [2]. Oyama et al. reported the presence of circulating autoantibodies to the extracellular matrix 1 of the protein (ECM-1) in the serum of approximately 75% of patients with LS [4]. The pathogenicity of the ECM-1 anti-antibody has not yet been substantiated [2].
Clinically, the lesions appear in the form of whitish patches or pearlescent white, atrophic, especially interesting the trunk, the root of the limbs and the folds [3], Pruritus is inconstant, blashko linear and bullous clinical forms have been described [2]. Even though the clinical recognition of well-developed patches of morphea and CLS is usually straightforward, distinguishing them from similar dermatoses and from each other may be quite troublesome when presenting with early (inflammatory) or late (atrophic) lesions or atypical/subtle cases [5,6].
On dermoscopy, Lichen sclerosus is mainly characterized by bright white/white-yellowish patches and yellowish-white keratotic follicular plugs; all these structures display complete specificity for the correspondent dermatosis. Unlike morphea, where the most common dermoscopic findings are “fibrotic beams” [7].
The diagnosis is based on cutaneous histology, which reveals atrophy of the epithelium with horizontalization of the basal layer, follicular hyperkeratosis and especially the presence of an under epithelial band of fibrous or edematous collagen in the superficial dermis without elastic fibers when using orcein staining [8].
The treatment of LSA extra genital is not yet codified, based on very strong class dermocorticoides, tacrolimus, anti-malarial synthesis, retinoids, calcipotriol, UVB.
In severe forms, oral corticosteroids and methotrexate are often required [9].
Statement of Ethics
The patient gave her consent to publication. There are no ethical considerations
REFERENCES
1. Hallopeau H. Leçons clinique sur les maladies cutanées et syphilitique. Union Med. 1887;43:742–7.
2. Abadi R, Ishak R, Abbas O. Hypopigmented papules on the upper trunk and forearm of a young man. Int J Dermatol. 2011;50:1465–6.
3. Kirtschig G. Lichen sclerosus-presentation, diagnosis and management. Dtsch Arztebl Int. 2016;113:337-43.
4. Oyama N, Chan I, Neill SM, Hamada T, South AP, Wessagowit V, et al. Autoantibodies to extracellular matrix protein 1 in lichen sclerosus. Lancet. 2003;362:118–23.
5. Errichetti E1, Lallas A, Apalla Z, Di Stefani A, Stinco G. Dermoscopy of morphea and cutaneous lichen sclerosus:clinicopathological correlation study and comparative analysis. Dermatology. 2017;233:462-70.
6. Hengge UR. Lichen sclerosus;in Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K (eds):Fitzpatrick's Dermatology in General Medicine, ed 8. New York, Mc-Graw-Hill, 2012, pp 702–707.
7. Fistarol SK, Itin PH. Diagnosis and treatment of lichen sclerosus:an update. Am J Clin Dermatol. 2013;14:27-47.
8. Abbas O, Chatrath V, Goldberg LJ. Elastophagocytosis in extragenital lichen sclerosus. J Cutan Pathol. 2010;37:1032–7.
9. Kreuter A, Tigges C, Gaifullina R, Kirschke J, Altmeyer P, Gambichler T. Pulsed high-dose corticosteroids combined with low-dose methotrexate treatment in patients with refractory generalized extragenital lichen sclerosus. Arch Dermatol. 2009;145:1303–8.
Notes
Source of Support: Nil
Conflict of Interest: None declared.
Request permissions
If you wish to reuse any or all of this article please use the e-mail (brzezoo77@yahoo.com) to contact with publisher.
| Related Articles | Search Authors in |
|
|




Comments are closed.